Effect of alcohol use on emergency department length of stay among minimally injured patients based on mechanism of injury: multicenter observational study
Article information
Abstract
Objective
This study aimed to evaluate the effect of alcohol use on emergency department (ED) length of stay (LOS) among minimally injured patients by mechanism of injury.
Methods
This was a retrospective study of injury surveillance data for injured patients (except poisoning), aged over 18 years, discharged home from the ED, and treated at seven academic EDs in Korea during 2008 to 2012. Patients were divided into alcohol-related and alcohol-unrelated groups based on self-report. We used multivariable quantile regression models for the analysis and adjusted covariates including age, sex, consciousness status, severity of injury, emergency medical service use, the season, day and time of visit, and hospital. To determine if there were different effects of alcohol use across mechanism of injury, all analyses were stratified by each mechanism.
Results
Among 192,200 patients, 95,807 patients were analyzed. The number of participants in the alcohol-related group was 16,249 (17.0%). In the multivariable quantile regression model, the alcohol-related group had significantly longer ED LOS at the 10th (7 minutes; 95% confidence interval [CI], 6 to 8), 50th (21 minutes; 95% CI, 19 to 23), and 90th (81 minutes; 95% CI, 74 to 87) percentiles when compared to the alcohol-unrelated group. The effect of alcohol use on increased ED LOS was most prominent in motor vehicle injuries.
Conclusion
We found that alcohol use was associated with increased emergency ED LOS. Furthermore, if we limited our attention to the effect of alcohol use on the number of patients, the burden of alcohol use on the ED would have been underestimated.
INTRODUCTION
A significant proportion of alcohol-related patients in the emergency department (ED) are there due to injuries and these patients have different characteristics and outcomes as compared with others [1]. Most studies have evaluated the burden of alcohol use on the ED by investigating the contribution of alcohol use to the number of patients visiting the ED [2,3].
Some evaluations of the effect of alcohol use on patient flow or the usage of resources in the ED have been undertaken; however, various confounding factors, such as age, sex, and injury severity were not considered [4,5]. It is known that the effect of alcohol use on the risk of injury and the severity of injury varied by mechanism of injury (MOI) [6,7]. Similarly, although the effect of alcohol use on injured patient flow may vary by MOI, there are no studies that investigated the different effects of alcohol use on patient flow by MOI.
In this study, we evaluated the effect of alcohol use on patient flow in the ED. We hypothesized that alcohol use would lengthen ED length of stay (LOS), even after adjusting for various factors. In addition, we also hypothesized that the effect of alcohol use on patient flow would vary depending on MOI. We restricted our attention to a population of injured patients treated in the ED without being admitted or transferred, to minimize the confounding effect of the severity of injury and factors related to the hospital (e.g., hospital bed occupancy, boarding time) on ED LOS.
METHODS
Study design and setting
This was a retrospective study of injury surveillance data at seven academic EDs in Korea. Five were urban EDs with 25,000 to 85,000 annual visits, and two were suburban EDs with 15,000 to 20,000 annual visits. Participating hospitals conduct injury surveillance of all injured patients who present to the EDs. Primary surveillance data were collected on a structured registry form by general physicians; the form was then reviewed and revised by emergency physicians and trained study coordinators. We used the data obtained from June 1, 2008 to December 31, 2011. This study was reviewed and approved by the institutional review board of Seoul National University Hospital (1103-152-357). Informed consent was waived and patient information was anonymized prior to analysis.
Selection of participants
Patients over the legal drinking age of 19 years were included. We excluded patients who were admitted or transferred, those who died while in the ED, or visited because of poisoning. We also excluded data in which alcohol use, MOI, and ED LOS contained missing values.
Data collection and processing
Patient data including demographics, characteristics of the visit and injury were collected. Demographics information included age (categories collapsed to 19–29, 30–44, 45–64, and >65 years), sex, and alcohol use. A history of self-reported alcohol use was collected from the patient or their guardian (e.g., patient relative or companion). If alcohol use was identified, the patient was assigned to an alcohol-related group. Visit characteristics included the arrival time to ED, emergency medical service (EMS) use, time of visit (categories collapsed to daytime, 6 a.m. to 6 p.m. or nighttime, 6 p.m. to 6 a.m.), day of visit (categories collapsed to weekday or weekend), season of visit, disposition, and time of departure from ED. Injury characteristics included Glasgow Coma Scale (GCS) at the time of ED visit (categories collapsed to GCS=15 or GCS <15), MOI and severity of injury. Mechanism of injury was classified based on the International Classification of External Causes of Injuries (ICECI) [8]. To facilitate multivariable analysis, we re-categorized the MOI as motor vehicle injury, fall/slip, cut/pierce, collision, and miscellaneous (choking, hanging, drowning, burn with fire, hot liquid, other, and not specified) based on the classifications used in previous studies [6].
