Factors affecting patients who attempted suicide in the emergency department due to the prolonged pandemic of COVID-19
Article information
Abstract
Objective
This study examined the characteristics of patients who attempted suicide in the emergency department before and during the COVID-19 pandemic.
Methods
We compared data from patients in the emergency department following suicide attempts between January 2018 and December 2021. The patients were categorized into two groups: “pre–COVID-19” and “during COVID-19” pandemic.
Results
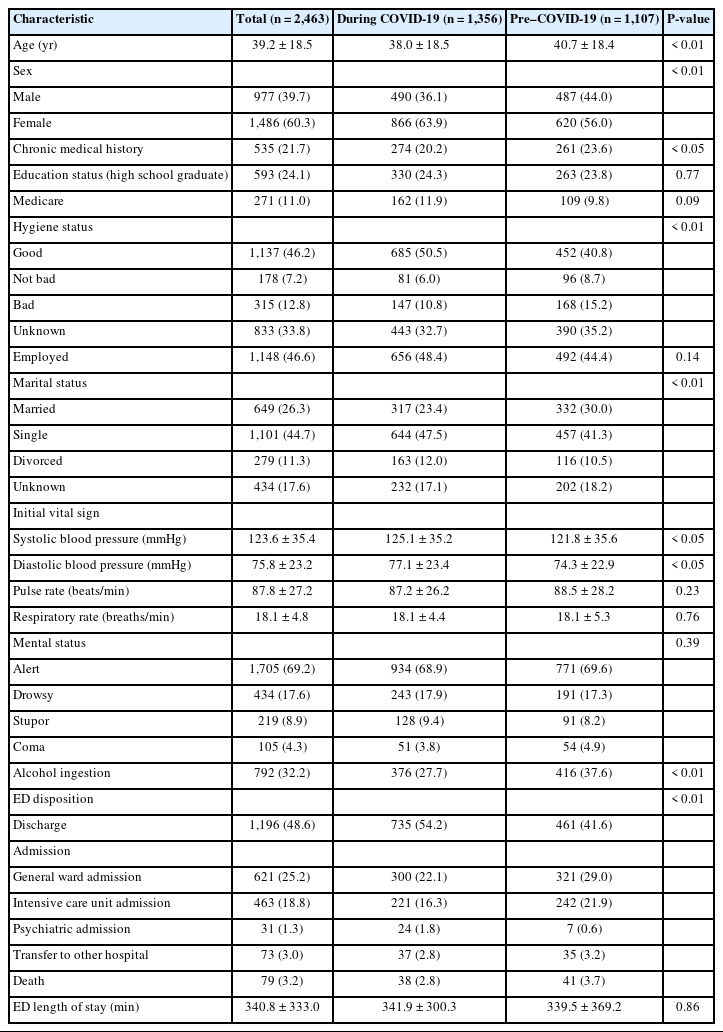
The findings revealed an increasing trend of suicide attempts during the study period. Suicide attempts were reported at 1,107 before the COVID-19 pandemic and 1,356 during the COVID-19 pandemic. Patients who attempted suicide during the COVID-19 pandemic were younger (38.0±18.5 years vs. 40.7±18.4 years, P<0.01), had a smaller proportion of men (36% vs. 44%, P<0.01), and had fewer medical comorbidities (20.2% vs. 23.6%, P<0.05). The group during the COVID-19 pandemic reported better hygiene conditions (50.5% vs. 40.8%, P<0.01) and lower alcohol consumption (27.7% vs. 37.6%, P<0.01). Patients who attempted suicide during the COVID-19 pandemic had higher rates of use of psychiatric medications and previous suicide attempts. The most common reasons for the suicide attempt were unstable psychiatric disorders (38.8%), poor interpersonal relationships (20.5%), and economic difficulties (14.0%). Drug poisoning (44.1%) was the most common method of suicide attempts. Subgroup analysis with patients who attributed their suicide attempts to COVID-19 revealed a higher level of education (30.8%) and employment status (69.2%), with economic difficulties (61.6%) being the primary cause of suicide attempts.
Conclusion
These findings suggest that the prolonged duration of the COVID-19 pandemic and its effects on social and economic factors have influenced suicide attempts.
INTRODUCTION
The COVID-19 pandemic has directly and indirectly affected daily life worldwide. As an unprecedented infectious disease, it has strongly affected aspects of global health that have previously been taken for granted. Mask-wearing has become essential to prevent viral transmission, and most countries have begun social distancing, thus limiting social encounters. It is now natural to track movements using quick response (QR) codes and provide contact information to infected people. Remote office work and online classes for students in schools have become more common. Cultural and performance events with large crowds have largely disappeared, and the forms of essential gatherings, such as weddings and holiday events, have changed significantly.
