Sensitivity, specificity, and predictive value of cardiac symptoms assessed by emergency medical services providers in the diagnosis of acute myocardial infarction: a multi-center observational study
Article information
Abstract
Objective
For patients with acute myocardial infarction (AMI), symptoms assessed by emergency medical services (EMS) providers have a critical role in prehospital treatment decisions. The purpose of this study was to evaluate the diagnostic accuracy of EMS provider-assessed cardiac symptoms of AMI.
Methods
Patients transported by EMS to 4 study hospitals from 2008 to 2012 were included. Using EMS and administrative emergency department databases, patients were stratified according to the presence of EMS-assessed cardiac symptoms and emergency department diagnosis of AMI. Cardiac symptoms were defined as chest pain, dyspnea, palpitations, and syncope. Disproportionate stratified sampling was used, and medical records of sampled patients were reviewed to identify an actual diagnosis of AMI. Using inverse probability weighting, verification bias-corrected diagnostic performance was estimated.
Results
Overall, 92,353 patients were enrolled in the study. Of these, 13,971 (15.1%) complained of cardiac symptoms to EMS providers. A total of 775 patients were sampled for hospital record review. The sensitivity, specificity, positive predictive value, and negative predictive value of EMS provider-assessed cardiac symptoms for the final diagnosis of AMI was 73.3% (95% confidence interval [CI], 70.8 to 75.7), 85.3% (95% CI, 85.3 to 85.4), 3.9% (95% CI, 3.6 to 4.2), and 99.7% (95% CI, 99.7 to 99.8), respectively.
Conclusion
We found that EMS provider-assessed cardiac symptoms had moderate sensitivity and high specificity for diagnosis of AMI. EMS policymakers can use these data to evaluate the pertinence of specific prehospital treatment of AMI.
INTRODUCTION
The mortality rate of acute myocardial infarction (AMI) has declined substantially during the past 30 years [1,2]. However, AMI is still a leading cause of death in many countries [3], and the importance of timely treatment is well established [4]. Many AMI patients do not receive timely and proper treatment, and prehospital delay is among the main causes of delayed treatment [5-7]. In prehospital areas, various methods, including assessment via 12-lead electrocardiograms (ECGs), activation of the cardiac catheter laboratory, and fibrinolysis to shorten the time to reperfusion, are used to manage AMI patients [8-13].
Although prehospital 12-lead ECG is the most studied tool and is a class I recommendation for the prehospital management of AMI [8,14], whether a prehospital 12-lead ECG reading is taken or not is based on the symptoms of the patient and is yet to be determined. Therefore, emergency medical services (EMS) provider-assessed symptoms have a critical role in evaluating AMI patients in prehospital settings. When AMI is accurately assessed in the prehospital phase, it is possible to provide optimal prehospital management and rapid transport, select a proper receiving hospital, and ultimately reduce first medical contact to device time in AMI patients [14].
In contrast to many studies about the diagnostic accuracy of hospital physician-assessed cardiac symptoms for AMI [15], the diagnostic accuracy of EMS provider-assessed cardiac symptoms for AMI has not been evaluated in previous studies. We hypothesized that the diagnostic accuracy of EMS provider-assessed cardiac symptoms for AMI would be acceptable and associated with proper management and reduced process times in prehospital and hospital settings. This study aimed to describe the diagnostic accuracy of EMS provider-assessed cardiac symptoms for AMI and to identify the difference in prehospital and hospital processes according to the presence of EMS provider-assessed cardiac symptoms.
