Characteristics of fall-from-height patients: a retrospective comparison of jumpers and fallers using a multi-institutional registry
Article information
Abstract
Objective
Fall from height (FFH) is a major public health problem that can result in severe injury, disability, and death. This study investigated how the characteristics of jumpers and fallers differ.
Methods
This was a retrospective study of FFH patients enrolled in an Emergency Department-based Injury In-depth Surveillance (EDIIS) registry between 2011 and 2018. Depending on whether the injury was intentional, FFH patients who had fallen from a height of at least 1 m were divided into two groups: jumpers and fallers. Patient characteristics, organ damage, and death were compared between the two groups, and factors that significantly affected death were identified using multivariable logistic analysis.
Results
Among 39,419 patients, 1,982 (5.0%) were jumpers. Of the jumpers, 977 (49.3%) were male, while 30,643 (81.9%) of fallers were male. The jumper group had the highest number of individuals in their 20s, with the number decreasing as age increased. In contrast, the number of individuals in the faller group rose until reaching their 50s, after which it declined. More thoracoabdominal, spinal, and brain injuries were found in jumpers. The in-hospital mortality of jumpers and fallers was 832 (42.0%) and 1,268 (3.4%), respectively. Intentionality was a predictor of in-hospital mortality, along with sex, age, and fall height, with an odds ratio of 7.895 (95% confidence interval, 6.746–9.240).
Conclusion
Jumpers and fallers have different epidemiological characteristics, and jumpers experienced a higher degree of injury and mortality than fallers. Differentiated prevention and treatment strategies are needed for jumpers and fallers to reduce mortality in FFH patients.
INTRODUCTION
Fall from height (FFH) is a major cause of death and disability. The World Health Organization (WHO) reported that falls are a major public health problem worldwide as the second leading cause of injury-related death after road traffic injuries [1]. According to the Korean Statistical Information Service (KOSIS), falls account for 9.8% of injury-related deaths [2]. One study of healthcare costs for FFH patients revealed an aggregate expenditure of US$4,421,507 in 1 year, with an average cost of US$15,735 per patient. This financial burden underscores the significant impact of FFH on the healthcare financing system [3]. FFH can be divided into unintentional falls and intentional jumping. In statistics published by the Korean Ministry of Health and Welfare, intentional falls were the second most common method of suicide after hanging, comprising 16.5% of all cases [4]. Worldwide, suicide is the predominant cause of mortality among young individuals and has substantial socioeconomic ramifications [5]. As FFH incidents driven by suicidal intentions are rooted in mental health challenges, it is crucial to have different prevention strategies for jumpers compared to fallers. The mechanism of damage from the force generated by rapid vertical deceleration and direct collision with the ground or an object applies equally to people who have fallen unintentionally or those who have jumped, but the clinical characteristics and patterns of damage differ [6–10]. Due to the high mortality rate of FFH, several autopsy-based studies have been published [11–13]. Studies reporting the clinical characteristics of FFH patients in the medical field have focused primarily on accidental falls, as this accounts for the majority of FFH cases [3,14–16]. Some studies have also compared jumpers and fallers; however, these studies are not representative because they included only a small number of jumpers [6,10,17,18].
In this study, we aimed to compare the characteristics of jumpers and fallers using a multi-institutional registry and to determine factors that affect the prognosis of FFH patients in the emergency department (ED).
METHODS
Ethics statement
This study was approved by the Institutional Review Board of Severance Hospital (No. 4-2019-0692). The requirement for informed consent was waived due to the retrospective nature of the study. All data were completely anonymous.
Study design and data source
This retrospective, observational, cohort study used data from the Emergency Department-based Injury In-depth Surveillance (EDIIS) registry between 2011 and 2018) of the Korea Disease Control and Prevention Agency (KDCA). Twenty-three institutions participated in this surveillance survey. Trained researchers from each institution collected the clinical information of injured patients who presented to the ED. KDCA provided continuous education programs for researchers to manage the quality of the data, performed a qualitative assessment of each institution's data, and provided periodic feedback.