To assess the severity of injury, Excess Mortality Ratio-adjusted Injury Severity Score (EMR-ISS) was calculated using International Classification of Diseases 10th edition diagnoses codes [9]. EMR-ISS was categorized as mild (1≤ EMR-ISS ≤8) and moderate to severe (9≤ EMR-ISS) based on a previous study [10]. The primary outcome was ED LOS, which was calculated by subtracting the patient’s ED arrival time from the ED departure time.
Statistical analysis
Descriptive statistics are reported as counts, percentages, medians, and interquartile ranges, as appropriate. Patients’ characteristics were compared between the alcohol-unrelated group and alcohol-related group. Continuous variables were compared using the Wilcoxon rank sum test or Student t-test, and categorical variables were compared using the chi-square test.
The distribution of the ED LOS was highly right-skewed and not distributed normally [11]. Therefore, because standard ordinary least squares regression models may fail to discern the effect of alcohol use on ED LOS, we used quantile regression models for the analysis. Unlike standard least squares regression models, quantile regression models indicate the effect of alcohol use on ED LOS of the middle and both tails of distribution [12]. We used a quantile regression method to estimate covariate effects at 10-percentile intervals from the 10th to 90th percentile of ED LOS. Multivariable quantile regression models were constructed to assess the adjusted effect of alcohol use on ED LOS. We adjusted for the covariates that could have affected EDL LOS including age, sex, injury severity, level of consciousness, EMS use, time of visit, day of visit, season of visit, and hospital. With this approach, the quantile-specific coefficient of alcohol-relation in a quantile regression model shows how the ED LOS at the specific quantile differs between the alcohol-related group and the alcohol-unrelated group while holding other covariates constant. To determine if there were differing effects of alcohol use across MOI, all results were stratified by the MOI.
A two-sided P-value of less than 0.05 was considered statistically significant. Data management and analyses were performed with R ver. 3.24 (available at http://www.r-project.org). Quantile regression models were constructed using the R quantreg package.
RESULTS
The data of 192,200 patients from seven EDs were reviewed; after excluding 96,393 (50.2%) patients, 95,807 (49.8%) eligible patients were analyzed (Fig. 1). Of the eligible patients, 16,249 (17.0%) comprised the alcohol-related group and 79,558 (83.0%) patients comprised the alcohol-unrelated group.
Flow diagram of study patients. DOA, death on arrival; ED, emergency department; LOS, length of stay.
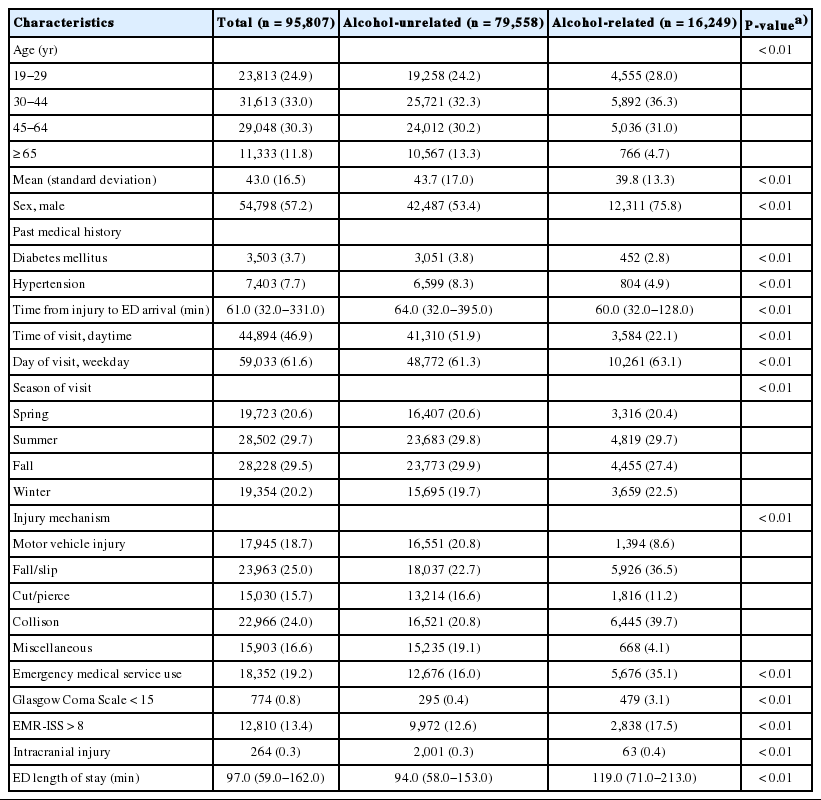
Table 1 shows the demographic characteristics in relation to alcohol use. Young, male patients, using EMS, decreased level of consciousness, and having a moderate-to-severe injury were more likely to be in the alcohol-related group. The median ED LOS of the alcohol-related group was significantly longer than the alcohol-unrelated group. The alcohol-related group also stayed significantly longer in the ED for all MOI (Fig. 2).