METHODS
Study setting
Korea established a single-tiered and fire-based public EMS system in 1995. The emergency hotline number in Korea is 119, and emergency medical technicians (EMTs) are dispatched during emergency calls. Detailed information on the education and training of Korean EMTs has been described previously [16]. EMTs can provide care comparable to that of intermediate EMT level in the US, including intravenous fluid infusion, endotracheal intubation or laryngeal mask airway insertion, and administration of certain medications, including nitroglycerin, under online medical direction [17]. An ambulance runsheet is filled out by EMTs for every ambulance dispatch, and all information is electronically recorded in the servers of the headquarters of the 16 provinces. Since a pilot trial of prehospital 12-lead ECG reading by the National Emergency Management Agency in 2009, EMS providers have acquired prehospital 12-lead ECG readings in some regions in Korea. However, it is not yet a widely accepted method for AMI management during emergencies.
Study design and data collection
This study was a retrospective observational study using an EMS database, administrative databases of participating emergency departments (EDs), and hospital medical records. The records of 4 large tertiary academic EDs located in urban areas with 40,000 to 80,000 annual patients were reviewed. We acquired the EMS database from the National Emergency Management Agency for this study. Using the EMS database from January 1, 2008 to December 31, 2012, we linked the participating hospitals’ administrative data to the EMS database and assessed information on age, sex, visiting date, and visiting time. The hospital medical records of the sampled patients were reviewed by trained researchers. Available ED records, hospital admission records, nursing charts, and coronary angiography reports were reviewed.
Study population
We included patients who visited any of the 4 participating hospitals’ EDs by EMS from January 1, 2008 to December 31, 2012. Patients whose EMS data were not linked to the administrative data were excluded. Using the disproportionate stratified sampling method, we planned to enroll 800 patients for our analysis.
Sampling and weighting
Because patients who had EMS-assessed cardiac symptoms and patients whose final diagnosis was AMI were rare in the EMS database, a disproportionate stratified sample design was used to gain an adequate number of those patients. EMS-assessed cardiac symptoms and a discharge diagnosis of AMI in the administrative database were used for stratification. To gain an evenly distributed sample, the hospital and year of visit were also used for stratification. We planned to sample 10 patients in each stratum for a total of 800 patients. The sampled data were weighted to the probability of selection.
Variables and measurement
Among the 30 predefined categories of symptoms in the EMS database, we defined EMS-assessed cardiac symptoms as chest pain, dyspnea, palpitation, and syncope. Meanwhile, an ED discharge diagnosis of AMI was defined as an International Classification of Diseases 10th revision (ICD-10) code of I21.0 to I21.9 in the administrative ED database.
From the EMS database, we collected data on the patient’s age, sex, symptom to call time, response time, scene time, transport time, hospital arriving time, presenting symptoms, prehospital documented shock (at least 1 event of systolic blood pressure less than 90 mmHg as measured by the EMS), and prehospital management, including oxygen therapy, ECG monitoring, intravenous fluid infusion, nitroglycerin administration, and cardiopulmonary resuscitation (CPR).
From the participating hospital’s administrative database, we collected data regarding patients’ age, sex, hospital arriving time, ICD-10 ED diagnosis, and ED disposition status.
By reviewing hospital medical records, we collected data on the final diagnosis of AMI or not. For AMI patients, we also collected data on the presence of ST segment elevation, cardiogenic shock before reperfusion therapy, performance of CPR before reperfusion therapy, and the type of reperfusion therapy (thrombolysis, percutaneous coronary intervention, or coronary artery bypass grafting). Data on door-to-needle or balloon times were also collected in patients with ST elevation myocardial infarction (STEMI).
Statistical analysis
Descriptive statistics were used to assess the similarity between the study population and the study sample. The characteristics of patients whose final diagnosis was AMI and STEMI were compared according to EMS provider-assessed cardiac symptoms. Values in the study sample were weighted via the reciprocal of the probability of selection in all analyses. Because we planned to compare weighted values according to EMS provider-assessed cardiac symptoms, design-based statistical tests, including Student’s t-test, Wilcoxon rank-sum test, chi-square test, and Fisher exact test, were used as appropriate using a survey package for R software. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) with 95% confidence interval (CI) of each of the EMS-assessed cardiac symptoms as well as all of the EMS-assessed cardiac symptoms combined were calculated for the final diagnosis of AMI. Verification bias-adjusted estimates were calculated by using stratified sampling to weigh results from patients in the EMS database using CompareTests for R software [18-20].
