AbstractObjectiveTo evaluate the prognostic factors associated with the sustained return of spontaneous circulation (ROSC) and survival to hospital discharge in traumatic out-of-hospital cardiac arrest (TOHCA) patients without prehospital ROSC.
MethodsWe analyzed Korean nationwide data from the Out-of-Hospital Cardiac Arrest Surveillance, and included adult TOHCA patients without prehospital ROSC from January 2012 to December 2016. The primary outcome was sustained ROSC (>20 minutes). The secondary outcome was survival to discharge. Multivariate analysis was performed to investigate factors associated with the outcomes of TOHCA patients.
ResultsAmong 142,905 cases of OHCA, 8,326 TOHCA patients were investigated. In multivariate analysis, male sex (odds ratio [OR], 1.326; 95% confidence interval [CI], 1.103ŌĆō1.594; P=0.003), and an initial shockable rhythm (OR, 1.956; 95% CI, 1.113ŌĆō3.439; P=0.020) were significantly associated with sustained ROSC. Compared with traffic crash, collision (OR, 1.448; 95% CI, 1.086ŌĆō1.930; P=0.012) was associated with sustained ROSC. Fall (OR, 0.723; 95% CI, 0.589ŌĆō0.888; P=0.002) was inversely associated with sustained ROSC. Male sex (OR, 1.457; 95% CI, 1.026ŌĆō2.069; P=0.035) and an initial shockable rhythm (OR, 4.724; 95% CI, 2.451ŌĆō9.106; P<0.001) were significantly associated with survival to discharge. Metropolitan city (OR, 0.728; 95% CI, 0.541ŌĆō0.980; P=0.037) was inversely associated with survival to discharge. Compared with traffic crash, collision (OR, 1.745; 95% CI, 1.125ŌĆō2.708; P=0.013) was associated with survival to discharge.
INTRODUCTIONOut-of-hospital cardiac arrest (OHCA) is the leading etiology of mortality and an increasing concern in public health care [1,2]. Compared with the victims of cardiac arrest with cardiac origins, patients with traumatic cardiac arrest generally have worse outcomes. Even with medical improvements, the rate of survival to discharge for patients with traumatic out-of-hospital cardiac arrest (TOHCA) tends to be lower [3-5]. Recent studies of data from prospectively registered trauma systems have reported survival rates of traumatic cardiac arrest comparable to those for out-of-hospital medical cardiac arrest, ranging from 5.7% to 7.5% [6-8]. However, the reasons for this increase in survival from TOHCA are unclear.
The outcomes of patients with OHCA are associated with multiple variables, including age, comorbidities, initial rhythm recorded on the monitor, and the return of spontaneous circulation (ROSC) [9]. Among these variables, the most influential factor associated with survival from OHCA is ROSC in the field, regardless of the subsequent in-hospital treatment [2]. TOHCA is a fundamentally different disease process compared to non-traumatic cardiac arrest that is largely of primary cardiac etiology [10]. Therefore, prognostic factors of non-traumatic and traumatic cardiac arrest outcome could be different. In addition to the mechanism of trauma, the other determinants of survival identified could be the magnitude of neurological injury incurred during resuscitation [11]. Additionally, the neurological injury of TOHCA patients without prehospital ROSC could be more severe than that of TOHCA patients with prehospital ROSC. However, the prognostic factors for TOHCA patients without prehospital ROSC remain unclear.
This study aimed to evaluate the prognostic factors associated with sustained ROSC and survival to hospital discharge in patients without prehospital ROSC after TOHCA.
METHODSStudy design, setting, and populationThis retrospective observational study investigated all adult patients with TOHCA (18 years and older) admitted to the emergency department (ED) by using nationwide data from the Out-of-Hospital Cardiac Arrest Surveillance (OHCAS) of the Korean Centers for Disease Control and Prevention (KCDC) from January 2012 to December 2016. OHCAS was conducted in 17 provinces of South Korea (about 50 million people) and contained patient information from the moment of cardiac arrest to outcomes at hospital discharge. From January 2012 to December 2016, 142,905 OHCA patients were registered in the OHCAS. Among them, patients with OH CA were excluded from the study on the basis of any non-traumatic cause, age younger than 18 years, do-not-resuscitate order, death on arrival, prehospital ROSC, unknown mechanism of trauma, invalid data on ROSC status or survival data, and any missing variables.
