AbstractObjectiveAmong the pediatric population with minor head trauma, it is difficult to determine an indication for the usage of brain computerized tomography (CT). Our study aims to compare the efficiency of the most commonly used clinical decision rules: the Pediatric Emergency Care Applied Research Network (PECARN) and Canadian Assessment of Tomography for Childhood Head Injury 2 (CATCH2).
MethodsThis retrospective study investigated whether the PECARN and CATCH2 rules were applicable to Korean children with minor head trauma for reducing the use of brain CT imaging, while detecting intracranial pathology.
ResultsOverall, 251 patients (0–5 years old) admitted to emergency rooms within 24 hours of injury were included between August 2015 to August 2018. The performance results are as follows: the PECARN and CATCH2 rules had a sensitivity of 80.00% (51.91%–95.67%) and 100% (78.20%–100.00%) with a specificity of 28.39% (22.73%–34.60%) and 15.25% (10.92%–20.49%), respectively; the negative predictive values were 98.58% and 100%, respectively. Overall, the CATCH2 rule was more successful than the PECARN rule in detecting intracranial pathology; however, there was no significant difference between them. Furthermore, the PECARN and CATCH2 rules lowered the rate of head CT imaging in our study group.
ConclusionBoth the rules significantly lowered the rate of indicated brain CT. However, since the CATCH2 rule had higher sensitivity and negative predictive value than the PECARN rule, it is more appropriate to be used in emergency rooms for detecting intracranial pathology in children with minor head trauma.
INTRODUCTIONTraumatic brain injury (TBI) is among the most common causes of pediatric morbidity and mortality worldwide [1]. Although most head injuries in children do not result in clinically important TBI (ciTBI), which is defined as any acute intracranial finding revealed on computed tomography (CT) that would normally require admission to hospital and neurosurgical follow-up, children who are at risk must be identified as early as possible in the emergency department (ED) setting [1,2]. According to the Korea Centers for Disease Control and Prevention, pediatric head injury accounts for ≥40% of the injured and is the most common reason for visits to the ED [3]. Additionally, Oh et al. [4] reported a substantial increase in the number of CT examinations, which is known as the reference standard for diagnosing TBI over the last decade, as well as the number of pediatric patients since 2005 in South Korea.
CT is the reference standard for providing a rapid and definitive diagnosis of intracranial pathology [5]. However, CT is expensive than other health examinations, and it is not advisable to perform CT on every pediatric patient with minor head trauma because of the risks of radiation exposure [6-8]. Moreover, CT usage is resource-intensive and carries additional risks for children who require sedation for imaging [9,10].
For these reasons, many efforts have been made to limit pediatric CT exposure to “as low as reasonably achievable” for almost 20 years [11]. Countries like the US and Canada have come up with clinical decision rules for children with minor head trauma to determine whether the patient should undergo CT. A clinical decision rule is defined as a decision-making tool that incorporates three or more variables from the history and examination or simple tests derived from original research [12,13]. In the US, the Pediatric Emergency Care Applied Research Network (PECARN) developed a head trauma prediction rule for identifying children at low risk of ciTBI who do not require head CT [6]. In Canada, the Canadian Assessment of Tomography for Childhood Head Injury (CATCH) and CATCH 2 (CATCH2) rules supported the decision making to guide CT use in children with a minor head injury [14]. When implemented, both these rules have shown to decrease the rate of CT imaging for pediatric head trauma without missing injuries that warrant neurosurgical intervention [6,14].
In South Korea, although there have been some studies on the validity of the PECARN rule among children younger than 2 years with a minor head injury, there is a lack of information on how to implement clinical decision rules among the pediatric population with a minor head injury [15]. This study hypothesized that if these clinical decision rules were to be applied in South Korea, the rate of head CT for children with minor head trauma would decrease while detecting ciTBI in patients at risk of deterioration or need of neurosurgical intervention. The secondary aim is to determine which of the subparameters included in these rules are the most common and effective for detecting intracranial pathology. The primary aim of the study is to compare the validity and efficacy of the most commonly used clinical decision rules worldwide: the guidelines of the PEARN and the CATCH2 which has been updated from the previous CATCH rules.
METHODSStudy designThis is a retrospective study to investigate and compare the efficiency and effectiveness of the PECARN and CATCH2 rules for identifying Korean children with minor head trauma. The ethics committee waived the requirements for institutional review board approval, as the study does not fall within the criteria for approval since only anonymous medical information was used. The ethics committee of the hospital approved this study (WMCSB 2019 03-22-190214).