Comparison of the emergency department (ED) length of stay (LOS) between the alcohol-unrelated group and alcohol-related group by mechanism of injury. The lower and upper boundaries of each box represent the 25th and 75th percentiles, the bar within each box represents the median, and the whiskers extend to the most extreme observation within 1.5 interquartile range units of the 25th and 75th quartiles. There were significant differences between the alcohol-unrelated group and alcohol-related group in all mechanisms of injury.
Table 2 presents the multivariable quantile regression coefficient estimates of the median ED LOS by MOI. Although level of consciousness, injury severity and EMS use had larger coefficients than alcohol use, alcohol use showed significant positive coefficient estimates across all MOI.
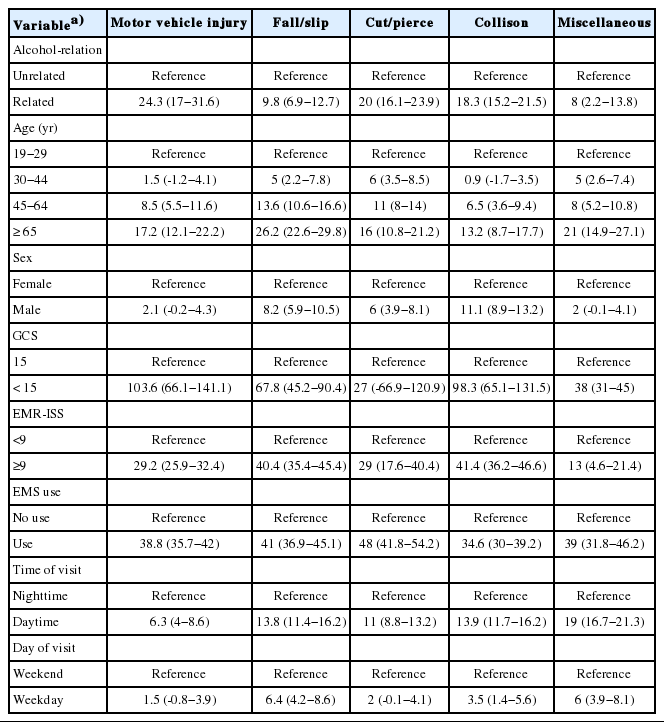
Coefficient estimates and 95% confidence intervals for alcohol-relation at the median of the emergency department length of stay by mechanism of injury
In a univariable quantile regression model, the alcohol-related group had significantly longer ED LOS at the 10th (9 minutes; 95% confidence interval [CI], 8 to 10), 50th (25 minutes; 95% CI, 13 to 27), and 90th (162 minutes; 95% CI, 149 to 175) percentiles compared to the alcohol-unrelated group. In the multivariable quantile regression model, the alcohol-related group had significantly longer ED LOS at the 10th (7 minutes; 95% CI, 6 to 8), 50th (21 minutes; 95% CI, 19 to 23), and 90th (81 minutes; 95% CI, 74 to 87) percentiles compared to the alcohol-unrelated group.
Fig. 3 presents the multivariate quantile regression coefficient estimates of alcohol use by the mechanisms of injury. In each MOI, the estimates at the 10th percentile of the ED LOS were similar, because all estimates were less than 10 minutes regardless of the mechanism of injury. However, the estimates at the 50th to 90th percentiles were substantially different across the mechanisms of injuries. Of all MOI, motor vehicle injury had the largest coefficient estimates in the alcohol-related group. Regardless of MOI, the coefficient estimates of the alcohol-related group indicated that the difference in time between the 50th and 90th percentiles was much greater than the difference between the 10th and 50th percentiles.
DISCUSSION
We found that alcohol use was independently associated with an increase in the ED LOS of minimally injured patients. Alcohol use can affect ED LOS by its association with age, sex, EMS use, time of visit, level of consciousness, and the severity of injury. Although level of consciousness, severity injury, and EMS use were the three most influential factors on ED LOS, alcohol use was associated with significantly longer ED LOS, even after adjustment for those factors.
