AbstractObjectiveEspecially in emergency departments (EDs), a lack of internal medicine (IM) residents in charge causes difficulties in medical care and ED overcrowding. Thus, protocols without IM residents in EDs is needed. This study aimed to investigate changes in medical care when emergency medicine residents replaced the roles of IM residents.
MethodsThis study was conducted at a single-site ED of a university medical center. The study group contained patients admitted to the IM department between September and December 2015, during which IM residents were absent in the ED. The control group contained patients admitted to the IM department between September and December 2014, during which IM residents were present in the ED. Changes in medical care between the presence and absence of IM residents in the ED were studied by comparing admission rates from the ED, length of ED stay, duration of hospitalization, and concordance of diagnoses between admission and discharge by the IM department.
ResultsThe study group contained 2,341 patients; the control group contained 2,215 patients. Admission rates from the ED increased by 53.4% (95% confidence interval [CI], P<0.001); lengths of stay decreased by 15.1% (95% CI, P<0.001); and durations of hospitalization in the pulmonology department decreased by 38.4% (95% CI, P=0.001). Concordance of diagnoses between admission and discharge decreased by 14.2% in the cardiology department (95% CI, P=0.021).
INTRODUCTIONIn compliance with the Ministry of Health and WelfareŌĆÖs policy of Korea, resident quotas have been cut down to balance them with the number of residents who pass the National Examination for Medical Practitioners since 2013. Additionally, the special act for medical residents implemented in December 2015 has reduced the hours of training per week to 88 hours, limited the maximum hours of continuous training to 36 hours, and guaranteed at least 10 hours of break while on on-call duties. This has created a temporary employment gap in the treatment of inpatients in teaching hospitals [1]. Moreover, the number of internal medicine residents in Korea has been decreasing for various reasons. According to statistics provided by the Korean Hospital Association, the application rate for internal medicine reached 150% in 2004, and then decreased to 139% in 2010, 109% in 2014, and 92.2% in 2015. The recruitment rate of internal medicine residents was 85% in the first half of 2015 [2]. Teaching hospitals outside of the capital area are having even greater difficulties recruiting internal medicine residents, and there are inevitable setbacks in the treatment of inpatients.
Typically, notification and confirmation from senior residents or faculty is necessary for admission or discharge of internal medicine patients in Korean teaching hospitals. In case of absence of internal medicine physicians, a protocol for admission or discharge that can be used in emergency departments must be developed to overcome these situations. In the absence of internal medicine physicians, it is up to emergency medicine physicians to decide whether a patient should be hospitalized or not, and research is lacking regarding how this may affect emergency treatment.
In this present study, protocols for admission or discharge with the absence of internal medicine physicians in the emergency department were developed and applied. Then, emergency treatment results before and after applying the protocol were compared.
METHODSStudy subjectsStudy groupThe present study involved patients who visited the emergency department of a university hospital. To make comparisons between the cases with or without internal medicine physicians present in the emergency department, the patients with internal medicine disorders (or supposed disorders) who visited the emergency department in the absence of internal medicine physicians between September 1, 2015 and December 31, 2015 were designated as the study group. Internal medicine physicians were present in the emergency department during the day (between 7:30 a.m. and 6:00 p.m. on weekdays, and between 7:30 a.m. to 1:00 p.m. on Saturday). Therefore, patients who visited the emergency department between 6:00 p.m. and 7:30 a.m. of the following day during weekdays, between 1:00 p.m. on Saturday and 7:30 a.m. on Monday, and between 7:30 a.m. and 7:30 p.m. on the following day during holidays were recruited. The number of emergency medicine specialists did not change in the study group compared to the control group, but the number of residents increased by one in the study group. There were no changes in the number of other personnel, such as nurses and emergency medical technicians.
Control groupIn 2014, internal medicine physicians were always present in the emergency department. The control group included patients with internal medicine disorders (or supposed disorders) who visited the emergency department during the same period as the control patients in order to minimize differences between the two groups. They visited the emergency department in the same time period as the study group between September 1, 2014 and December 31, 2014. Patients who were transferred to other hospitals from this hospital or voluntarily left the hospital were excluded.
Treatment protocol for patients in the emergency department in the absence of internal medicine physiciansAfter being examined by an emergency medicine physician, patients submitted a hospitalization form. If an emergency medicine physician decided that the patient needed emergency treatment, he/she contacted an internal medicine specialist from a relevant department (Fig. 1). Internal medicine physicians were placed on duty in the hospital wards and intensive care unit so that they could start treating patients immediately upon their admission and provide continuous treatment.