Ethics statement
The study protocol was approved by the Institutional Review Board of the Seoul National University Hospital (1509-120-705). Informed consent was waived by the Institutional Review Board.
RESULTS
Characteristics of the study participants
From January 2008 to December 2012, 121,394 patients who visited the participating hospitals via EMS were identified from the EMS database. Among them, data of 92,353 (76.1%) patients were linked to a participating hospital’s administrative ED database. Although stratified sampling of 800 patients was planned, only 775 patients were sampled because the total number of patients in some strata did not exceed the planned number. The medical records of the sampled 775 patients were reviewed. Among them, 276 patients had a final diagnosis of AMI. Notably, no confirmed AMI was observed in patients who did not have a diagnosis of AMI in the administrative ED database (Fig. 1).

Schematic of data analyses. ED, emergency department; EMS, emergency medical services; EMS Sx+, patients who had EMS provider-assessed cardiac symptoms; ED Dx+, patients diagnosed with AMI in the administrative ED database; ED Dx-, patients who did not have a diagnosis of AMI in the administrative ED database; EMS Sx-, patients who did not have EMS provider-assessed cardiac symptoms; AMI, acute myocardial infarction. a)Hospital and year of visit was also used in stratification.
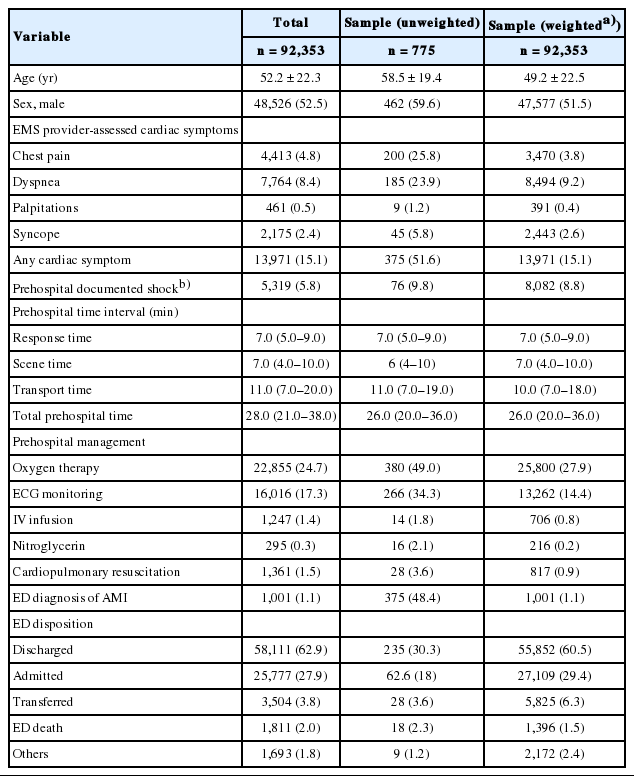
Table 1 shows the baseline characteristics of the study population and sample. Among all patients, 15.1% had any of the EMS provider-assessed cardiac symptoms, and 4.8% had chest pain. The mean age was 52.2 years in the total population, 58.5 years in the unweighted sample, and 49.2 years in the weighted sample. The proportion of men in the total population, unweighted sample, and weighted sample was 52.5%, 59.6%, and 51.5%, respectively. Although baseline characteristics were different between all patients and sampled patients, the weighted values were similar between them.
