INTRODUCTION
Perihepatitis (hepatic capsular enhancement) is defined as inflammation of the peritoneal capsule of the liver and is associated with various diseases, such as Fitz-Hugh-Curtis syndrome, systemic lupus erythematosus, perforated cholecystitis, perforated hepatic abscess, and tuberculous peritonitis [1-3]. Mycobacterium tuberculosis is a gram-positive bacillus that usually causes pulmonary infection, as well as extra-pulmonary infection. Miliary tuberculosis refers to clinical disease resulting from hematogenous dissemination of M. tuberculosis. Perihepatitis associated with M. tuberculosis is rare, such as in cases of genital tuberculosis and peritoneal tuberculosis [4,5]. We encountered a rare case of miliary tuberculosis accompanying perihepatitis in a 24-year-old woman without sexual experience, who visited the emergency department with the chief complaint of right upper quadrant (RUQ) pain.
CASE REPORT
A 24-year-old virgin woman presented to the emergency department with a 3-day history of RUQ abdominal pain, which worsened with walking, running, and deep breathing. There were no other gastrointestinal symptoms, such as vomiting or diarrhea. The patient also complained of sweating at night, cough, sputum, and weight loss of 10 kg in the previous month. Her sister had developed pulmonary tuberculosis one year ago.
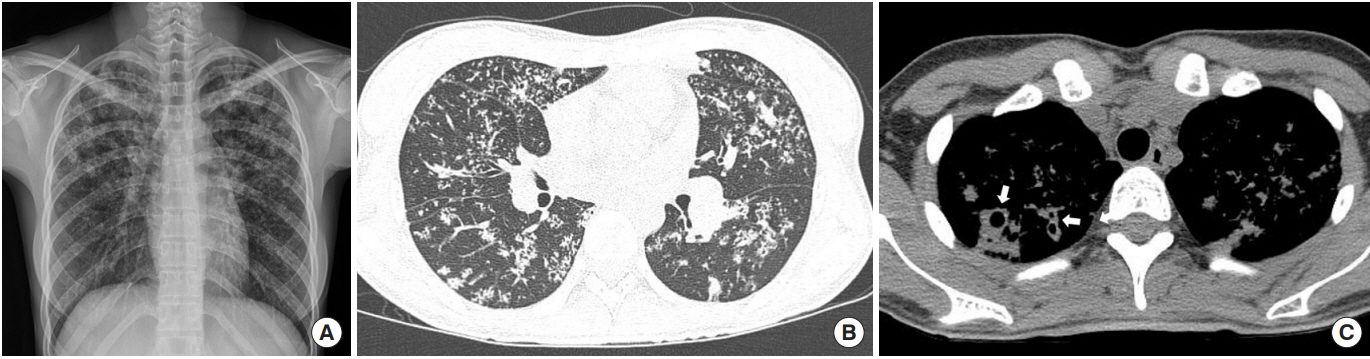
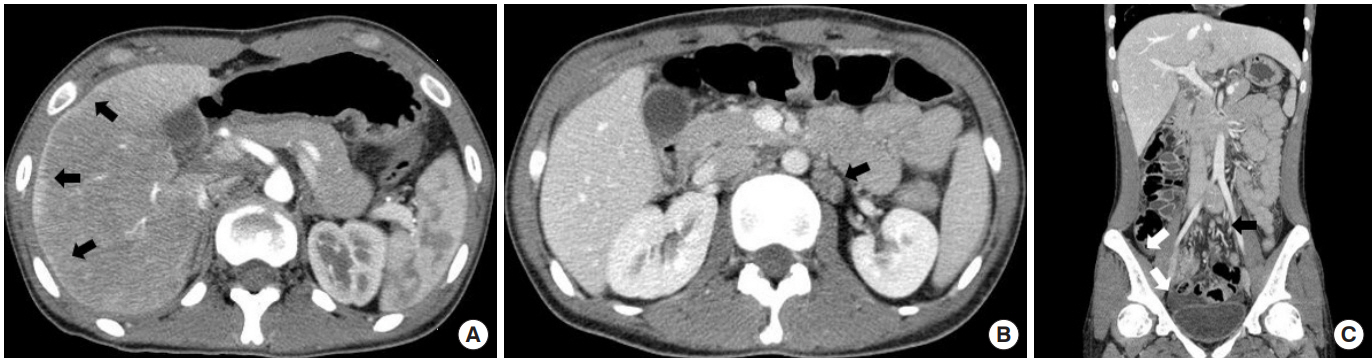
On physical examination, RUQ tenderness was obvious, with right costovertebral angle tenderness and a positive MurphyŌĆÖs sign. We auscultated coarse breath sounds throughout both lungs. Vital signs on admission were as follows: blood pressure, 100/60 mmHg; pulse rate, 100 beats/min; respiratory rate, 24 breaths/min; and body temperature, 38.6┬░C. Blood tests showed a leukocyte count of 10,200/╬╝L (reference; 4,000 to 10,000/╬╝L) and C-reactive protein level of 11.20 mg/dL (reference, <0.3 mg/dL). Acid-fast bacillus culture and polymerase chain reaction hybridization assay of the sputum revealed the presence of M. tuberculosis. Chest radiography showed widely spread small nodular opacities throughout both lung parenchyma (Fig. 1A). Computed tomography (CT) of the chest showed cavitary nodules, centrilobular nodules, branching structures, and consolidation in both lung parenchyma (Fig. 1B, C). Dynamic contrast-enhanced CT of the abdomen revealed diffuse perihepatic capsular enhancement of the liver (Fig. 2A), enlarged paraaortic lymph nodes, small bowel mesentery with internal necrosis (Fig. 2B), and a moderate amount of ascites in the pelvic and peritoneal cavities (Fig. 2C). Anti-tuberculosis therapy with oral isoniazid, rifampicin, ethambutol, pyrazinamide, and pyridoxine was initiated. Eight days after admission, the patient showed an improvement in symptoms and was discharged.