As these changes in life persist, the “corona blue” phenomenon spreads. As daily life shifted to nonphysical interactions, social isolation was maximized, and the boundaries of each field collapsed, creating emotional instability [1]. Offline economic activity has declined sharply. High unemployment and those who have not adapted to the changes have been directly affected by decreased income, causing anxiety, fear, and depression [2].
Suicide attempts are an important social measure of mental health outcomes and can be associated with economic and cultural status. According to the 2022 Suicide Prevention White Paper released in 2022, the suicide attempt rate in Korea was 24.6 per 100,000 people in 2019, the highest among Organization for Economic Co-operation and Development (OECD) member countries, more than twice the average for OECD countries [3]. After the outbreak of COVID-19, the number of people complaining of depression increased to 20% of the total population due to quarantine measures, such as national lockdown and self-isolation. The symptoms associated with anxiety and depression during the pandemic are not unique to Korea [4].
According to data from the US Centers for Disease Prevention and Control (CDC), 41% of those surveyed said they had experienced pandemic-related psychological abnormalities and a high proportion of respondents (11%) considered suicide. A higher suicide attempt rate during the COVID-19 pandemic was also reported in Japan, according to a 2-year survey conducted between 2020 and 2021 [5].
A Korean database study that predicts and compares suicide attempt rates using a forecasting model reported that the overall number of suicide attempts did not increase; however, the number of suicide attempts by women and young people did [6]. Additionally, studies that focus on changes in mortality rate have analyzed rescue factors of suicide attempters before and during the COVID-19 pandemic [7]. However, studies determining the direct or indirect effects of COVID-19 on suicide attempts after the outbreak are lacking.
This study aimed to compare the characteristics of patients who attempted suicide in the emergency department (ED) before and during the COVID-19 pandemic to examine the factors that affected suicide attempts in the ED during the prolonged COVID-19 pandemic.
METHODS
Ethics statement
This study was approved by the Institutional Review Board of Inha University Hospital (No. 2021-05-023). The requirement for informed consent was waived due to the retrospective nature of the study.
Study design and setting
Inha University Hospital (Incheon, Korea) is a tertiary academic hospital and suicide crisis prevention center in Korea. We conducted a retrospective study using data obtained from medical records and counseling surveys conducted in the ED of our hospital. This ED-based suicide crisis prevention center started in 2017 and has a 24-hour operating system. This suicide crisis prevention center mainly focuses on the initial evaluation, follow-up management, and community connection of suicide attempts among those who visit the ED. Through this, various information, such as the characteristics and demographic information of suicide attempts and the motivation, location, and method of suicide attempts, were recorded and follow-up management was conducted.
Data collection and variables
Patients who had attempted suicide and were seen at the hospital through a regional emergency medical center between January 1, 2018 and December 31, 2021, were included. Among patients who visited the ED, those whose intentionality could not be confirmed due to cardiac arrest or decreased consciousness were excluded. Caregiver counseling was recorded when it was impossible to interview the patient. Medical records, including psychiatric consultation and counseling records, were reviewed retrospectively.
Main outcomes
From January 1, 2018 to December 31, 2021, the medical records of patients who visited the hospital due to suicide attempts and counseling on follow-up management projects for suicide attempts were reviewed retrospectively. Demographic data included age, sex, history of chronic diseases, education, medical insurance, hygiene, employment status, marital status, ED vital signs, consciousness, alcohol consumption, ED exit results, and duration of stay in the ED. Hygiene categories were collected based on psychiatric consultation records. The insurance status and history were collected by checking medical records. Medicare is a vulnerable group that receives state funding. Suicide-related data included psychiatric history, mental illness history, history of previous suicide attempts, reasons for the suicide attempt, and method of suicide attempt. This information was collected from ED records, mental health consultations, and medical charts.
Based on the first reported COVID-19 case in January 2020, patients who were seen in the hospital for suicide attempts from January 1, 2018 to December 31, 2019, were in the “pre–COVID-19 pandemic” group, and those seen from January 1, 2020 to December 31, 2021, were in the “COVID-19 pandemic” group. Additionally, a small group analysis was conducted among patients who reported that suicide attempts during the COVID-19 pandemic were related to COVID-19. Suicide attempts of patients and COVID-19 associations were included only when associations mentioned by patients were recorded in the ED, during hospitalization, or on the psychiatric chart through a review of medical records.