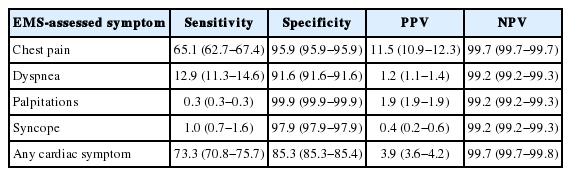
Main outcome
Table 2 shows the sensitivity, specificity, and predictive values of EMS provider-assessed cardiac symptoms for the diagnosis of AMI. The sensitivity and specificity were 73.3% (95% CI, 70.8 to 75.7) and 85.3% (95% CI, 85.3 to 85.4), respectively, for any of the EMS-assessed cardiac symptoms, and 65.1% (95% CI, 62.7 to 67.4) and 95.9% (95% CI, 95.9 to 95.9), respectively, for chest pain. Chest pain was revealed as the most sensitive symptom for diagnosis of AMI, and PPV was also the highest for chest pain (PPV 11.5%; 95% CI, 10.9 to 12.3) (Table 2).
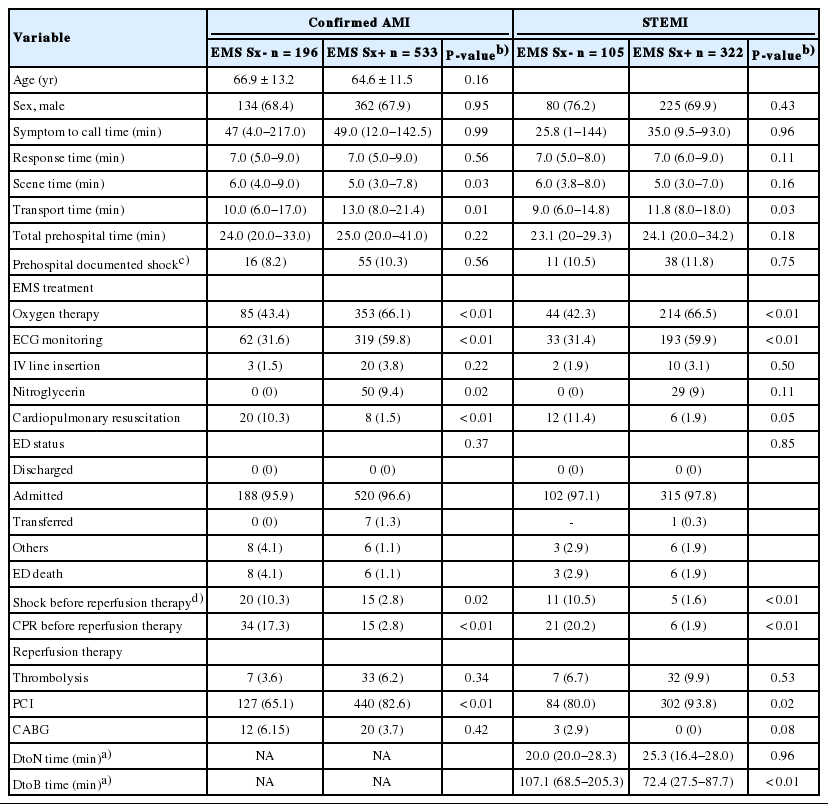
Table 3 shows the prehospital, ED, and hospital characteristics of AMI patients in a weighted sample of EMS-assessed cardiac symptoms. AMI was confirmed in 748 patients (0.8% of total patients). Among all confirmed AMI patients, those whose cardiac symptoms were assessed by EMS had shorter scene time and longer transport time and received more oxygen therapy, ECG monitoring, and nitroglycerine administration than patients who had not. The probability of providing CPR in the prehospital or hospital phase was also lower in patients who had EMS-provider assessed cardiac symptoms than in patients who had not. Although prehospital documented shock was more common in patients who had EMS provider-assessed cardiac symptoms than in patients who had not (10.3% vs. 8.2%), shock in the hospital phase was less common in patients who had EMS provider-assessed cardiac symptoms than patients who had not (2.8% vs. 10.3%). Among STEMI patients, the door-to-balloon time in percutaneous coronary intervention patients was significantly shorter in those who had EMS-assessed cardiac symptoms than in patients who had not (median [interquartile range], 72.4 [27.5 to 87.7] vs. 107.1 [68.5 to 205.3] minutes) (Table 3).