The Kangnam Sacred Heart Hospital Institutional Review Board approved this study in 2019 (institutional review board approval no. 2019-07-003), and the need for informed consent was waived because of the retrospective nature of the study and the use of anonymous clinical data for the analysis. The KCDC approved the use of the data for this study. The methodology of this study was consistent with the STROBE checklist for observational studies.
Data collectionThe OHCAS is a population-based, emergency medical service (EMS)-assessed OHCA registry and retrospective patient cohort. Information about the patients with OHCA was obtained from the EMS records entered by EMS providers immediately after the transport of these patients, and the data of patients with OHCA for hospital care and outcomes at hospital discharge were provided by the KCDC. Medical record reviewers of KCDC visited all EDs and hospitals to where the patients with OHCA were transported and reviewed the medical records.
The OHCAS included information about the patients and the mechanism of trauma, place of cardiopulmonary resuscitation (CPR), bystander CPR, ROSC, procedures during transportation, and survival to hospital discharge using an appropriately devised survey form.
VariablesInformation on demographic factors (age and sex), geographical factors of the OHCA (metropolitan city versus non-metropolitan city), places of CPR (public places versus non-public places), initial cardiac rhythm (shockable versus non-shockable), hospital cardiac rhythm (shockable versus non-shockable), witnessed cardiac arrest, bystander CPR, time interval from CPR to ED arrival, and mechanism of trauma was collected. Metropolitan city is defined as any city with more than one million people and first-level administrative division within South Korea. There are eight first-level cities in South Korea: Busan, Daegu, Daejeon, Gwangju, Incheon, Sejong, Seoul, and Ulsan.
TOHCA was defined as cardiac arrests caused by traumatic events at the scene or prehospital phase, including traffic crash, fall, collision, stab injury, and gunshot injury. Traffic crash was defined as any damages related to transportation, such as automobile and motorbike. Collision was defined as any damage caused by colliding with object, being trapped between objects, or striking. Detailed classification of the cause of traumatic cardiac arrest is described in Supplementary Table 1.
Public places were defined as the places generally open and near to people, such as roads, public buildings, and commercial facilities. Detailed classification of cardiac arrest is summarized in Supplementary Table 2. A shockable rhythm was defined as ventricular fibrillation or pulseless ventricular tachycardia. Sustain ed ROSC was defined as spontaneous rhythm that was sustained for >20 minutes. The interval from cardiac arrest to ED arrival was defined as the time from EMS calling for TOHCA to ED arrival of patients.
OutcomesThe primary outcome of this study was sustained ROSC, and the secondary outcome was survival to discharge of patients with TOHCA.
Statistical analysisThe data including demographic characteristics between the sustained ROSC and non-sustained ROSC groups, and survival to discharge and non-survival groups are presented as a median and interquartile range (IQR) for continuous data or as a frequency and percentage for categorical data. The normality of each continuous variable was assessed using the Kolmogorov-Smirnov test. The independent sample t-test was used to analyze parametric data, Mann-Whitney U-test was used to analyze nonparametric continuous data, and Pearson chi-square or Fisher exact test was used to analyze categorical variables.
The model of multivariate logistic regression was stepwise backward elimination. Any variables with a P-value <0.05 in univariate analyses were included in the multivariate regression analysis. All statistical analysis was conducted with IBM SPSS ver. 20.0 (IBM Corp., Armonk, NY, USA) and R package ver. 3.3.2 (R Foundation for Statistical Computing, Vienna, Austria), and P<0.05 was considered statistically significant.
RESULTSCharacteristics of the study patientsOf 142,905 OHCA patients who were registered during the study period, we excluded patients for the following reasons: non-traumatic cause (n=127,400), age <18 years (n=2,857), do-not-resuscitate or death on arrival (n=3,409), prehospital ROSC (n=624), unknown mechanism of trauma (n=241), and unknown ROSC or survival at hospital discharge (n=48) (Fig. 1). The remaining 8,326 patients were finally enrolled in this study.