Statistical analysis
Categorical variables were presented as frequency and percentage, and continuous variables were presented as mean±standard deviation. Comparisons between groups were made using the chi-square test for categorical variables and the t-test for continuous variables. All reported P-values were two-sided and statistical significance was set at P<0.05. A multivariate logistic regression analysis was performed to determine the association between COVID-19 suicide attempts and economic difficulties. Multivariate logistic regression analysis adjusted according to age, sex, chronic medical history, education, insurance, employment status, and marital status was performed to calculate the adjusted odds ratio and 95% confidence interval (CI). Stata ver. 16 (Stata Corp) was used for all analyses.
RESULTS
During the study period, 260,662 patients visited our hospital’s ED. Data from 2,463 patients who had attempted suicide were analyzed. Before the COVID-19 pandemic, 1,107 suicide attempts were reported and 1,356 suicide attempts were reported during the COVID-19 pandemic. An increasing trend was observed annually, with 524 cases in 2018, 583 in 2019, 627 in 2020, and 729 in 2021 (Fig. 1).
Demographic characteristics
The mean age was 39.2±18.5 years, and 977 patients (39.7%) were male. During the COVID-19 pandemic, patients who attempted suicide and were evaluated in the ED had a younger age, a lower proportion of men, and fewer past history of diseases such as diabetes and high blood pressure. There were no significant differences in the degree of education, proportion of Medicare users, and employment between the two groups. Regarding hygiene during ED visits, many groups of patients who attempted suicide during the COVID-19 pandemic were in good condition and drank significantly less. There were also differences in marital status and ED results (Table 1).
Psychiatric characteristics
A total of 1,339 patients (54.4%) had a history of psychiatric illness and there were no significant differences between the two groups. The most common psychiatric history was a major depressive disorder. Overall, more than half of the patients who attempted suicide were taking psychiatric medications, and the group who attempted suicide during the COVID-19 pandemic showed more use of psychiatric medications (n=721, 53.2%) and previous suicide attempts (n=376, 27.7%) than before the COVID-19 pandemic (P<0.05). The causes of suicide attempts common in the two groups were issues related to psychiatric disorders (n =956, 38.8%), interpersonal relationships (n =505, 20.5%), economic difficulties (n=345, 14.0%), physical illness (n=106, 4.3%), and other causes not listed (n=551, 22.4%). The methods of suicide attempt were the following: drug poisoning (n=1,086, 44.1%), carbon monoxide poisoning (n=358, 14.5%), drowning (n=45, 1.8%), hanging (n=128, 5.2%), falling (n=42, 1.7%). Suicidal ideation (n=66, 2.7%), self-harm with cutting and stabbing (n=447, 18.1%), and others (n=291, 11.8%) were also reported (Table 2).
Subgroup analysis
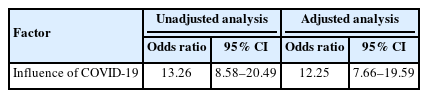
The average age of the patients who mentioned that COVID-19 was a cause of suicide was 42.3±16.9 years, and 42 (40.4%) were male. The proportion of patients graduating from high school or higher was 30.8%, the proportion of patients with a good hygiene status was 61.5%, and the proportion of patients with employment was relatively high at 69.2%. The most common cause of suicide in this group was economic difficulties, with the highest rate at 63.5%. The situation worsened by COVID-19 was also found to be the highest in terms of economic difficulties, with 61.6% (Table 3). Among the patients who visited during the COVID-19 pandemic, those who responded that COVID-19 affected suicide showed a significant association with attempted suicide for economic reasons (adjusted odds ratio, 12.25; 95% CI, 7.66–19.59) (Table 4).
DISCUSSION
This study analyzed more than 2,400 patients who attempted suicide. During the COVID-19 pandemic, the number of suicide attempts steadily increased. The most common cause of suicide was an existing psychiatric disorder, and the most common method of suicide attempt was drug poisoning. Patients who attempted suicide due to COVID-19 were driven primarily by economic reasons that caused the attempt.
We found an increase in the number of suicide attempts during the COVID-19 pandemic. The unexpected spread of COVID-19 and the rising distress in the community have led to a pandemic, which may eventually lead to an increasing trend in reported suicide attempts during the COVID-19 pandemic compared with similar pandemics worldwide. This is consistent with the results of previous studies [8,9]. A Japanese study [10] compared changes in suicide attempt rates by period and reported that there were no significant changes immediately after COVID-19; however, as the disaster situation increased, the suicide attempt rate peaked in the fall of 2020, followed by a downward trend.