DISCUSSION
Because the timeliness of treatment is critical in AMI patients [4], accurate symptom assessment in the prehospital phase is important. The effectiveness and efficiency of various aspects of prehospital management, including 12-lead ECG readings, oxygen, drugs and fluids, selection of hospital, and prehospital notification, would be improved if symptoms were assessed accurately in the prehospital setting. In this study, we evaluated the diagnostic accuracy of EMS provider-assessed cardiac symptoms for AMI using an EMS database, administrative ED databases, and hospital records. Regardless of individual symptoms, the specificity of EMS-assessed cardiac symptoms was significantly higher than the sensitivity of EMS-assessed cardiac symptoms. This means that these symptoms are more useful at excluding rather than including AMI. For example, if we use chest pain for identifying AMI, a negative result is reliable at reassuring that a patient does not have AMI (NPV 99.7%), and chest pain as an indicator of AMI correctly identifies 96% of patients who do not have AMI (specificity 95.9%). However, the presence of chest pain is poor at identifying AMI (PPV 11.5%), and further investigation is needed to diagnose AMI.
We found that EMS provider-assessed cardiac symptoms had very high NPV. However, because only 0.8% of patients had confirmed AMI, the high NPV of EMS provider-assessed cardiac symptoms was primarily based on the low prevalence of confirmed AMI patients in the EMS database. We also found that the sensitivities of dyspnea, palpitation, and syncope were low. Therefore, the diagnostic value of these symptoms is minimal for identifying AMI.
We found that AMI patients who had EMS provider-assessed cardiac symptoms tend to receive more prehospital management and have low prevalence of shock in the ED phase. Active management in the prehospital setting can be associated with early stabilization of AMI patients [21]. STEMI patients who had EMS provider-assessed cardiac symptoms had higher prevalence of receiving reperfusion therapy and faster reperfusion time intervals than patients who did not. EMS has been reported to be associated with a wide use of acute reperfusion therapies and fast time intervals in AMI patients [6]. Even in EMS users, we found that patients who had EMS provider-assessed cardiac symptoms had a higher proportion of those characteristics than patients who did not.
The mechanism of efficient hospital treatment in patients who had EMS-assessed cardiac symptoms was not directly evaluated in our study. Because patients who had EMS-assessed cardiac symptoms had classic symptoms for AMI, the ease of diagnosis can be associated with efficient treatment in the hospital phase. Other EMS provider activities, including prehospital notification and alerts to ED staff when EMS providers hand over patients, can also be associated with those characteristics. Because prehospital 12-lead ECG was not widely used in our setting, the effect of prehospital 12-lead ECG would be minimal in our study.
To our knowledge, this is the first study to evaluate EMS provider-assessed cardiac symptoms in view of the final diagnosis of AMI. Previously, the concordance of symptoms of myocardial infarction between paramedic and hospital records was evaluated in one study, and they found that the concordance of paramedic prehospital patient care documentation of symptoms was excellent for almost all symptoms, including chest pain [22]. Those findings could suggest that EMS provider-assessed cardiac symptoms could have similar diagnostic accuracy to hospital physician-assessed cardiac symptoms. However, the actual diagnostic accuracy of EMS provider-assessed cardiac symptoms was not evaluated. In one study, the diagnostic accuracy of chest pain assessed by an EMS call center was evaluated [23]. In that study, the overall rate of AMI was 12% in patients who called EMS for chest discomfort, and that level was similar to the PPV of chest pain in our study.