Study setting and populationThe retrospective study was performed in an education and research hospital in Gunpo, a suburb city outside of Seoul in South Korea, between August 2015 to August 2018. The average annual number of patients visiting the hospital’s ED is about 25,000. of these, approximately 10%–15% are children. This study determined the appropriate brain CT indication for children younger than 5 years with minor blunt head trauma admitted to the ED. Patients were selected if the routine departmental coding contained any indication of head trauma.
The effectiveness and efficiency of the PECARN and CATCH2 clinical decision rules were investigated and compared, which are recommended by many physicians and literature for diagnosing severely injured patients while minimizing inappropriate brain CT requests. Furthermore, each parameter of these rules was assessed separately for detecting intracranial pathology.
Children (0–5 years old) with acute head injury were eligible to be included in the study if they had blunt head trauma and Glasgow Coma Scale (GCS) of ≥14 admitted to an emergency room (ER) within 24 hours of injury. Patients with a GCS of <14, penetrating head trauma or depressed fracture, bleeding disorder, trivial injury, or incomplete data were ineligible for the study (Fig. 1).
MeasurementsTwo emergency physicians manually reviewed electronic health records of all patients included in the study; the patient data included demographic characteristics, medical and personal history, time of injury and ED attendance, mechanism of injury and site of trauma, symptoms, mental status, and CT scan findings. CT scans were independently reviewed by a radiologist at the hospital who was not aware of this study.
The variables were recorded according to the PECARN and CATCH2 rules, and prior to data collection, guidelines and definitions for data abstraction and definition were developed.
Management of patients and data collectionIn the analysis of the PECARN prediction rule, patients who underwent brain CT imaging with minor head trauma were evaluated and classified as high-risk, intermediate-risk, and low-risk groups according to the age groups of <2 years old and 2–5 years old. Children were classified as a high-risk group if they had altered mental status or palpable skull fracture for <2 years old and altered mental status or signs of basilar fracture for 2–5 years old. Two-year-old children with one or more intermediate-risk predictors, which consist of severe injury mechanism, loss of consciousness for >5 seconds, non-frontal hematoma, and not acting normally according to parents, were considered positive. Children of 2–5 years old were considered as intermediate risk if they had one or more of the followings: severe injury mechanism, any loss of consciousness, vomiting, or severe headache (Fig. 2). The PECARN rule was considered positive when children had any of the high-risk or intermediate-risk predictors; the rule was considered negative when children had no predictors.
In the analysis of the CATCH2 rule, irrespective of the age group, when children had any of the predictors among the eight variables, which are a GCS of <15 at 2 hours after injury, suspected open or depressed skull fracture, headache, irritability, any sign of basal fracture, large and boggy hematoma, dangerous mechanism of injury, or ≥4 episodes of vomiting, they were considered positive (Fig. 3).
Patients were divided into those with and without intracranial pathology according to their brain CT result. The pathologies detected using brain CT were classified as follows: only skull fracture, epidural hemorrhage with a skull fracture, subdural hemorrhage with a skull fracture, subarachnoid hemorrhage with a skull fracture, only intracerebral hemorrhage (ICH), and ICH with a skull fracture [16]. The presence or absence of intracranial pathologies detected using brain CT represents the endpoint of both the PECARN and CATCH2 decision rules.
This study analyzed and compared the diagnostic value of two clinical decision rules: the PECARN and CATCH2. The accuracy, sensitivity, specificity, and positive and negative predictive values with 95% confidence intervals (CIs) between the two clinical decision rules were evaluated, comparing the effectiveness and their efficacy in predicting intracranial pathology in a minor head injury.
Statistical analysesThe two rules were assessed for their classification performance (i.e., sensitivity and specificity) for identifying ciTBI. SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA) was used for analyzing the data. Fisher exact test was used for the comparison of non-normal distribution data, while the chi-squared test was used for the comparison of frequency data. The sensitivity and specificity of the PECARN and CATCH2 rules for predicting intracranial pathology were determined, and the positive and negative likelihood values were calculated. A P-value of <0.05 was considered statistically significant.
RESULTSOverall, 251 patients admitted to ED within 24 hours of injury who met the inclusion criteria and who underwent brain CT imaging were included in the study (Fig. 1). The demographic characteristics of these patients are presented in Table 1. Two hundred twenty nine (91.2%) patients had a GCS of 15, and 22 (8.7%) patients had a GCS of 14. Regarding the mechanism of injury, fall (82%) was observed mostly in the <2 years old group and 2–5-years old group (60.7%), followed by head struck injury in both the groups. In the <2 years old group, seven (8.9%) patients had acute brain lesions, and in the 2–5 years old group, eight (4.6%) patients had ciTBI on brain CT evaluation; thus, the incidence of ciTBI was significantly higher in the <2 years old group. Among the 15 patients with ciTBI, five patients had only linear skull fracture, followed by three patients in the epidural hemorrhage with a skull fracture and in the ICH only group, two patients in the subdural hemorrhage with a skull fracture group, and one patient in subarachnoid hemorrhage, SAH with skull fracture and ICH with skull fracture group, respectively (Fig. 4).