According to the World Health Organization (WHO) [8], previous attempts at suicide in normal situations are considered the most important risk factor for suicide among the public. However, a recent systematic review [11] identified domestic conflict and violence, financial or job loss, anxiety, depression, and existing psychiatric conditions as risk factors. The study also found that groups that attempted suicide during the COVID-19 pandemic had higher rates of use of psychiatric medications and previous suicide attempts than those before the COVID-19 pandemic. This can be interpreted as being affected by risk factors for social isolation and stay-at-home rules required during the COVID-19 pandemic.
The increase in employment instability and the decrease in income due to the prolonged COVID-19 pandemic have negatively affected mental health. The economy has stagnated due to limited social and economic activity worldwide, and many people are experiencing a decrease in income and job insecurity [12–14]. Reduced employment during the COVID-19 pandemic reduces psychological well-being and increases depression [15]. In this study, the main cause of attempted suicide was mental disorders, followed by interpersonal relationships in all patients before and after the COVID-19 pandemic. More than 60% of the patients attempted suicide due to the influence of COVID-19. The prolonged COVID-19 pandemic is not expected to adversely affect mental health; however, it is important to specifically confirm which patients who attempted suicide were adversely affected to attempt suicide.
In this study, there was an increase in suicide attempts among patients who were single (47.5% vs. 41.3%) and divorced (12.0% vs. 10.5%) during the pandemic, showing that people without families may have suffered more severely due to the constraints of the pandemic. A previous study reported an increase in the risk of suicide in people living alone or in metropolitan areas during the pandemic, and another study reported an increase in the suicide rate of socially vulnerable people, such as women, people living alone, and minorities [16,17]. Studies have shown that continuous case management suicide crisis prevention centers for suicide reduce suicide reattempts. This is why more active and continuous case management for the vulnerable is needed in the future [18,19].
There are some limitations to this study. First, patients who were seen in the ED primarily for suicide attempts were targeted; if their intention was unknown, they were excluded from the study. Patients who repeatedly visited the hospital were included in the analysis. Generalization is limited because this was a cross-sectional study conducted at a single institution. However, it has the advantage of conducting an in-depth review of the relevance of COVID-19. Second, since this study was a retrospective review study of medical records, information was limited when the patient was in a coma or could not be obtained from a caregiver. Third, if the injury caused by suicide attempts is minor, it can be underestimated compared to before the COVID-19 pandemic. During the COVID-19 pandemic, medical resources have been concentrated in patients with more severe symptoms due to a lack of medical resources. In the case of tertiary academic hospitals such as this research institute, those who attempted suicide with mild symptoms may have had more difficulty accessing medical services. Fourth, in the small group analysis, the association between the patient’s suicide attempt and COVID-19 was limited to those affected only when the patient’s mentioned that COVID-19 was the reason for the suicide attempts was confirmed on the chart. Therefore, there was a limit for unidentified patients.
In conclusion, during the COVID-19 pandemic, the most common cause of suicide was an existing psychiatric disorder, and the most common method of suicide attempt was drug poisoning. Patients who attempted suicide due to COVID-19 were driven by economic reasons. These findings suggest that the prolonged duration of the pandemic and its effects on social and economic factors influence suicide attempts.
Notes
ETHICS STATEMENT
This study was approved by the Institutional Review Board of Inha University Hospital (No. 2021-05-023). The requirement for informed consent was waived due to the retrospective nature of the study.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
This study was supported by the Inha University Research Grant (No. 64608-1, 2021).
AUTHOR CONTRIBUTIONS
Conceptualization: YJL, JHK; Data curation: HK, YJL, AD; Formal analysis: YJL, SK, WKL; Funding acquisition: YJL, SBH; Investigation: YJL, JHK; Methodology: YJL, WKL; Project administration: YJL, SBH; Resources: YJL, JHK; Software: YJL, SK; Supervision: YJL, SBH; Validation: YJL, SK, JHK; Visualization: YJL, SK, WKL; Writing–original draft: HK, YJL; Writing–review & editing: all authors. All authors read and approved the final manuscript.
References
Article information Continued
Notes
Capsule Summary
What is already known
The COVID-19 pandemic is directly and indirectly affecting daily life around the world. It is also having an adverse effect on mental health.
What is new in the current study
This study conducted a small group analysis on patients who attempted suicide due to the influence of COVID-19. The economic reasons for causing suicide were characterized as the biggest. These findings suggest that the long-term persistence of the epidemic and its impact on social and economic factors influenced suicide attempts.