DISCUSSION
We report this case of perihepatitis that was associated with miliary tuberculosis, which occurred in a young immunocompetent woman who did not exhibit pelvic inflammatory disease symptoms.
Perihepatitis is characterized by perihepatic inflammation associated with Fitz-Hugh-Curtis syndrome (which is frequently caused by sexually transmitted microorganisms, such as Chlamydia trachomatis and Neisseria gonorrhoeae), systemic lupus erythematosus, drug side effects, and non-tuberculosis mycobacterial infection [6-9].
Classical miliary tuberculosis is defined as millet-like seeding of M. tuberculosis in the lungs, as evidenced on chest radiographs, which also accounts for up to 20% of all extra-pulmonary tuberculosis [10]. The risk of extra-pulmonary tuberculosis is increased in immunocompromised patients with cirrhosis, human immunodeficiency virus infection and acquired immune deficiency syndrome, diabetes, and cancer. Although there are a few case reports of perihepatitis associated with genital tuberculosis or peritoneal tuberculosis infected with M. tuberculosis, there have been no case reports concerning perihepatitis associated with miliary tuberculosis in the published English literature to date.
CT is the gold standard method for non-invasive diagnosis of perihepatitis, in which hepatic capsule enhancement in the arterial phase can be observed relative to other phases; this enhancement is due to an increased blood flow or inflammation of the hepatic capsule [1,11]. It may also be helpful to demonstrate the ŌĆśviolin string-like adhesionsŌĆÖ observed on laparoscopic examination. Abdominal CT in our case showed enlarged multiple intra-abdominal lymphadenopathy with internal necrosis, which may demonstrate extra-pulmonary spreading of miliary tuberculosis. We propose three potential mechanisms for the pathway of miliary tuberculosis to the subphrenic or perihepatic region, as follows: 1) transphrenic descending spread of M. tuberculosis from the lungs, 2) hematogenous dissemination, and 3) translymphatic spread.
We presented a rare case of perihepatitis associated with miliary tuberculosis, which occurred in a 24-year-old virgin woman with the chief complaint of RUQ abdominal pain. This illustrates that emergency physicians should include miliary tuberculosis in the differential diagnosis of perihepatitis.