Study population and data collection
Our study included patients aged 10 years or older who fell from a height of 1 m or more. Patients were divided into two groups according to intention: jumpers and fallers. Patients who injured themselves unintentionally were categorized as fallers, while those who were injured due to self-harm or suicide attempts were designated as jumpers. Incidents involving homicide, violence, or intentions that remained unknown were excluded from this study.
The following variables were reviewed in the current study: sex, age, height of fall, type of insurance, mode of ED arrival, date and time of ED arrival, place where the injury occurred, alcohol drinking, ED treatment results, in-hospital mortality, and trauma-related diagnoses. Patients were divided into 10-year age groups to determine incidence according to age. Fall height was classified as 1 to 4 m and ≥4 m. Insurance types were categorized as National Health Insurance, Medicaid, and other. Seasons were defined based on the arrival date at the ED as follows: spring (March–May), summer (June–August), autumn (September–November), and winter (December–February). The mode of ED arrival was divided into emergency medical service (EMS), private ambulance, and other. The place where injuries occurred was classified as factory, residential area, nature, public or commercial area, road, farm, sports facility, school, hospital, or other. Alcohol consumption was assessed through history taking or blood ethanol level analysis and categorized as yes, no, or unknown. Death on arrival and expiration in the ED were considered in-hospital mortality. Diagnoses were reported in accordance with the International Classification of Diseases, 10th Revision (ICD-10). We investigated the patient's primary diagnosis and 2nd to10th diagnoses and identified the injured organs using the following codes: epidural hemorrhage (S06.4), subdural hemorrhage (S06.5), subarachnoid hemorrhage (S06.6), intracranial hemorrhage (S06.8), pneumothorax (S27.0, S27.2), hemothorax (S27.1, S27.2), flail chest (S22.5), liver injury (S36.1), spleen injury (S36.0), kidney injury (S37.0), hollow viscous organ injury (S36.3, S36.4, S36.5, S36.6), aorta injury (S25.0, S35.0), cervical spine fracture (S12.0, S12.1, S12.2, S12.7), thoracic spine fracture (S22.0, S22.1), lumbar spine and pelvis fracture (S32), upper extremity fracture (S42, S52, S62), and lower extremity fracture (S72, S82, S92).
Statistical analysis
We compared the demographic characteristics, treatment outcomes, and injured organs between the jumper and faller groups. Categorical variables are presented as numbers and percentages, and continuous variables are presented as means and standard deviations. The chi-square test or Fisher exact probability test and independent sample t-test were used for analysis. Multivariable logistic regression analysis was performed to identify factors that influenced in-hospital mortality. Variables with significant differences between the death and survival groups (P<0.1) were selected as confounding variables. Statistical analyses were conducted using SAS ver. 9.4 (SAS Inc). Statistical significance was set at a two-tailed P<0.05.
RESULTS
Among the 2,143,189 patients registered in the EDIIS registry from 2011 to 2018, 645,308 (30.1%) presented to the ED due to a fall (Fig. 1). After excluding 584,562 patients who had fallen from less than 1 m in height and 3,433 patients whose fall height was unknown, 57,313 patients were determined to have FFH. Of these, 39,419 patients were included in the study after excluding 17,192 patients under the age of 10 years and 702 patients with unknown intent. The numbers of jumpers and fallers were 1,982 (5.0%) and 37,437 (95.0%), respectively.
