INTRODUCTION
The term “pneumoparotid” is defined as the presence of air within parotid acini and ducts [1]. Pneumoparotid with associated infection describes pneumoparotitis, a rare pathology of the parotid gland. Pneumoparotitis is caused by retrograde introduction of microbes into the parotid gland via pneumatic trauma to the gland [2]. Due to abundant oral flora, it is rare to have pneumoparotid without pneumoparotitis. Increases in intraoral pressure, caused by any type of Valsalva maneuver, or an incompetent Stenson’s duct are associated with pneumoparotitis. Because it often presents as edema and local pain in the parotid area, pneumoparotitis is often misdiagnosed as parotitis.
The common patient population includes wind instrumentalists and adolescents with psychosocial issues [3]. Patients are usually aware of their ability to inflate the parotid system. Diagnosing pneumoparotitis becomes challenging in cases in which patients cannot voluntarily insufflate the parotid gland [4]. Treatment is dependent upon severity and length of disease and ranges from supportive measures to surgery [2].
CASE REPORT
The case of an adult patient with recurrent subcutaneous emphysema of the head and neck is reviewed. The patient’s pertinent history, clinical findings, and imaging studies are examined. The patient is a 34-year-old prison inmate with bipolar disorder presenting with recurrent sensations of a “pop” in the neck region with associated bilateral facial swelling and palpable crepitus of the head and neck.
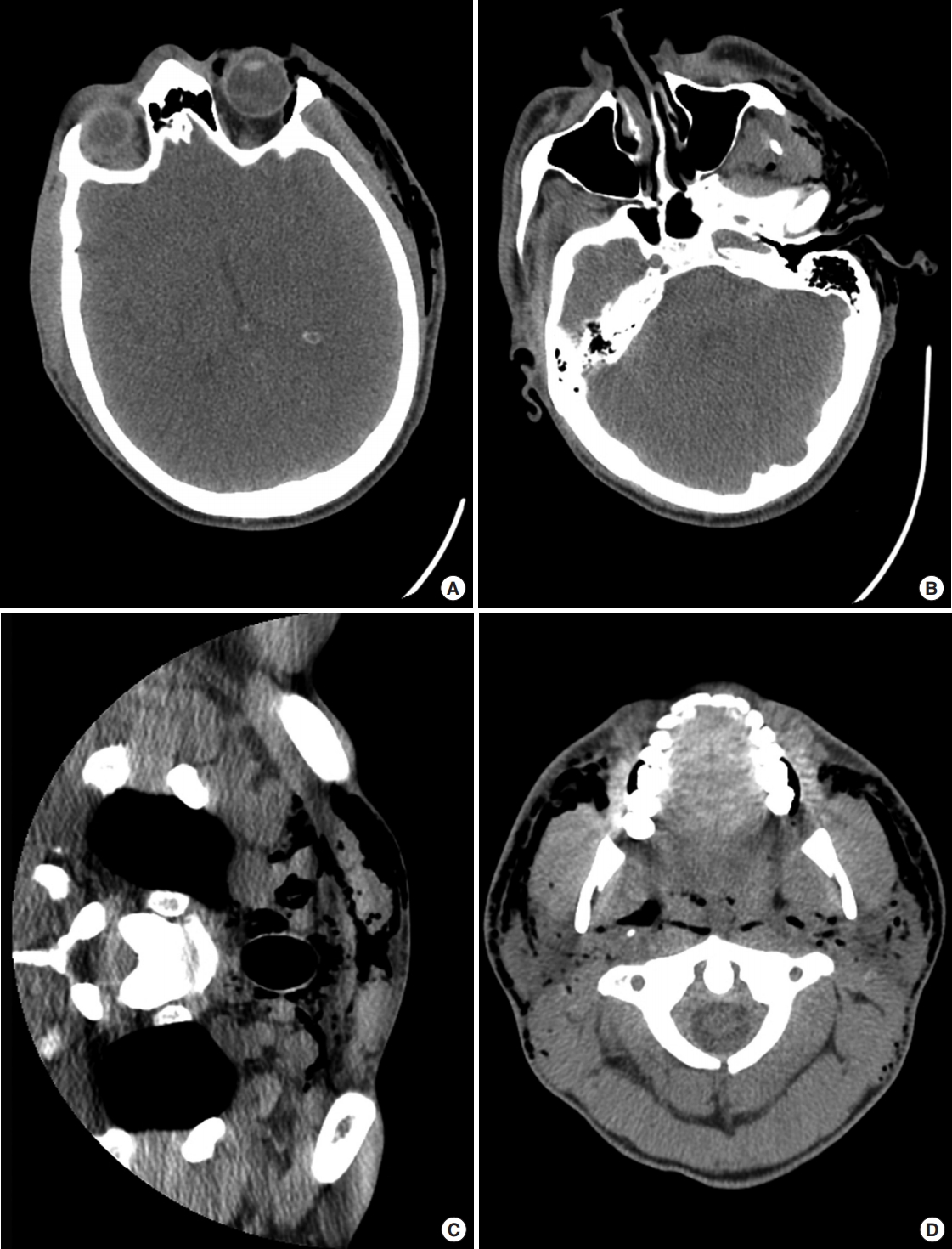
Physical examination revealed left periorbital, left facial, and bilateral neck edema with palpable crepitus throughout. Computed tomography showed subcutaneous emphysema of the left facial and bilateral neck soft tissues, from the level of the scalp to the sternal notch (Figs. 1, 2). Against medical advice, the patient refused the recommendation for intubation. The patient was also encouraged to undergo direct laryngoscopy and esophagoscopy to evaluate the piriform sinuses and vallecula in detail and to rule out possible pharyngeal perforation. However, the patient refused direct laryngoscopy, and esophagoscopy. Flexible laryngoscopy revealed fibrinous exudate and discolored debris along the vallecula and piriform sinuses bilaterally, with the left piriform containing more debris than the right. The subglottis was widely patent.