Table 1 summarizes the clinical characteristics of patients in the non-sustained ROSC and sustained ROSC groups. The percentages of male patients (70.6% vs. 76.4%, P<0.001) and witnessed cardiac arrests (39.6% vs. 45.8%, P<0.001) were significantly higher in the sustained ROSC group than in the non-sustained ROSC group. The time interval from cardiac arrest to ED arrival (22 minutes; IQR, 15ŌĆō30 minutes) in the sustained ROSC group was significantly shorter than the median prehospital length of CPR (24 minutes; IQR, 18ŌĆō34 minutes) in the non-sustained ROSC group (P<0.001), and the mechanism of trauma differed significantly between the non-sustained ROSC and sustained ROSC groups (P<0.001).
Table 2 summarizes the clinical characteristics of patients in the non-survival and survival to discharge groups. The percentages of male patients (71.8% vs. 79.4%, P<0.001), TOHCAs in public places (65.4% vs. 69.6%, P=0.028), initial shockable rhythms (1.0% vs. 2.5%, P<0.001), and hospital shockable rhythms (0.8% vs. 1.8%, P<0.013) were significantly higher in the survival to discharge group than in the non-survival group. The percentage of TOHCAs in a metropolitan city was significantly lower in the survival to discharge group than in the non-survival group (37.6% vs. 32.5%, P=0.008). The mechanism of trauma differed significantly between the non-survival and survival to discharge groups (P<0.001).
Prognostic factors for sustained ROSC of patients with TOHCAAfter multivariate logistic regression analysis, male sex (odds ratio [OR], 1.326; 95% confidence interval [CI], 1.103ŌĆō1.594; P=0.003) and an initial shockable rhythm (OR, 1.956; 95% CI, 1.113ŌĆō3.439; P=0.020) were significantly associated with sustained ROSC. Regarding the mechanism of trauma, collision (OR, 1.448; 95% CI, 1.086ŌĆō1.930; P=0.012) was associated with sustained ROSC compared with traffic crash. Fall (OR, 0.723; 95% CI, 0.589ŌĆō0.888; P=0.002) was inversely associated with sustained ROSC compared with traffic crash (Table 3).
Prognostic factors for survival to discharge of patients with TOHCAAfter multivariate logistic regression analysis, male sex (OR, 1.457; 95% CI, 1.026ŌĆō2.069; P=0.035) and an initial shockable rhythm (OR, 4.724; 95% CI, 2.451ŌĆō9.106; P<0.001) were significantly associated with survival to discharge. Metropolitan city (OR, 0.728; 95% CI, 0.541ŌĆō0.980; P=0.037) was inversely associated with survival to discharge. Concerning the mechanism of trauma, collision (OR, 1.745; 95% CI, 1.125ŌĆō2.708; P=0.013) was associated with ROSC compared with traffic crash (Table 3) [6].
DISCUSSIONWe analyzed nationwide data to identify prognostic factors associated with sustained ROSC and survival to discharge in adult TOHCA patients without prehospital ROSC. Regarding sustained ROSC, male sex and an initial shockable rhythm were favorable factors, and collision as a mechanism of trauma was a favorable prognostic factor for ROSC compared with traffic crash. However, fall was an unfavorable prognostic factor for ROSC compared with traffic crash. Concerning survival to discharge, male sex, and an initial shockable rhythm were favorable factors, but metropolitan city was an unfavorable factor. Regarding the mechanism of trauma, collision was a favorable factor for survival to discharge compared with traffic crash.
The survival rate in our study is higher than that reported in a recent large-scale study in North America that used data from two registry systems, but this difference was due to the measurement time of survival and rate of gunshot injury. The survival rate in this study was only measured at hospital discharge, not at 30 days after hospital discharge, and our study had a very low rate (0.1%) of gunshot injury compared to the North American study [6]. Our study also demonstrated that 2,654 (31.9%) patients had sustained ROSC during ED resuscitation, although they did not have prehospital ROSC, and sustained ROSC was defined as ROSC >20 minutes. The rate of sustained ROSC in our study was higher than that in a nationwide population-based study in Qatar (14.9%) [12]. However, the rate was comparable to that of sustained ROSC in patients with TOHCA in other studies and ranged from 19.6% to 31.4% [13-15]. These findings suggest that the resuscitation attempts in TOHCA patients without prehospital ROSC may be beneficial. However, the outcomes of TOHCA could be influenced by several factors, including the interval between the collapse and ED arrival, place of cardiac arrest, cardiac rhythm, and mechanism of trauma.