General characteristics
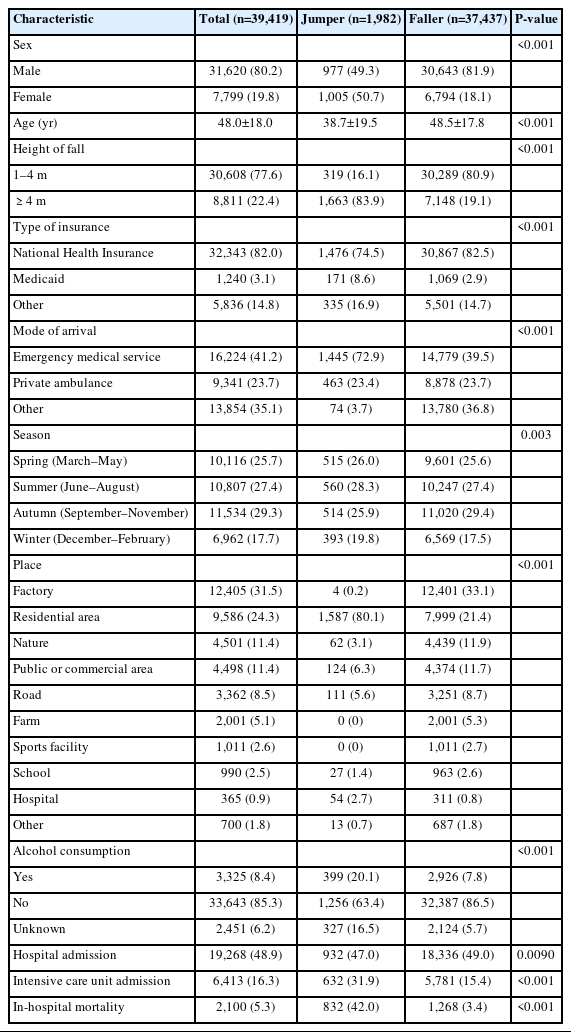
Of the jumpers, 977 (49.3%) were male, while 30,643 fallers (81.9%) were male (Table 1). The mean±standard deviation age of the jumper group was 38.7±19.5 years, which was younger than the faller group (48.5±17.8 years, P<0.001). In the jumper group, 1,663 (83.9%) had fallen from a height of 4 m or more, whereas only 7,148 (19.1%) of those in the faller group had fallen from such a height (P<0.001). The frequency of EMS use was 1,445 (72.9%) in jumpers and 14,779 (39.5%) in fallers (P<0.001). In the jumper group, the place of fall occurrence was predominantly in the residential area (n=1,587, 80.1%), while most FFH occurred in the factory setting (n=12,401, 33.1%) in the faller group. Alcohol consumption was higher in the jumper group than in the faller group (399 [20.1%] vs. 2,926 [7.8%], P<0.001). Unknown alcohol levels were also higher in the jumper group (327 [16.5%] vs. 2,124 [5.7%], P<0.001). In-hospital mortality in the jumper group was 832 (42.0%) compared with 1,268 (3.4%) in the faller group (P<0.001).
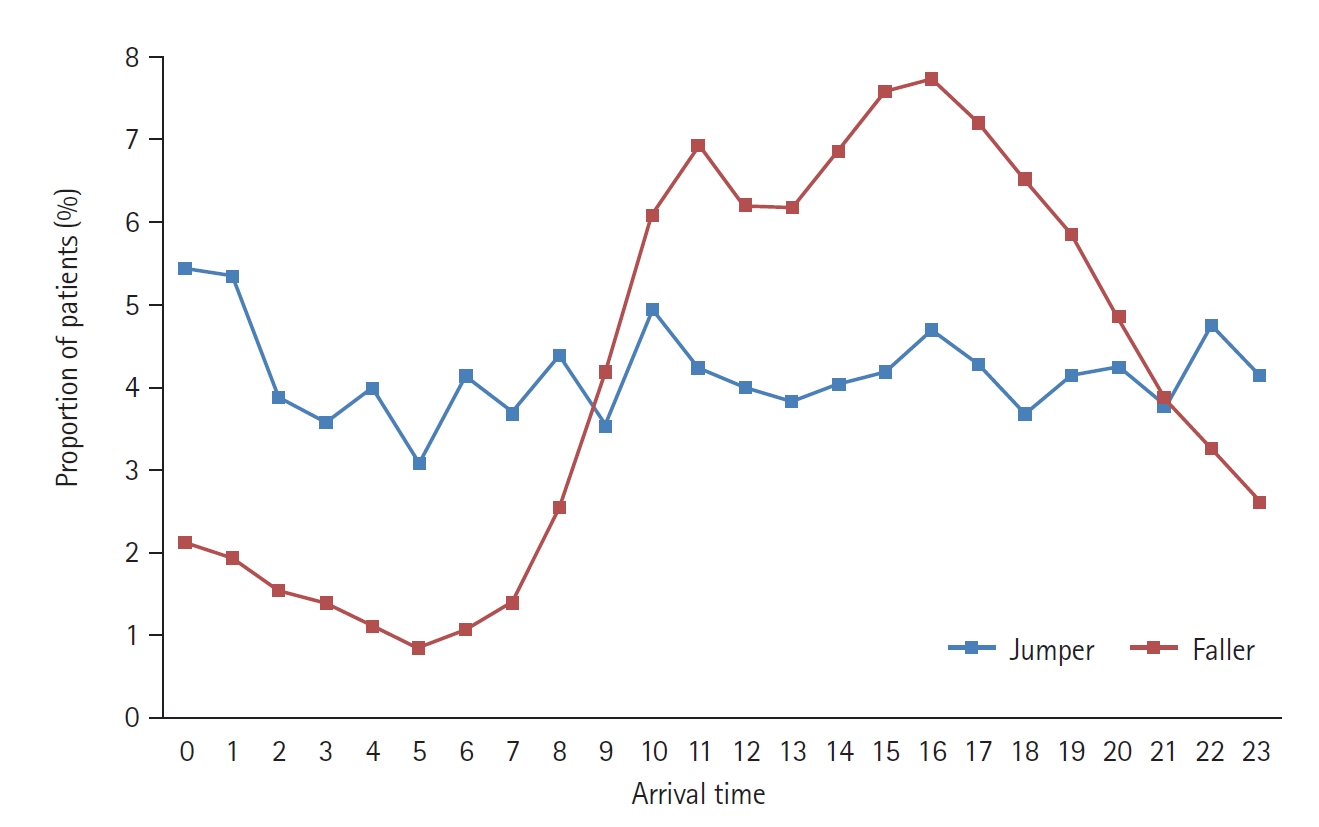
Age and time distribution