In comparing the indication parameter of the PECARN and CATCH2 rules among “brain injury group” and “no brain injury group”, one of the subparameters, namely, ‘nonfrontal hematoma’ in the <2 year old group of the PECARN, was the only one that showed statistical significance with a P-value of 0.023. However, in the 2–5 years old group, none of the indicated parameters showed any statistical difference. In the CATCH2 rule, ‘irritability on examination’ was found to be statistically significant with a P-value of 0.035 (Table 2).
When the PECARN rule was applied to our cohort, among the low-risk group in the <2 years old group, one patient had ciTBI, and in the 2–5 years old group, two patients had ciTBI; hence, the PECARN rule failed to identify three patients with ciTBI. The CATCH2 rule was able to detect those three patients as the high-risk group. The patient in the <2 years old group who was not identified by the PECARN rule but who was recognized as high-risk in the CATCH2 rule had vomiting for ≥4 times. In the 2–5 years old group, two patients who were undetected using the PECARN rule but who were considered as high-risk using the CATCH2 rule had a large, boggy hematoma of the scalp and had a fall from a height greater than 91 cm.
When the PECARN and CATCH2 rules were compared for the sensitivity, specificity, and positive and negative predictive values in the <2 years old group, the PECARN rule had a sensitivity, specificity, positive predictive value, and negative predictive value of 85.71%, 18.31%, 2.10%, and 98.43%, respectively. The CATCH2 rule had a sensitivity, specificity, positive predictive value, and negative predictive value of 100%, 19.72%, 2.48%, and 100%, respectively; however, considering 95% CIs, these values showed no statistical significance with the values of 59.04% to 100%, 11.22% to 30.86%, 2.22% to 2.77%, and 59.04% to 100%, respectively (Table 3). In the 2–5 years old group, the PECARN rule had sensitivity, specificity, positive predictive value, and negative predictive value of 75.00%, 32.73%, 2.22%, and 98.46%, respectively, and the CATCH2 rule had a sensitivity, specificity, positive predictive value, and negative predictive value of 100%, 13.33%, 2.30%, and 100%, respectively. In consideration of 95% CIs, which was different from those of the <2 years old group, this group showed a statistical difference in specificity and accuracy (Table 4).
In the analysis of the overall age group from 0 to 5 years old, the PECARN rule had a sensitivity, specificity, positive predictive value, and negative predictive value of 80.00%, 28.39%, 2.23%, and 98.58%, respectively, and the CATCH2 rule had a sensitivity, specificity, positive predictive value, and negative predictive value of 100%, 15.25%, 2.35%, and 100%, respectively. Similar to the 2–5 years old group, the overall age group showed a statistically significant difference for both specificity and accuracy (Table 5).
DISCUSSIONFor the purpose of a diagnostic tool for screening, in our study, CATCH2 seems to be suitable with higher sensitivity and ease to use in spite of age, which could be quickly done by the bedside in the ED. However, in consideration of the negative effects of the brain CT such as the radiation exposure on the child and the high health expenses, the PECARN rule seems to be more appropriate with higher specificity. When the PECARN clinical decision rule was applied to this study it decreased the number of patients who would require brain CT by 13% compared to when the CATCH2 rule was applied, yet PECARN was unable to detect three patients with ciTBI who were categorized into low-risk group.
Although CT is known to be the most practical and accurate diagnostic technique for TBI, consideration of economic feasibility and the risk of radiation are the reasons why it should be used with caution. Lethal malignancies have been reported to occur in one in 1,000–5,000 pediatric brain CT scans and must be balanced against the risks of radiation induced malignancy [17]. For example, when the same radiation dose is administered, a 1-year-old is 10–15 times more likely to develop cancer than a 50-year-old [17]. Especially in pediatric patients, we need to be more careful and considerate when choosing the diagnostic technique because children are more susceptible to the risks of radiation and sedation.
Many clinical decision rules have been postulated to reduce the number of CT scans while detecting ciTBI, especially in children who are often unable to express their present symptoms and in whom the examination for possible pathological abnormalities is limited. The US and Canada have come up with clinical decision rules for identifying children with minor head trauma to determine whether the patient should undergo brain CT.