Unlike previous TOHCA studies in which male sex had no or a negative association with ROSC or survival to discharge [11,16], male sex was a favorable factor for ROSC and survival to discharge in our study. The association between male sex and higher rate of sustained ROSC and survival to discharge remains unclear. However, this difference could be partially explained by the result of a recent study of OHCA in which female patients had lower chances than male patients to be resuscitated by a bystander and lower rate of an initial shockable rhythm [17].
In our study, metropolitan city was an unfavorable factor for survival to discharge. Cardiac arrests that occurred in rural locations were less likely witnessed by bystanders and approached by EMSs, causing delayed hospital transportation and resuscitation. There is a significantly lower rate of survival among patients in areas lacking medical resources. This lower survival rate could be caused by various levels of medical resources in different areas [16]. Nevertheless, the pathophysiology of TOHCA is different depending on the medical causes of cardiac arrest, and different treatment priorities may be needed [18]. Traffic injury was the leading mechanism of TOHCA, and traffic injury in a metropolitan city was likely to be associated with more severe traumatic injury, which may need more medical care and interventions, compared with traffic injury in a non-metropolitan city [16]. Therefore, patients with TOHCA in a metropolitan city could have less chance of survival to discharge than patients with TOHCA in a non-metropolitan city.
Our results demonstrated that an initial shockable rhythm was a remarkable factor of the outcome. Consistent with several previous studies, cardiac arrest patients with shockable rhythm had better survival than those without it [19,20]. Wolbinski et al. [21] reported that OHCA patients with shockable presentations had a much higher survival rate than those without it (27% vs. 1%). Because a shockable rhythm was recorded in only 3% of total traumatic patients with OHCA compared with 17.1% of medical patients with OHCA, the survival rate of traumatic patients with OHCA was significantly lower [4]. Even though 11.4% of patients who achi eved spontaneous circulation on admission presented with an initial shockable rhythm, the proportion of shockable rhythm was elevated to 25% among the patients who survived to discharge [12]. This phenomenon was consistent with our findings that TOHCA patients with survival to discharge had a higher proportion of shockable rhythm than those without survival to discharge (2.5% vs. 1.0%). The underlying mechanism of the higher rate of shockable rhythm among TOHCA patients with survival to discharge remains unclear. However, Georgescu et al. [22] revealed that one-third of traumatic patients with OHCA also presented with cardiovascular injuries or lesions, which is a reasonable explanation for our finding. It is very possible that cardiac problems increased the rate of shockable rhythm among patients with TOHCA. Consequently, an initial shockable rhythm played an important role in improving the survival to discharge of patients with TOHCA in this study.
In terms of the mechanism of trauma, traffic crash was the leading cause of OHCA in this study. This finding corresponds with the results of other TOHCA studies that identified traffic crash as the most common cause of trauma [6,12]. However, the proportion of TOHCAs due to traffic crash was less in a North American study (28%ŌĆō24%). Additionally, while gunshot wound (24%ŌĆō26%) was the second leading cause of injuries in North America, it was a rare cause of traumatic cardiac arrest in our study [6].
In the multivariate logistic analysis for sustained ROSC and survival to discharge, compared with traffic crashes, collision was associated with a higher possibility of sustained ROSC and survival to discharge of patients with TOHCA, and these findings are similar to those of previous studies [16]. However, unlike previous TOHCA-related studies in which fall was associated with a higher possibility of survival to discharge, fall was not associated with sustained ROSC and survival to discharge compared with traffic crash in our study. This difference may be because only TOHCA patients without prehospital ROSC were included in this study, and such patients could have a more severe traumatic injury than those in the previous TOHCA-related studies.