Protocol for admission in the emergency department in the presence of internal medicine physiciansWhen patients arrived at the emergency department, they were first examined by an emergency medicine physician. When the emergency medicine physician decided that the patient needed internal medical intervention or admission to the internal medicine department, the emergency medicine physician called an internal medicine resident. After examining the patient, the internal medicine resident notified the internal medicine staff of the relevant department. Then, the internal medicine staff decided whether the patient needed hospitalization or emergency intervention. If the patient did not need any internal medical intervention, he/she was discharged (Fig. 2).
Outcome measuredThis study retrospectively looked at the differences in hospitalization rates, lengths of stay in the emergency department, and diagnosis at the time of admission and discharge with or without the internal medicine physician present using patient medical records. We defined concordance rate as a percentage of concordance of diagnosis between admission and discharge.
The hospitalization rates in the internal medicine department and its divisions were expressed as percentages. If patients were treated in multiple departments at the same time, emergency medicine physicians or third-year (or higher) medical residents reviewed the patientsŌĆÖ medical records and determined the major department. The length of stay in the emergency department was determined as the duration from the patient visiting and leaving the emergency department. The hospitalization rate (%) was calculated as (the number of inpatients/the number of patients examined)├Ś100.
Transferred patients and patients who voluntarily left the hospital were not included in the study. In addition, to assess the accuracy of diagnoses given by the internal medicine physicians and emergency medicine physicians, the diagnoses upon leaving the emergency department and at the end of hospitalization were compared, and their concordance rates were studied.
Statistical analysisThe SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA) was used for analysis. The chi-square test was used for the hospitalization rates and diagnosis concordance rates. Fisher exact test was used for an expected frequency of less than 5 and number of cells greater than 25%. An independent samples t-test was used for the length of stay in the emergency department and duration of hospitalization. A Mann-Whitney U-test was performed for the lengths of stay in the emergency department and durations of hospitalization that were not normally distributed based on the Shapiro-Wilk test. All values were expressed as mean┬▒standard deviations. The confidence interval was set at 95%. The level of significance was set at P<0.05.
RESULTSCharacteristics of both the study and control groupsThe number of patients who visited the emergency department during the study period in 2015 was 11,497. Of these, 253 patients voluntarily left the hospital, and 56 were transferred. Of the remaining 11,188 patients, 2,215 patients (19.8%) examined for internal medicine diseases were assigned to the study group (Fig. 3).
The number of patients who visited the emergency department during the study period in 2014 was 11,821. Of these, 211 patients voluntarily left the hospital, and 33 were transferred. Of the remaining 11,577 patients, 2,341 patients (20.2%) examined for internal medicine diseases were assigned to the control group (Fig. 4). No significant differences in the number of patients, age, and gender were found between the control and study groups (Table 1).
The number of patients who visited the emergency department during the day in 2014 and 2015 was 10,128 and 9,736, respectively. Among these, patients who voluntarily left or were transferred were excluded. In 2014 and 2015, 2,119 and 2,142 patients were examined for internal medicine diseases during the day, respectively, and no significant differences were found in the patientsŌĆÖ age and gender (P>0.05).
The study group had a greater number of patients admitted to the gastroenterology, cardiology, pulmonology, and endocrinology departments compared to the control group. No significant differences were found in the number of patients in admitted to other departments (Table 2).
Comparison of hospitalization rates with or without internal medicine physiciansThe hospitalization rate was 23.8% in the control group and 36.5% in the study group, signifying a 53.4% increase in the study group compared to the control group (P<0.01). An increase in hospitalization rates was the most significant for endocrinology, followed by infectious diseases, cardiology, pulmonology, and gastroenterology (Table 3). No significant changes in hospitalization rates were observed for nephrology, hemato-oncology, and rheumatology (Table 3).
The rates of hospitalization to the general wards and intensive care unit were 5.5% and 18.4% in the control group, and 9.2% and 27.3% in the study group, respectively. The hospitalization rates were significantly increased by 67.3% and 48.4% in the study group compared to the control group, respectively (P<0.01) (Table 3).
There was no significant difference in the hospitalization rates between the patients who visited the emergency department during the day time in 2014 and 2015, and their hospitalization rates were 43.0% and 42.9%, respectively (P=0.975).