In 2009, Kupperman et al. [6] reported a prospective cohort study wherein the PECARN rule was able to identify children at very low-risk of ciTBIs for whom CT scans can be routinely ruled out.
In 2018, Osmond et al. [14] reported a multicenter cohort study in Canada to develop a highly sensitive clinical decision rule for the use of CT in children with a minor head injury. They concluded that for children with a minor head injury, the CATCH rule is a sensitive, prospectively derived clinical decision rule that has the potential to both standardize the need for CT and reduce the number of CT scans performed.
In 2019, Bozan et al. [18] compared the efficiency of the PECARN and CATCH and both were found to be effective in determining the necessity of brain CT for children with minor head trauma. The study showed that the implementation of clinical decision rules reduced the number of unnecessary CT scans and concluded that the PECARN proved to be more useful for emergency services because of its higher sensitivity. The study further analyzed the set of parameters that were more common and effective and suggested the superiority of the PECARN rule; the authors concluded that a low GCS (GCS <15) and the presence of nonfrontal hematoma were the most effective parameters for pathology determination.
After the comparison study of the PECARN and CATCH rules, Osmond et al. [14] came up with new iteration, the CATCH2 rule, that has greatly increased the sensitivity of the CATCH rule by adding a new component (vomiting ≥4 times). The CATCH2 rule affirmation and refinement was based on the original post hoc dataset; hence, it was not prospectively validated. We conducted the first retrospective study to evaluate the applicability of the PECARN and CATCH2 rules for children with minor head trauma in South Korea.
Both the PECARN and CATCH2 rules have a parameter to assess children for their “normal” behavior by the parent and physicians and are classified as “irritability on examination”, “agitation”, and “not acting right as per the parent” subparameters. The CATCH2 rule includes a subparameter to assess children for their normal behavior in “irritability on examination” by the physician, and the PECARN rule has a criterion included in the high-risk group to assess “altered mental status”, which includes agitation, sleepiness, and slow response as well as “not acting right as per parents” in the intermediate-risk group. Assessing the patient for their “normal behavior” after traumatic brain injury could be controversial and difficult for the parent and physician. Since these judgments could be significant in determining whether the child should undergo brain CT scans, we have considered several factors when assessing the patient’s behavior. We checked whether the child was administered a sedative and the number of administrations prior to performing a brain CT scan, which could indicate the irritability of the child. We also considered if the child showed any signs of irritability, which according to the World Health Organization-Emergency Triage Assessment and Treatment, the continuously “irritable or restless child” is defined as conscious but who cries constantly and would not settle [19]. The subparameter of assessing the normality of the patient in the CATCH2 rule is the “irritability on examination” (Table 2), which is considered one of the significant factors, yet in the PECARN rule, the “altered mental status” seemed to be not very important. This difference could be owing to the subcategories; the PECARN has a subcategory of high-risk group of “altered mental status” in which the patient must have one of the following symptoms: agitation, somnolence, repetitive questions, slow response to verbal communication, or palpable skull fracture.
The performance results of the PECARN and CATCH2 rules are detailed in Table 5. The CATCH2 rule had a higher sensitivity (100%) and negative predictive value (100%) than the PECARN rule (80% and 98.58%, respectively). Overall, the CATCH2 rule was more successful than the PECARN rule in detecting patients with ciTBI with higher sensitivity and negative predictive value; however, there was no significant difference between them according to their confidence intervals. However, the specificity showed a significant difference between the PECARN and CATCH2 rules, and the accuracy was also higher for the PECARN rule than for the CATCH2 rule (Table 5). With a higher specificity of the PECARN rule, 34 fewer patients were evaluated for brain CT imaging, that is, less radiation exposure and health expense; however, three patients with ciTBI could not be detected. However, these three patients did not need neurological intervention or further treatment.
One patient with ciTBI who was not identified using the PECARN rule was in the <2 years old group and two patients were in the 2–5 years old group. The CATCH2 rule was able to detect the patient in the <2 years old group because of the vomiting incidence of ≥4 times. The other two patients with ciTBI who were not identified using the PECARN rule were in the 2–5 years old group, whereas the CATCH2 rule was able to identify the patient owing to the different standard of “fall” height measurement and the presence of a scalp hematoma. One patient fell from 100 cm stairs, and the other had a large occipital hematoma who fell from a 60 cm height, both of which were the indications for brain CT evaluation according to the CATCH2 rule in the high-risk group. Of these three patients who were excluded from the PECARN’s indication for brain CT imaging, two had nondisplaced fractures without hemorrhage, and one had intracranial hemorrhage without fracture as revealed by brain CT.