Our study has several limitations. First, since this was a retrospective observational study, it may have been subject to selection bias relating to ROSC and survival. Second, we could not assess the survival rate beyond hospital discharge because the survival rate was measured using data from the patientsŌĆÖ medical records at hospital discharge. Therefore, a longer survival outcome, such as 30-day mortality, could be different from the outcomes of this study. Third, our retrospective registry did not contain data that described potential confounders, e.g., the patientsŌĆÖ underlying diseases, hemodynamic statuses, and hemorrhage control. These factors could affect patient ROSC and survival to discharge. Thus, more studies that include more variables related to the patientsŌĆÖ statuses are required to corroborate our results. Fourth, whether our studyŌĆÖs findings can be generalized to other countries with different medical systems is uncertain. The study was performed in the context of South KoreaŌĆÖs EMS, which does not permit the provision of advanced cardiac life support to patients. Hence, the findings from this study should be interpreted with caution with regard to their generalizability to other countriesŌĆÖ medical systems that provide advanced cardiac life support to patients. Fifth, EMS-witnessed cardiac arrest and hemorrhage control were significant factors that affect the outcome of TOHCA [12,23]. However, these factors were not evaluated in this study. Therefore, the outcome of TOHCA in this study could be different if the EMS-witnessed TOCHA and hemorrhage control were identified. Finally, procedures performed by EMS during transportation, such as airway management, applying a splint or cervical collar, or adre naline administration, were not assessed in this study. These procedures might be significant factors that affect the outcome of TOHCA. Therefore, the outcome of TOHCA in this study could be different if the procedures done by EMS were identified.
In conclusion, male sex, an initial shockable rhythm, and collision could be favorable factors associated with sustained ROSC. In contrast, patients with fall as a cause of trauma compared with traffic crash could be less likely to have sustained ROSC. Survival to discharge might be higher among patients who are men, reside in a non-metropolitan city, have an initial shockable rhythm, or have collision as a cause of trauma compared with traffic crash. Nevertheless, these results should be cautiously interpreted considering the possible biases. Further nationwide studies will be needed to measure the long-term outcome, and they should include in-hospital data of patients.
SUPPLEMENTARY MATERIALSupplementary Tables are available from: https://doi.org/10.15441/ceem.19.057.
REFERENCES1. Kitamura T, Iwami T, Kawamura T, et al. Nationwide public-access defibrillation in Japan. N Engl J Med 2010; 362:994-1004.
2. Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes 2010; 3:63-81.
3. Chien CY, Su YC, Lin CC, Kuo CW, Lin SC, Weng YM. Is 15 minutes an appropriate resuscitation duration before termination of a traumatic cardiac arrest? A case-control study. Am J Emerg Med 2016; 34:505-9.
4. Beck B, Tohira H, Bray JE, et al. Trends in traumatic out-of-hospital cardiac arrest in Perth, Western Australia from 1997 to 2014. Resuscitation 2016; 98:79-84.
5. Zwingmann J, Mehlhorn AT, Hammer T, Bayer J, Sudkamp NP, Strohm PC. Survival and neurologic outcome after traumatic out-of-hospital cardiopulmonary arrest in a pediatric and adult population: a systematic review. Crit Care 2012; 16:R117.
6. Evans CC, Petersen A, Meier EN, et al. Prehospital traumatic cardiac arrest: Management and outcomes from the resuscitation outcomes consortium epistry-trauma and PROPHET registries. J Trauma Acute Care Surg 2016; 81:285-93.
7. Barnard E, Yates D, Edwards A, Fragoso-Iniguez M, Jenks T, Smith JE. Epidemiology and aetiology of traumatic cardiac arrest in England and Wales: a retrospective database analysis. Resuscitation 2017; 110:90-4.
8. Leis CC, Hernandez CC, Blanco MJ, Paterna PC, Hernandez Rde E, Torres EC. Traumatic cardiac arrest: should advanced life support be initiated? J Trauma Acute Care Surg 2013; 74:634-8.
9. Nielsen N. Predictive scores, friend or foe for the cardiac arrest patient. Resuscitation 2012; 83:669-70.
10. Hayashi M, Shimizu W, Albert CM. The spectrum of epidemiology underlying sudden cardiac death. Circ Res 2015; 116:1887-906.