Previous studies have evaluated the association between alcohol use and ED LOS in injured patients. Using the National Hospital Ambulatory Medical Care Survey (NHAMCS) database, O’Keeffe et al. [4] found that alcohol-related patients had a significantly longer ED LOS than alcohol-unrelated patients. However, they did not consider the confounding factors of age, sex, and the severity of injury. Lee et al. [5] conducted a retrospective study of patients injured in motor vehicle accidents who were treated and discharged from a level I trauma center; it was found that the median ED LOS of alcohol-related patients was longer than that of the alcohol-unrelated group. They included only patients discharged from the ED to minimize the confounding effect of injury severity. However, other confounding factors were not considered in this study and only the patients injured in motor vehicle accidents were included in this study.
We also found that the magnitude of the effect of alcohol use on ED LOS was different across the modes of injury. The effect of alcohol use on ED LOS was most prominent for injuries acquired in motor vehicle accidents. Because motor vehicle-related injuries are known to be the most common cause of spinal injuries in developed countries [13], the possibility of conducting time-consuming tests, such as magnetic resonance imaging on unconscious ED patients might lead to increased ED LOS for these patients. Even if the patient is conscious, these patient may also contribute to an increase in time-consuming tests when they want unnecessary, time-consuming tests which could be covered by their private car insurance [14].
We also found that alcohol use affected the ED LOS differently at various sections of the distribution. In all modes of injury, the difference in the time between the 50th percentile and 90th percentile was much larger than the difference between the 10th and 50th percentile; alcohol use was more influential in patients who have longer stays in the ED.
Various reasons could explain the effect of alcohol use on ED LOS. The effect of alcohol on the level of consciousness is a potential barrier to clinical assessment. In addition, the chance of undergoing more expensive and time-consuming tests, such as imaging and blood tests, are increased in the alcohol-related group [4]. It has also been reported that the alcohol-related individuals are far more likely to be triaged to ED critical care rooms even with minimal injuries [5]. Finally, the alcohol-related group visiting the ED is more likely to be uninsured and lack the means to pay for care, which can lead to longer ED LOS [15].
Many previous studies have evaluated the burden of alcohol on ED crowding by investigating the number of alcohol-related patients in EDs [2,3]. Patient number is a traditional measure of ED crowding and one of the input factors in the conceptual ED crowding model [16]. ED LOS is another prominent measure of ED crowding, and it represents the throughput factor of the conceptual ED crowding model [17]. Our study revealed that alcohol affected ED crowding occurs not only due to an increase in the number of patients but also by negatively affecting the patient flow.
The use of registry data allowed us to study a large number of patients, but also created several limitations. First, we identified the alcohol-related group based on the self-reported use of alcohol. However, self-reported data has proven to be valid information in several studies including in Korea [18,19]. In addition, self-reported drinking could be more inclusive, because blood alcohol concentration could be affected by the amount of time passed between the injury and arrival at the ED [20]. Second, although we enrolled only ED discharge patients, the ED LOS can still be influenced by various factors such as ED occupancy at the time of evaluation or total number of patients in the ED. Because we did not know these values, we tried to control for some of these by including the time, day, and season of the visit, which may have adjusted for some causes of variation. Finally, all participating hospitals were tertiary teaching hospitals in Korea. Therefore, the generalizability of results to other community-based hospitals and other countries is not clear. However, the consistency of findings across four years and seven hospitals supports the effect of alcohol use on ED LOS, which may be applicable to different ED settings.
In conclusion, we report the increased ED LOS among patients who used alcohol. These effects were independent of demographics, visit and injury characteristics, and the severity of the injury. This effect was most visible for ED visits related to motor vehicle injuries. If we only considered the effect of alcohol use on patient number, the burden of alcohol on ED could have been underestimated.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This work was supported by the Emergency Department based Injury In-depth Surveillance funded by Korea Centers for Disease Control and Prevention.
References
Article information Continued
Notes
Capsule Summary
What is already known
Some evaluations of the effect of alcohol use on patient flow in the emergency department (ED) have been undertaken. However, various factors, such as age, sex, injury severity, and mechanism of injury were not considered.
What is new in the current study
Even after adjusting injury severity and other confounding factors, the alcohol-related group had significantly longer ED length of stay compared to the alcohol-unrelated group. The effect of alcohol use on increased ED length of stay was most prominent in motor vehicle injuries.