Comparison in lengths of stay in the emergency department with or without internal medicine physiciansThe length of stay in the emergency department was 125.2┬▒113.4 minutes in the study group and 147.5┬▒152.5 minutes in the control group, showing a significant difference of 22.3 minutes (15.1%). The length of stay was shortest for cardiology (100.4┬▒57.1 minutes), and longest for hemato-oncology (168.3┬▒99.1 minutes). The decrease in length of stay was the greatest in for nephrology (24%), followed by endocrinology, rheumatology, and gastroenterology (Table 4).
The length of stay significantly decreased for patients in the intensive care unit, patients in the general wards, and patients discharged from the emergency department (Table 4). For the patients in the intensive care unit, the length of stay significantly decreased in the gastroenterology and the nephrology groups. For patients in the general wards, the lengths of stay significantly decreased in the gastroenterology, cardiology, pulmonology, nephrology, and hemato-oncology groups (Table 4). For discharged patients, the length of stay in the emergency department significantly decreased in gastroenterology only (Table 4).
There was no significant difference in the length of stay between the patients who visited the emergency department in the daytime in 2014 and 2015, and their lengths of stay were 161.5┬▒96.8 and 160.9┬▒97.1 minutes, respectively (P=0.826).
Comparison of duration of hospitalization with or without an internal medicine physician in emergency departmentThe mean duration of hospitalization was 7.5┬▒8.4 days in the study group, which was reduced by 27.2% compared to the control group (Table 5). The duration of hospitalization was especially significantly reduced in the cardiology and pulmonology departments. The duration of hospitalization in the intensive care unit was significantly reduced by 36.4%. No significant reduction by the type of department was observed in the case of the intensive care unit. The duration of hospitalization in general wards was 6.8┬▒6.7 days, which was reduced by 23.6% compared to the control group. The duration of hospitalization was significantly reduced for pulmonology only (Table 5).
There was no significant difference in the duration of hospitalization between the patients who the visited emergency department during the day in 2014 and 2015, and their hospitalization durations were 10.4┬▒11.4 and 9.8┬▒9.81 days, respectively (P= 0.250).
Comparison of the concordance rates of diagnoses at the time of admission and dischargeNo significant differences in the concordance rates of diagnoses at the time of both admission and discharge were found between the control and study groups (Table 6). The concordance rate for patients hospitalized in the cardiology department was 69.5%, signifying a 14.2% reduction compared to the control group. The concordance rate for patients hospitalized in the pulmonology department was 99.3%, signifying a 7.6% increase compared to the control group (Table 6).
DISCUSSIONA shortage of internal medicine physicians is a common phenomenon in general hospitals. Thus, the protocol for admission covering the absence of internal medicine physicians is required and the implementation of such treatment protocols that can effectively proceed with treatments in the absence of internal medicine physicians may reduce the length of stay and prevent crowding in emergency departments. According to the annual emergency medicine statistics report released by the National Emergency Medical Center in 2015, 14.8% of the patients who visited emergency departments were internal medicine patients. In this study, a significant proportion of patients (19.8% to 20.2%) who visited the emergency department were internal medicine patients. However, due to the shortage of internal medicine physicians, it is highly likely that internal medicine physicians will no longer be working in emergency departments in the future. Thus, we must make changes in existing treatment protocols without negatively affecting patient examination and treatment in emergency departments. With previous protocols, there were no significant changes in lengths of stay, hospitalization rates, and durations of hospitalization during the day time in 2014 and 2015. However, we found significant changes with the new protocol in 2015. Thus, we can assume that this protocol affects the emergency department positively.
McCoy et al. [3] reported a reduction in both lengths of stay in the emergency department and durations of hospitalization without an increase in admission rates into intensive care units when emergency department physicians performed the roles of internal medicine physicians in the emergency department. However, while the length of stay was reduced by only 13.6% in their study, it was reduced by 34.0% in this study. In the study by McCoy et al. [3], the mean length of stay in the emergency department for inpatients of the intensive care unit was 374 minutes, much longer compared to the time observed in the present study (178.6 minutes). Protocols in the absence of internal medicine physicians may be more effective in hospitals that have enough empty beds in intensive care units and general wards, and therefore, the patients do not have to stay for extended periods in the emergency department. In this study, the existing internal medicine treatment protocol excluding the internal medicine physicians was used in the emergency department to overcome the shortage of internal medicine physicians. Positive results were observed.