In 2000, based on a large study by the Centers for Disease Control and Prevention in the US, 98% of patients with traumatic head injury had a ‘mild’ form of traumatic head injury, and the most common cause included ‘falls’ (28%), followed by motor vehicle crash (20%) and collision (19%) [20]. In our study, the most common cause of injury was falls (67.3%), head struck by a high impact object (18.3%), and sports related injuries (6.7%). The common mechanisms of the injury may be different from those reported in other studies as our study only included 0–5 years old children who are more susceptible to hard objects and “falling” from chairs or even from slides in a playground, and many are related to sports.
When the PECARN and CATCH2 rules were applied to the study group of 251 patients, 181 (72%) and 215 (85%) patients met criteria for brain CT scanning with the PECARN and CATCH2 rules, respectively. This shows that when these two rules are applied for the indication of brain CT scanning, the number of patients exposed to CT scanning is decreased. Although when the PECARN rule was applied to our study, it decreased the number of patients who met criteria for brain CT scanning by 13% when compared with the CATCH2 rule; however, the PECARN rule was unable to identify three patients with ciTBI who were categorized into the low-risk group. In consideration of the negative effects of head CT scanning, such as radiation exposure on children and increased health expenses, the PECARN rule seems to be more appropriate with higher specificity. It can be a controversial issue whether decreasing the number of CT imaging is more important for achieving a decreased risk of radiation-induced malignancy or having increased CT imaging is more critical for achieving a better diagnosis of pathology of the brain in children. According to other studies, since children who are at risk for deterioration or in need of neurosurgical intervention must be identified quickly in the ED setting, the clinical decision rule with a higher sensitivity (CATCH2 rule) should be chosen over the other rule since detecting the pathology is more crucial [1].
Our study has limitations. This study hypothesized that if either the PECARN and CATCH2 clinical prediction rules were to be applied in South Korea, the rate of brain CT scanning for children with minor head trauma should decrease. However, it is controversial to directly compare them, as they target different age groups and standards of injury severity using different outcomes. Moreover, the PECARN rule was developed to identify children at very low risk of ciTBI, and thus, should not undergo CT scanning. In contrast, the CATCH2 rule was designed to identify children at a high risk of brain injury and should undergo CT scanning. Therefore, it may not be accurate to compare and conclude which rule has a higher sensitivity for detecting ciTBI in the ED. Therefore, further multicenter validation studies across different settings are needed, including studies in general EDs and pediatric departments.
In conclusion, both the PECARN and CATCH2 clinical decision rules significantly lowered the rate of brain CT scanning. However, because the CATCH2 rule has a higher sensitivity and negative predictive value than the PECARN rule, it seems to be more appropriate to be used in the EDs for detecting ciTBI in children with minor head trauma, as it is critical and necessary to identify any abnormalities in the brain quickly for preventing long-term complications.
REFERENCES1. Burstein B, Upton JE, Terra HF, Neuman MI. Use of CT for head trauma: 2007-2015. Pediatrics 2018; 142:e20180814.
2. Stiell I, Lesiuk H, Vandemheen K, et al. Obtaining consensus for the definition of “clinically important” brain injury in the CCC Study. Acad Emerg Med 2000; 7:572.
3. Korea Centers for Disease Control and Prevention. Statistics of type of injury and cause. Cheongju: Korea Centers for Disease Control and Prevention; 2016.
4. Oh HY, Kim EY, Kim JE, et al. Trends of CT use in the pediatric emergency department in a tertiary academic hospital of Korea during 2001-2010. Korean J Radiol 2012; 13:771-5.
5. Brenner DJ, Hall EJ. Computed tomography: an increasing source of radiation exposure. N Engl J Med 2007; 357:2277-84.
6. Kuppermann N, Holmes JF, Dayan PS, et al. Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet 2009; 374:1160-70.
7. Bouida W, Marghli S, Souissi S, et al. Prediction value of the Canadian CT head rule and the New Orleans criteria for positive head CT scan and acute neurosurgical procedures in minor head trauma: a multicenter external validation study. Ann Emerg Med 2013; 61:521-7.
8. Kavalci C, Aksel G, Salt O, et al. Comparison of the Canadian CT head rule and the new orleans criteria in patients with minor head injury. World J Emerg Surg 2014; 9:31.
9. Goldwasser T, Bressan S, Oakley E, Arpone M, Babl FE. Use of sedation in children receiving computed tomography after head injuries. Eur J Emerg Med 2015; 22:413-8.