The age distribution of each group was analyzed according to sex (Fig. 2). In the jumper group, the largest number of individuals was in their 20s, with the prevalence decreasing by age. There was no meaningful difference in distribution according to sex in the jumper group. In fallers, the incidence of females was evenly distributed across all age groups, whereas the incidence of falls increased in men until their 50s and then decreased. Fig. 3 shows the distribution of visits per hour. Jumpers presented to the ED most frequently between 0:00 and 2:00 AM and in a relatively uniform manner in the remaining hours of the day, whereas fallers were more likely to present between 10:00 AM and 7:00 PM.
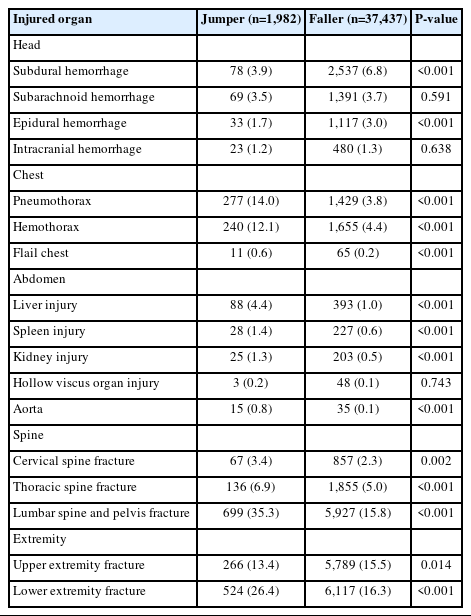
Injured organs
A comparison of injured organs between the two groups is presented in Table 2. The incidence of severe head injuries, such as epidural and subdural hemorrhages, was higher in fallers. The incidence of subarachnoid and intracranial hemorrhages did not differ between the two groups. Chest injuries such as pneumothorax, hemothorax, and flail chest occurred more frequently in the jumper group. Intra-abdominal organs (liver, spleen, and kidneys) were more likely to be injured in the jumper group than in the faller group. The incidence of aorta and spine injuries was significantly higher in the jumper group. Upper extremity injuries were more frequent in fallers, but lower extremity injuries were more common in jumpers (524 [26.4%] vs. 6,117 [16.3%], P<0.001).