Emergency department crowding has been reported to negatively affect patients in emergency departments [4,5]. Previous studies found that an increase in the number of patients in emergency departments negatively affected pain control of these patients [6,7]. High mortality rates and input of health care resources among patients who rely on mechanical ventilation were reported in situations where the patients experienced a delay in admission into intensive care units and were forced to wait in emergency departments [8]. Emergency department crowding must be reduced to deliver proper treatment to patients with acute conditions. One way to achieve this is to shorten the length of stay in emergency departments. Severely ill patients must be hospitalized in intensive care units without staying in emergency departments any further for the sake of better prognoses [9-11]. There is a problem of having internal medicine physicians in emergency departments. For example, when an emergency medicine physician refers to an internal medicine physician, the internal medicine physician must contact senior physicians or faculty from their departments to discuss hospitalization or discharge of the patient, as well as treatment directions. This leads to increased time spent by patients in emergency departments, longer wait times until treatment, and emergency department crowding.
The results of this study also support this finding as the lengths of stay in the emergency department were reduced by 15.1% when an internal medicine physician was not present in the emergency department. The lengths of stay in the emergency department were especially significantly reduced by 24.0% for nephrology. This may be because a large number of chronic patients suffer from renal diseases such as chronic kidney disease. Moreover, other types of diseases such as cardiac, pulmonary, and gastrointestinal diseases are excluded when making the decision of patient hospitalization or discharge in most cases. In this study, patients in the nephrology department with other associated conditions were referred to an internal medicine physician by an emergency medicine physician after they were admitted for hospitalization. This may be why the aforementioned reduction in the lengths of stay was observed in nephrology.
A previous study observed that when a hospitalization form was issued by an emergency medicine physician instead of an internal medicine physician, and the more internal medicine departments that the patient was associated with, the greater patients the decrease in wait times until his/her hospitalization [12]. The Health Insurance Review and Assessment Service assesses cardiac diseases such as acute myocardial infarction. In addition, critical pathway guidelines were established in most general hospitals, and they were subject to quality index management. This allows physicians to make fast decisions on patient treatment and hospitalization/discharge [13].
In this study, the mean length of stay in cardiology was shortest by 100.4 minutes in the study group, signifying a 19.9% reduction compared to the control group. The length of stay for cardiac patients admitted to intensive care units was 93.7 minutes, 37.2% lower than that of the control group. No significant differences were found between the discharged cardiac patients of the study and control groups. Therefore, it appears that protocols with only a presence of emergency medicine physicians may be more effective at assessing patients with cardiac diseases than those with the presence of internal medicine physicians.
Moreover, one study reported no correlation between the number of patients with ST-segment elevation acute myocardial infarction in emergency departments during busy hours and the time until percutaneous coronary intervention [14]. This suggests that emergency patients do not have to be treated in the department associated with their condition. The lengths of stay for hemato-oncology were the longest, and they were not reduced even after the new treatment protocol was applied. The main reason for this observation was that a large number of hemato-oncology patients visited the emergency department for a blood transfusion. While the lengths of stay were reduced for patients who requested hospitalization, they remained unchanged for patients who were discharged from the emergency department. Therefore, looking at hemato-oncology patients as a whole, no significant reduction in the length of stay in the emergency department was observed.
Another problem is that emergency medicine physicians do not actively issue hospitalization forms as they must obtain permission from senior internal medicine physicians or faculty to do so. They may be reluctant to hospitalize patients even when there are plenty of wards available in the hospital. In this study, the hospitalization rate was increased by 36.5% when emergency medicine residents were present. Of course, if too many hospitalization forms are issued while enough wards are not available, the lengths of waiting times and stays in the emergency department may increase. However, this may not be a serious problem since a decrease in lengths of stay was observed in this study when emergency medicine physicians were present to examine the patients. Since patients who visit emergency departments may require an immediate input of healthcare resources at any time, and emergency departments have a limited amount of healthcare resources, it is essential to quickly transfer patients to hospital wards for subsequent treatment after providing initial management and stabilizing patientsŌĆÖ conditions [15-17]. A study has actually reported increased treatment delays and complication rates when severely ill patients and patients with cardiovascular diseases visited an emergency department at the same time [18].
The overall hospitalization rate, as well as the rates of hospitalization in intensive care units and general wards all showed significant increases in the present study. The rates of hospitalization in intensive care units significantly increased in gastroenterology, pulmonology, and nephrology patients. The observed increase may be attributed to the increase in the number of patients in intensive care units. Since emergency medicine physicians are assigned to the emergency department while internal medicine physicians are assigned to examine hospitalized patients, the continuity of patient care may be compromised. Therefore, patients may simply prefer to be admitted to intensive care units.