10. Hoyle JD Jr, Callahan JM, Badawy M, et al. Pharmacological sedation for cranial computed tomography in children after minor blunt head trauma. Pediatr Emerg Care 2014; 30:1-7.
11. The ALARA (as low as reasonably achievable) concept in pediatric CT intelligent dose reduction. Multidisciplinary conference organized by the Society of Pediatric Radiology. August 18-19, 2001. Pediatr Radiol 2002; 32:217-313.
12. Laupacis A, Sekar N, Stiell IG. Clinical prediction rules. A review and suggested modifications of methodological standards. JAMA 1997; 277:488-94.
13. Wasson JH, Sox HC, Neff RK, Goldman L. Clinical prediction rules: applications and methodological standards. N Engl J Med 1985; 313:793-9.
14. Osmond MH, Klassen TP, Wells GA, et al. Validation and refinement of a clinical decision rule for the use of computed tomography in children with minor head injury in the emergency department. CMAJ 2018; 190:E816-22.
15. Jung KY, Han SB, Lee JS, Kim JJ, Suh YJ, Kim JH. Availability of the Pediatric Emergency Care Applied Research Network (PECARN) rule for computed tomography scanning decision in children younger than 2 years with minor head injury. Pediatr Emerg Med J 2015; 2:67-74.
16. Tenny S, Thorell W. Intracranial hemorrhage. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2020 [cited 2020 Sep 6]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470242/.
17. Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol 2001; 176:289-96.