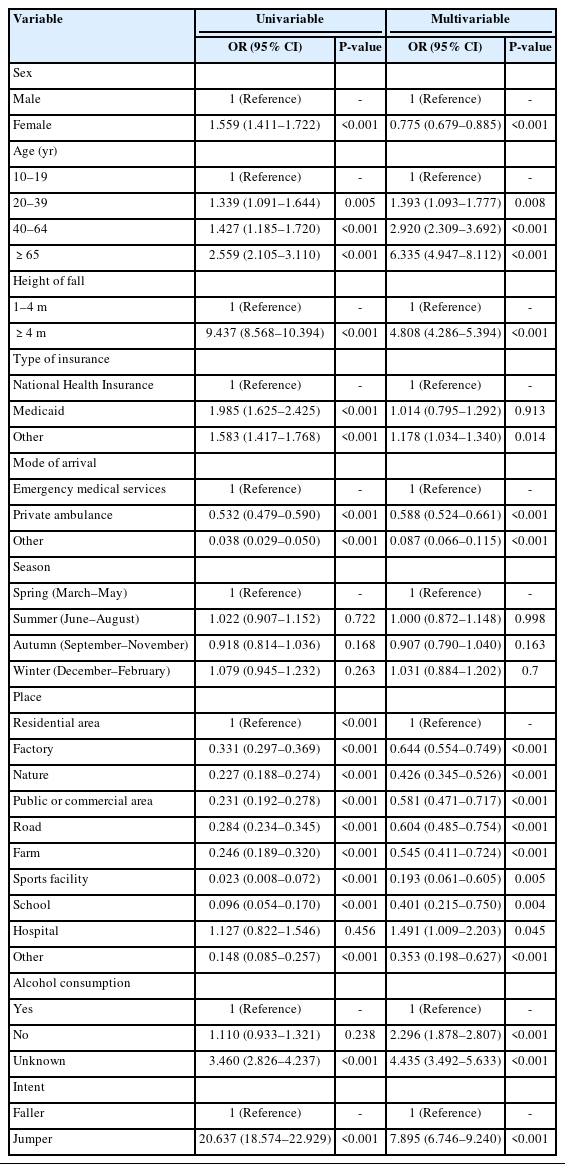
Prognostic factors of in-hospital mortality
Table 3 shows the results of the multivariable regression analysis used to identify factors that affect in-hospital mortality in FFH patients. The female to male odds ratio for in-hospital mortality was low, at 0.775 (95% confidence interval [CI], 0.679–0.885; P<0.001). Age was determined to be a factor, with the mortality rate increasing with age. Fall height and intentionality were significantly associated with in-hospital mortality with an odds ratio of 4.808 (95% CI, 4.286–5.394) and 7.895 (95% CI, 6.746–9.240), respectively.
DISCUSSION
Trauma due to FFH is a major challenge for society because it results in multiple severe injuries, permanent disability, and high mortality. Understanding the clinical characteristics and injury patterns of FFH patients can help in the emergency treatment of these patients, and their epidemiological characteristics are valuable basic data for establishing prevention strategies. This study is meaningful because it presents representative clinical features of jumpers based on analyses of a relatively large number of patients from a multi-institutional registry. From an epidemiological perspective, jumpers and fallers had different sex and age distributions. There was also a significant difference in the severity of injury and mortality between the two groups.
According to the Korean White Paper on Suicide Prevention [4], published in 2022, the most common means of suicide after hanging are falling and gas poisoning. There are differences in the preferred means of suicide according to age group. In 2022, 35.7% of adolescent suicide patients died from falls, while 17.4% of elderly patients died from falls. This study also confirmed that the frequency of jumping was high among young people and rapidly decreased with age in both sexes. Whether a fall victim has attempted suicide may not be immediately ascertainable when they first present at the ED. The results of this study suggest that serious injuries and suicide attempts should be suspected in young FFH patients. In addition, considering differences in the means used to attempt suicide by age, more effective policies for suicide prevention can be established. In particular, when implementing a suicide prevention project for falls, targeting the younger generation will lead to more effective suicide reduction [19].