11. Barnard EBG, Sandbach DD, Nicholls TL, Wilson AW, Ercole A. Prehospital determinants of successful resuscitation after traumatic and non-traumatic out-of-hospital cardiac arrest. Emerg Med J 2019; 36:333-9.
12. Irfan FB, Consunji R, El-Menyar A, et al. Cardiopulmonary resuscitation of out-of-hospital traumatic cardiac arrest in Qatar: a nationwide population-based study. Int J Cardiol 2017; 240:438-43.
13. Goto Y, Maeda T, Nakatsu-Goto Y. Neurological outcomes in patients transported to hospital without a prehospital return of spontaneous circulation after cardiac arrest. Crit Care 2013; 17:R274.
14. Konesky KL, Guo WA. Revisiting traumatic cardiac arrest: should CPR be initiated? Eur J Trauma Emerg Surg 2018; 44:903-8.
15. Beck B, Bray JE, Cameron P, et al. Predicting outcomes in traumatic out-of-hospital cardiac arrest: the relevance of Utstein factors. Emerg Med J 2017; 34:786-92.
16. Lai CY, Tsai SH, Lin FH, et al. Survival rate variation among different types of hospitalized traumatic cardiac arrest: a retrospective and nationwide study. Medicine (Baltimore) 2018; 97:e11480.
17. Blom MT, Oving I, Berdowski J, van Valkengoed IGM, Bardai A, Tan HL. Women have lower chances than men to be resuscitated and survive out-of-hospital cardiac arrest. Eur Heart J 2019; ehz297.
18. Tarmey NT, Park CL, Bartels OJ, Konig TC, Mahoney PF, Mellor AJ. Outcomes following military traumatic cardiorespiratory arrest: a prospective observational study. Resuscitation 2011; 82:1194-7.
19. Arrich J, Sterz F, Fleischhackl R, et al. Gender modifies the influence of age on outcome after successfully resuscitated cardiac arrest: a retrospective cohort study. Medicine (Baltimore) 2006; 85:288-94.
20. Kitamura T, Iwami T, Kawamura T, et al. Nationwide improvements in survival from out-of-hospital cardiac arrest in Japan. Circulation 2012; 126:2834-43.
21. Wolbinski M, Swain AH, Harding SA, Larsen PD. Out-of-hospital cardiac arrest patient characteristics: comparing ventricular arrhythmia and pulseless electrical activity. Heart Lung Circ 2016; 25:639-44.
Fig.┬Ā1.Flow diagram of the study population. OHCA, out-of-hospital cardiac arrest; DNR, do not resuscitate; DOA, death on arrival; ROSC, return of spontaneous circulation. 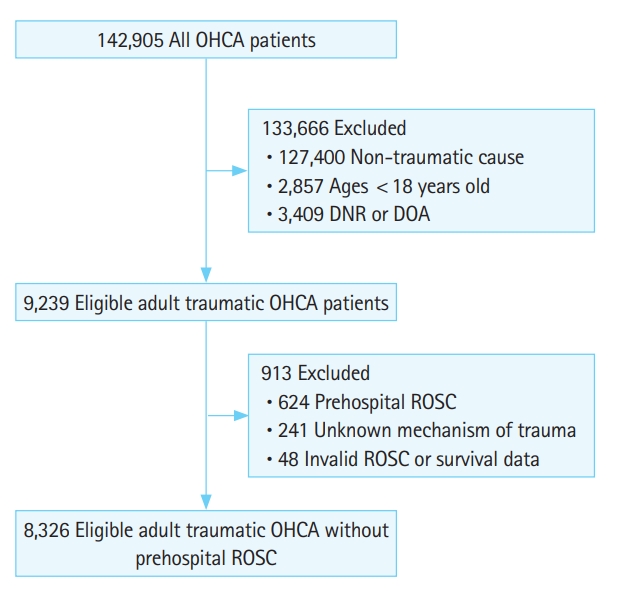
Table┬Ā1.Basic characteristics of TOHCA patients with and without sustained ROSC
Table┬Ā2.Basic characteristics of TOHCA patients with non-survival and survival to discharge
Table┬Ā3.Multivariate logistic analysis of sustained ROSC and survival to discharge
|
|