18. Bozan O, Aksel G, Kahraman HA, Giritli O, Eroglu SE. Comparison of PECARN and CATCH clinical decision rules in children with minor blunt head trauma. Eur J Trauma Emerg Surg 2019; 45:849-55.
19. World Health Organization. Emergency Triage Assessment and Treatment (ETAT): manual for participants [Internet]. Geneva: World Health Organization; 2005 [cited 2020 Sep 6]. Available from: http://whqlibdoc.who.int/publications/2005/9241546875_eng.pdf.
20. National Center for Injury Prevention and Control. Traumatic brain injury in the United States: assessing outcomes in children. Atlanta, GA: Centers for Disease Control and Prevention; 2008.
Fig. 1.Flow chart of patient selection. GCS, Glasgow Coma Score; CT, computed tomography; ciTBI, clinically important traumatic brain injury. 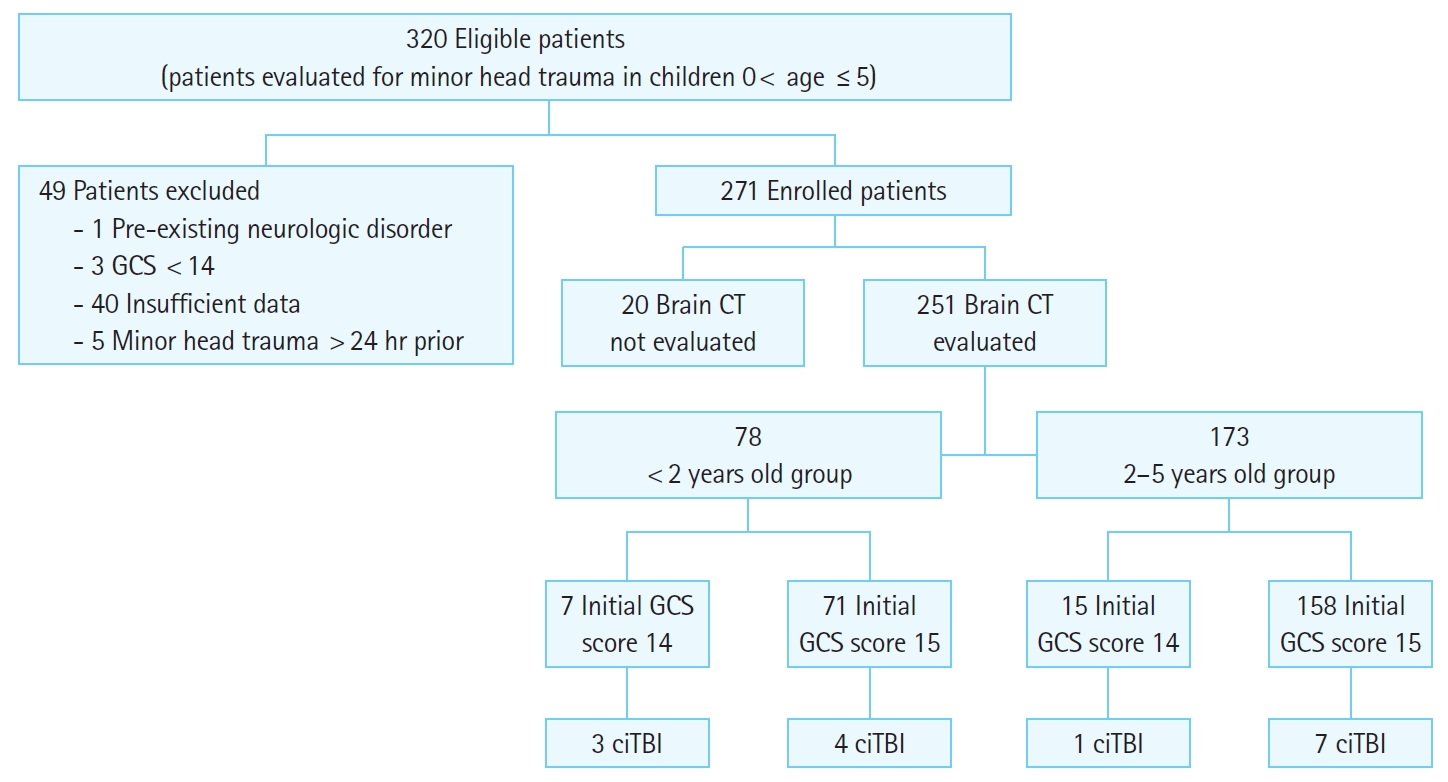
Fig. 2.The Pediatric Emergency Care Applied Research Network (PECARN) age-based clinical prediction rule for high, intermediate, and low traumatic brain injury risk groups. TBI, traumatic brain injury. a)Ground level falls or running into stationary objects with no signs of TBI other than scalp abrasion and lacerations. b)Glasgow Coma Scale 14, agitation, sleepiness, slow response or repetitive questioning. c)Retroauricular brusing (battle sign), periorbital bruising (raccoon eye), cerebrospinal fluid otorrhea, or hemotympanum. d)Motor vehicle crash with patient ejection, death of another passenger or rollover, pedestrian or bicyclist without helmet struck by motorized vehicle, falls of >3 feet for children <2 years of age or >5 feet for children >2 years or head struck by high impact object. 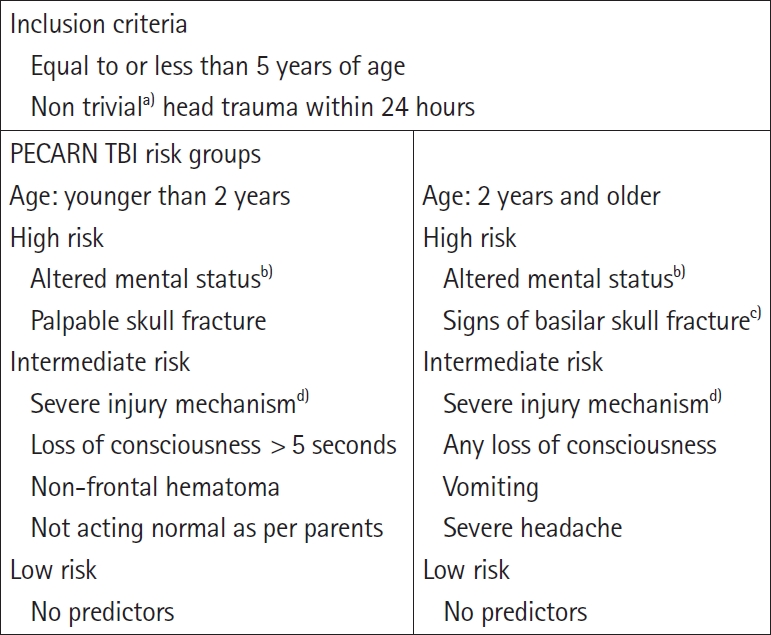