Patients who had fallen unintentionally were predominantly male, and the distribution by age was highest among those in their 50s. Most accidents tended to occur in factories during the daytime, suggesting that most falls occurred while working at heights. Globally, FFH is the leading cause of fatal injuries in construction workers [20]. Along with an aging society, the average age of construction workers is also increasing [21,22]. According to the US Bureau of Labor Statistics, the average age of construction workers in 2022 was 42.5 years [23]. The average age in Korea is higher than this; according to an investigation by the Korean Ministry of Employment and Labor, it was 53.1 years old in 2022 [24]. Older construction workers are generally more prone to work-related injuries. Indeed, physical decline, reduced coordination, and slow reaction times can increase the chances of accidents, musculoskeletal injuries, and falls in older construction workers [22]. Safety education, use of protective equipment, and compliance with safety guidelines should be conducted considering the increasing age of construction workers [25,26].
More thoracoabdominal organ and spinal injuries occurred in jumpers than in fallers. This is consistent with existing studies in that jumpers typically fall from greater heights and exhibit higher severity and mortality rates [27,28]. However, brain injuries were more frequent in patients who accidentally fell than in jumpers. While this outcome might appear surprising, other studies have similarly reported fewer head injuries among jumpers [29,30]. This should be interpreted with caution because we studied only those patients who were transferred to the hospital. It has been noted in previous studies that patients who land on their heads tend not to arrive at the hospital alive [31,32]. Another notable injury pattern was that jumpers displayed a higher incidence of lower extremity fractures than fallers. This finding aligns with those of previous studies that compared skeletal injuries between jumpers and fallers, emphasizing that jumpers frequently first contact the landing surface with their feet [6,7,27].
We confirmed that fall height, age, and suicidal intent were major determinants of death. This is consistent with the results of previous studies on the determinants of death in fall patients [33,34]. Fall height is a major factor that influences vertical deceleration injury patterns, with studies suggesting 6 or 7.5 m as the height of a fatal fall [35–38]. Jumpers tended to fall from a greater height than fallers, but even after adjusting for fall height, suicide intent remained a significant factor in mortality. Our registry only investigated fall height based on a height of 4 m; therefore, the effect of height on death may not have been adequately examined. However, previous studies have suggested that suicide attempts are a significant independent factor of death in fall patients [18,33]. This suggests that the difference in the risk of death between jumpers and fallers could be due not only to the height of the fall, but also to other factors such as use of protective gear or alcohol or drugs. Furthermore, a study conducted by Faggiani et al. [39] revealed that 76.9% of jumpers had received a diagnosis of a psychiatric disorder (mainly major depressive disorder and bipolar disorder) prior to the incident, and psychiatric illness played a role in extended hospitalization and prolonged stays in the intensive care unit. These underlying psychiatric conditions, coupled with the socioeconomic disadvantages experienced by jumpers, are influential factors that could potentially increase mortality rates. These elements must be considered when devising suicide prevention initiatives related to FFH.
This study has several limitations. First, patients with unknown intentions were excluded. The exclusion of severely ill patients whose intent could not be ascertained because they were unconscious or dead may have influenced the results. Second, patients who could not undergo diagnostic imaging due to an unstable condition or death at the time of arrival at the ED were omitted from the analyses of organ and spinal injuries.
In conclusion, jumpers and fallers had distinct epidemiological characteristics, with jumpers having a higher degree of injury and mortality than fallers. Understanding the characteristics of FFH patients by dividing them into jumpers and fallers could serve as a basis for effective preventive and clinical actions and optimizing hospital treatment.
Notes
Author contributions
Conceptualization: all authors; Data curation: MJK; Formal analysis: JYH, MJK; Funding acquisition: MJK, JHL; Visualization: JYH, MJK; Writing–original draft: JJ, JYH, MJK; Writing–review & editing: all authors. All authors read and approved the final version of the manuscript.
Conflicts of interest
The authors have are no conflicts of interest to declare.
Funding
This study was supported by the Korea Disease Control and Prevention Agency (KDCA) and by a faculty research grant from Yonsei University College of Medicine (No. 6-2021-0246).
Data availability
Data analyzed in this study are available from the corresponding author upon reasonable request.
References
Article information Continued
Notes
Capsule Summary
What is already known
Fall from height is a major trauma leading to serious disability and death.
What is new in the current study
Jumpers and fallers exhibit distinct epidemiological characteristics and severity. Additionally, intentionality, along with sex, age, and fall height, are independent predictors of mortality.