Emergency medicine physicians place more emphasis on patientsŌĆÖ symptoms rather than on the workload of internal medicine treatment when making a decision regarding patient hospitalization. This is because they feel little need to promptly refer severely ill patients to outpatient departments or monitor them in emergency departments, and instead prefer to hospitalize them for further monitoring and treatment. As a result, as emergency department physicians issue hospitalization forms, hospitalization rates increaseŌĆöas was observed in this studyŌĆöand the lengths of stay in emergency departments and the durations of hospitalization in intensive care units and general wards all decrease. This finding is similar to the result of a study in which the delay to hospitalization was correlated with the duration of hospitalization regardless of patientsŌĆÖ conditions [19]. It was possible that the mean duration of hospitalization decreased as an increased number of patients with mild conditions were admitted. However, in terms of hospital bed turnover rates and efficiency, reduction in the duration of hospitalization means more admission opportunities for patients.
In a study involving a hospital with 1,000 beds and bed utilization rates of less than 90%, the mean length of inpatient stay in the internal medicine department was 11.0 days. The treatment revenues per year increased by 300 million won when the length of stay was reduced by one day, and were estimated to increase by one billion won if the length of stay was reduced by three days [20]. In this study, the mean duration of hospitalization for patients who were admitted to the hospital via the emergency department was 10.3 days. Since the duration was reduced by 2.8 days, it can be reasoned that substantial profits would be made.
When an emergency medicine physician examines an internal medicine patient in the emergency department and issues a hospitalization form, the diagnosis of the patient may not be accurate. Therefore, this study investigated the accuracy of diagnoses between the time of admission and discharge. No significant differences were found between the concordance rates of diagnoses for internal medicine inpatients in both general wards and the intensive care unit. Therefore, there are no meaningful differences between emergency medicine physicians and internal medicine physicians when examining internal medicine patients. The concordance rates of diagnoses of pulmonary patients who were hospitalized in general wards significantly increased when an emergency medicine physician examined the patients. On the other hand, the concordance rates for cardiac patients were significantly reduced. Emergency medicine physicians prefer to monitor patient symptoms in the ward, rather than in the emergency department. For example, when a patientŌĆÖs chest discomfort persisted, the patient was hospitalized under the diagnosis of angina pectoris, rather than monitoring the patientŌĆÖs symptoms in the emergency department. After admission, laboratory follow-up and coronary angiography were performed, and the diagnosis was changed according to the results. As a result, the concordance rates of diagnoses had increased.
Our study has some limitations. First, this study was conducted in one university hospital, and the study was short in duration. Second, by conducting the study on patients who visited the emergency department at the same time and season, the variation of patients between the study group and the control group was minimized. However, the control of other factors including the number of physicians and other personnel was insufficient. Third, the study did not consider the impact of cooperation from other departments during patient examination and treatment. Fourth, some departments had a small sample size. Fifth, no indicators were established to assess whether patients were properly examined and treated while in the emergency department. Lastly, there is no mention of whether prognosis had improved or whether the patient died or had a poor prognosis. To overcome these limitations, additional research on treatment protocols for internal medicine patients in emergency departments should be conducted in the future.
The lengths of stay and durations of hospitalization may be effectively shortened by allowing emergency medicine physicians to make decisions on patient hospitalization, instead of having internal medicine physicians in the emergency department, and by improving admission protocols.
REFERENCES2. Lee WP. Shortage in residents of internal medicine and current status of Korean medical system. J Korean Med Assoc 2015; 58:368-71.
3. McCoy JV, Gale AR, Sunderram J, Ohman-Strickland PA, Eisenstein RM. Reduced hospital duration of stay associated with revised emergency department-intensive care unit admission policy: a before and after study. J Emerg Med 2015; 49:893-900.
4. Collis J. Adverse effects of overcrowding on patient experience and care. Emerg Nurse 2010; 18:34-9.
5. Tekwani KL, Kerem Y, Mistry CD, Sayger BM, Kulstad EB. Emergency department crowding is associated with reduced satisfaction scores in patients discharged from the emergency department. West J Emerg Med 2013; 14:11-5.
6. Hwang U, Richardson LD, Sonuyi TO, Morrison RS. The effect of emergency department crowding on the management of pain in older adults with hip fracture. J Am Geriatr Soc 2006; 54:270-5.