Compared to previous studies, our study has several strengths. First, rather than include only patients who had chest pain or AMI diagnosis, we included and sampled all patients responded by EMS. Therefore, we could estimate all aspects of diagnostic accuracy, including sensitivity, specificity, and predictive values. If we only included patients who had chest pain and AMI diagnosis, the specificity could not be calculated. Second, because we used disproportionate stratified sampling, we captured a substantial proportion of AMI patients in our sample. Because less than 1% of the total patients had AMI, a sample of more than 27,300 patients would be needed to capture 273 confirmed AMI patients, which is the same number of confirmed AMI patients in our study. Although we captured a substantial proportion of AMI patients using disproportionate stratified sampling, we found that baseline characteristics were similar between all patients and weighted values of sample patients (Table 1). Third, because other diagnostic tests, including prehospital 12-lead ECG, are seldom used in Korea, the diagnostic accuracy of EMS provider-assessed cardiac symptoms was minimally influenced by other tests.
EMS provider-assessed symptoms are critical for evaluation and management of AMI patients. The diagnostic accuracy of EMS provider-assessed cardiac symptoms can be used as baseline data for policymakers and quality indicators in prehospital AMI management and AMI education programs for EMS providers. Studies about the association between the diagnostic accuracy of EMS provider-assessed cardiac symptoms, outcomes of AMI patients, and the additional diagnostic value of other tests, including prehospital 12-lead ECG, for the evaluation of AMI in patients with EMS provider-assessed cardiac symptoms would be helpful to evaluate the importance of the EMS system and each EMS intervention in the management of AMI more objectively.
Our study has several limitations. First, it was performed at tertiary hospitals in Korea, and the results may not be generalized to other EMS systems. However, the consistency of findings across five years and four hospitals supports our findings, which may be applicable to different ED settings in these regions. Second, the gold standard of AMI was based on hospital medical review in this study, and there may be some errors. However, many studies on AMI use hospital medical review as the gold standard [24,25], and because this study was retrospective, there are limited ways to identify real AMI. Third, the effect of EMS provider-assessed cardiac symptoms on the outcomes of AMI patients can be caused by the selection of the designated hospital, but those effects could not be evaluated in our study. Fourth, approximately 24% of EMS databases were not linked to ED databases, and this could affect our findings. Moreover, because one-to-one matching was planned, duplicated matching pairs and ambiguous matching pairs were excluded in our study. Fifth, the diagnostic accuracy of the combinations of symptoms was not evaluated in this study. In addition, the characteristics of those symptoms, including severity of pain, were not also evaluated in this study.
In conclusion, each of the EMS provider-assessed cardiac symptoms showed moderate sensitivity, high specificity, low PPV, and very high NPV. We also found that among AMI patients, those who had EMS-assessed cardiac symptoms received more aggressive prehospital management and more efficient in-hospital treatment for AMI. Studies about the association of diagnostic accuracy of EMS provider-assessed cardiac symptoms and outcomes and additional diagnostic value of other tests, including prehospital 12-lead ECG, for the evaluation of AMI in patients with EMS provider-assessed cardiac symptoms are needed.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This study was financially supported by the Woochon Cardio-Neuro-Vascular Research Foundation (2014).
References
Article information Continued
Notes
Capsule Summary
What is already known
In contrast to many studies about the diagnostic accuracy of hospital physician-assessed cardiac symptoms for acute myocardial infarction (AMI), the diagnostic accuracy of emergency medical services (EMS) provider-assessed cardiac symptoms for AMI has not been evaluated in previous studies.
What is new in the current study
The sensitivity of EMS provider-assessed cardiac symptom for the final diagnosis of AMI was 73.3% (95% confidence interval [CI], 70.8 to 75.7), specificity was 85.3% (95% CI, 85.3 to 85.4), positive predictive value was 3.9% (95% CI, 3.6 to 4.2), and negative predictive value was 99.7% (95% CI, 99.7 to 99.8). We found that EMS provider-assessed cardiac symptoms had moderate sensitivity and high specificity for diagnosis of AMI.