Barium swallow demonstrated no obvious perforation, with no penetration of oral contrast into the cervical soft tissues. Chest X-ray showed subcutaneous emphysema in the cervical region and upper mediastinum without evidence of pneumothorax. The patient received intravenous antibiotics due to a mild leukocytosis of 15.3×109/L, along with morphine for pain control. The patient was discharged with oral antibiotics following improvement in his symptoms and leukocytosis.
The patient presented twice more to the emergency room with a similar presentation, including left-sided otalgia, nausea and vomiting, facial pain, and facial swelling. These symptoms developed after the patient felt a “pop” in his left ear followed by the taste of blood. Physical examination showed bilateral periorbital and facial edema, which was predominately left sided. The patient had palpable crepitus from the left temporal region to the clavicle. Purulence was expressed from the left Stenson’s duct. The floor of the mouth was soft, and without edema. Computed tomography continued to show subcutaneous emphysema from the level of the scalp to the sternal notch.
The patient’s multiple similar presentations, associated nausea and vomiting, imaging, and opportunity to leave prison all support the diagnosis of self-inflicted pneumoparotitis. After receiving intravenous antibiotics, the patient was discharged and encouraged to use warm compresses, sialagogues, massage, and aggressive hydration.
DISCUSSION
Parotid swelling can be attributed to infection, autoimmune disease, endocrine disorders, and duct obstruction. Pneumoparotitis represents a rare cause of parotid gland swelling due to retrograde airflow through Stenson’s duct. Although frequently attributed to increased intraoral pressure, other factors may predispose to pneumoparotitis, such as hypertrophy of the masseter muscle, weakness of the buccinator muscle, and dilation of Stenson’s duct [1,3]. Pneumoparotitis has classically been described in psychiatric patients, adolescents, glass blowers, and trumpet players. Dental instrumentation (braces), chronic cough suppression, and coughing during extubation have also been associated with pneumoparotitis [2].
Presentation commonly involves gland enlargement and palpable crepitus [3]. Frothy saliva or purulence may be expressed from one or both of Stenson’s ducts [3]. The parotid gland may be painless or tender, with overlying warmth and erythema [5]. In more severe or long-lasting cases of pneumoparotitis, air may extend into the face and neck causing subcutaneous emphysema.
The gold standard for diagnosing pneumoparotitis is computed tomography, which reliably identifies air in the ductal system and is useful for differentiating air from calculi and inflammation [3,6]. Recent studies have suggested that a “puffed cheek” computed tomography technique has the potential to aid in diagnosis and reveal a greater prevalence [6]. Ultrasound is also useful for diagnosis [6].
Treatment ranges from conservative techniques to surgical intervention. In minor cases, anti-inflammatory agents and parotid stimulation provide relief. Since oral microbes are usually introduced in a retrograde fashion into the gland, antibiotics should be prescribed. Surgical clamping or ligation of Stenson’s duct are treatment options [3]. Parotidectomy is usually reserved for recurrent cases [3].
We describe a case of recurrent pneumoparotitis. The patient had incentive to recreate his symptoms, notably the subcutaneous emphysema, as this allowed him to leave prison and receive narcotics. Self-inflicted pneumoparotitis has been described in patients with psychological issues and adolescents. Counseling is recommended in these cases [2]. Munchausen syndrome involving pneumoparotitis has been described [2]. However, our patient represents a unique case of malingering, in which the secondary gain involved escape from prison and medication.
Pneumoparotitis represents a rare cause of parotid pain and swelling. Because its presentation is similar to infection and autoimmune diseases of the parotid, pneumoparotitis is often misdiagnosed. Retrograde movement of air into the parotid duct system accounts for the pathology involved and is necessary for diagnosis. Computed tomography demonstrates air in the parotid ducts and acini. Subcutaneous emphysema may result from this condition, presenting with facial edema and palpable crepitus.
Our case demonstrates some of the common presenting signs, such as purulence from Stenson’s duct and facial edema. The patient is unique in that his pneumoparotitis is recurrent and severe, involving subcutaneous emphysema from the scalp to the sternum. Also, the increase in intraoral pressure is self-induced.
In summary, pneumoparotitis represents a very rare cause of head and neck swelling. Pneumomediastinum can occur with severe cases of pneumoparotitis, such as the case presented above. Emergency physicians must be able to create a broad differential diagnosis for causes of pneumomediastinum. Diagnoses include benign entities such as spontaneous pneumomediastinum in young patients and life-threatening entities such as esophageal perforation and necrotizing mediastinitis. Pneumoparotitis represents a unique cause of facial swelling, subcutaneous emphysema, and pneumomediastinum of which emergency physicians should be aware. Knowledge regarding presenting symptoms, signs, and image findings characteristic of pneumoparotitis can help emergency physicians diagnose and treat these patients.