7. Hwang U, Richardson L, Livote E, Harris B, Spencer N, Sean Morrison R. Emergency department crowding and decreased quality of pain care. Acad Emerg Med 2008; 15:1248-55.
8. Hung SC, Kung CT, Hung CW, et al. Determining delayed admission to intensive care unit for mechanically ventilated patients in the emergency department. Crit Care 2014; 18:485.
9. Multz AS, Chalfin DB, Samson IM, et al. A ŌĆ£closedŌĆØ medical intensive care unit (MICU) improves resource utilization when compared with an ŌĆ£openŌĆØ MICU. Am J Respir Crit Care Med 1998; 157(5 Pt 1):1468-73.
10. Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA 2002; 288:2151-62.
11. Carson SS, Stocking C, Podsadecki T, et al. Effects of organizational change in the medical intensive care unit of a teaching hospital: a comparison of ŌĆśopenŌĆÖ and ŌĆśclosedŌĆÖ formats. JAMA 1996; 276:322-8.
12. Mun SW, Jeong SG, Oh YM, et al. Effect of issuing of hospitalization sheets by emergency department on shortening length of stay. J Korean Soc Emerg Med 2009; 20:10-19.
13. Park EC. Problems and future directions for quality evaluation of the Health Insurance Review and Assessment Service. J Korean Med Assoc 2015; 58:176-8.
14. Harris B, Bai JC, Kulstad EB. Crowding does not adversely affect time to percutaneous coronary intervention for acute myocardial infarction in a community emergency department. Ann Emerg Med 2012; 59:13-7.
15. Kumar A, Roberts D, Wood KE, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 2006; 34:1589-96.
16. Gaieski DF, Mikkelsen ME, Band RA, et al. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med 2010; 38:1045-53.
17. Mitka M. Reducing door-to-needle time for tPA use remains an elusive goal in stroke care. JAMA 2011; 305:1288-9.
18. Fishman PE, Shofer FS, Robey JL, et al. The impact of trauma activations on the care of emergency department patients with potential acute coronary syndromes. Ann Emerg Med 2006; 48:347-53.
19. Richardson DB. The access-block effect: relationship between delay to reaching an inpatient bed and inpatient length of stay. Med J Aust 2002; 177:492-5.
20. Lee HJ, Kim YH, Lee EP, Kim SW, Jeoung BH. An analysis on the effectiveness of hospital revenues per bed by shortening length of stay. Korean J Hosp Manag 1998; 3:100-20.
Fig.┬Ā1.Study protocol for internal medicine patients in the emergency department when internal medicine physician is not in the emergency department. ED, emergency department; EM, emergency medicine; IM, internal medicine 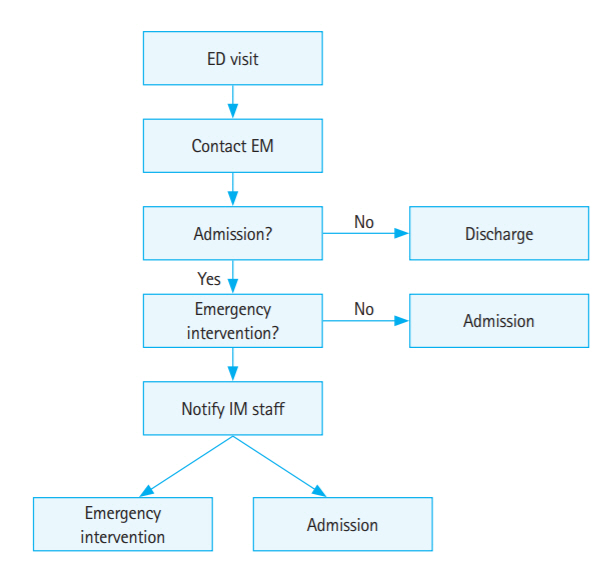
Fig.┬Ā2.Control protocol for internal medicine patients in the emergency department when internal medicine physician is in the emergency department. ED, emergency department; EM, emergency medicine; IM, internal medicine. 
Table┬Ā1.General characteristics of patients Table┬Ā2.Distribution of patients who visited the emergency department Table┬Ā3.Admission of patients who visited the emergency department
Table┬Ā4.Comparison of lengths of stay in the emergency department
Table┬Ā5.Comparison of durations of hospitalization
Table┬Ā6.Comparison of concordance rates between admission and discharge diagnoses
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||