Fig. 3.The Canadian Assessment of Tomography for Childhood Head Injury 2 rule. CT, computed tomography; GCS, Glasgow Coma Score. a)Minor head injury is defined as injury within the past 24 hours associated with witnessed loss of consciousness, definite amnesia, witnessed disorientation, persistent vomiting (>1 episode), or persistent irritability (in a child aged <2 years) in a patient with a GCS score of 13 to 15. b)igns of basal skull fracture include hemotympanum, raccoon eye, otorrhea, or rhinorrhea of the cerebrospinal fluid, and Battle sign. c)Dangerous mechanism is a motor vehicle crash, a fall from elevation ≥91 cm or 5 stairs, or a fall from a bicycle with no helmet. 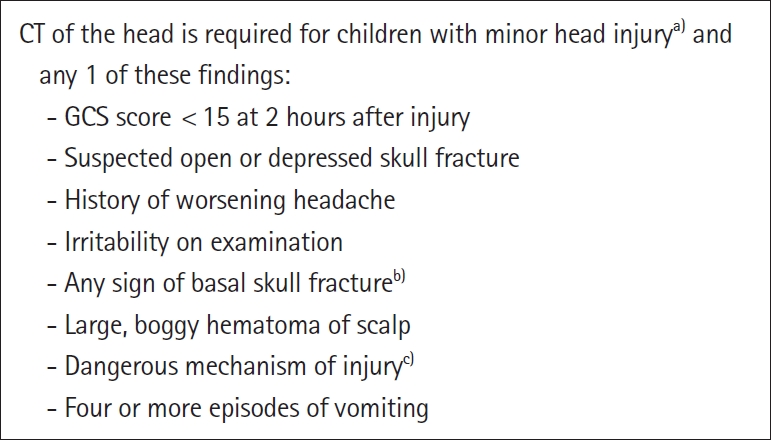
Fig. 4.Clinically important traumatic brain injury according to age groups. EDH, epidural hemorrhage; SDH, subdural hemorrhage; SAH, subarachnoid hemorrhage; ICH, intracerebral hemorrhage. 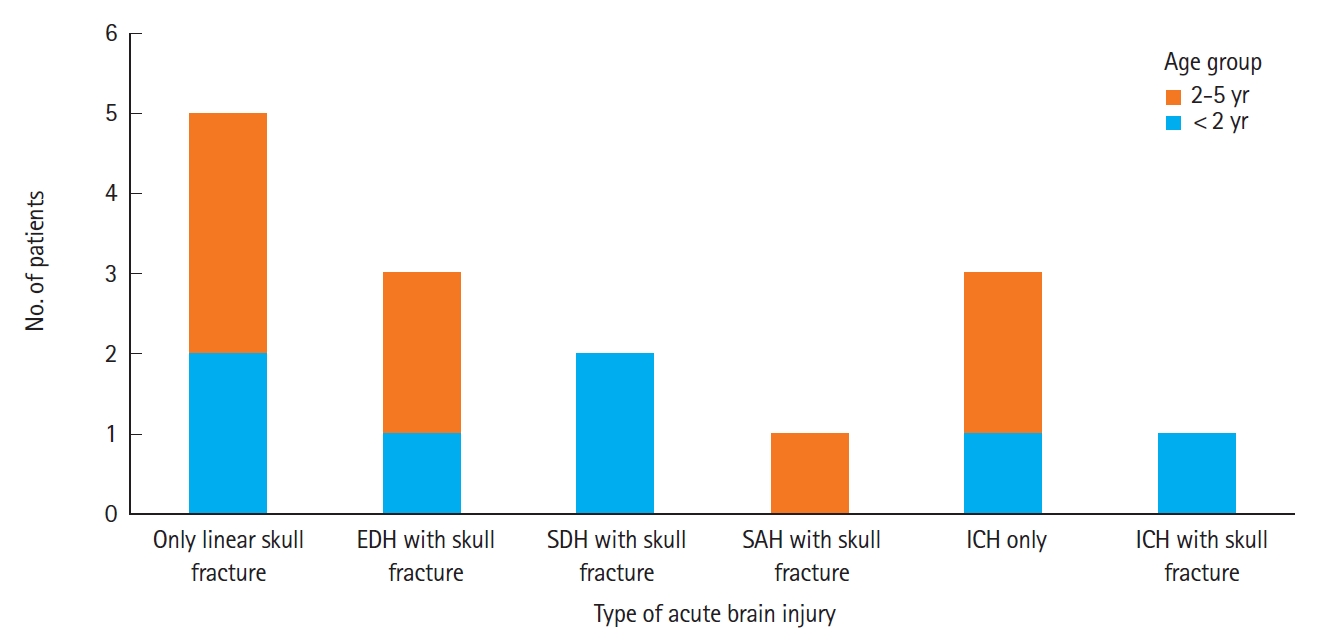
Table 1.Patients’ characteristics subdivided into age groups Table 2.Predictors of clinically important traumatic brain injury Table 3.Test performance of the PECARN and CATCH2 rules (<2 years old group) Table 4.Test performance of the PECARN and CATCH2 rules (2–5 years old group) Table 5.Test performance of the PECARN and CATCH2 rules (0–5 years old group) |
|
|||||||||||||||||||||||||||||||||||||||||