INTRODUCTION
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causing coronavirus disease 2019 (COVID-19) was first reported in China in December 2019. Subsequently, it was declared as a pandemic by the World Health Organization in March 2020, and the global burden of COVID-19 was reported as 37,888,384 cases and 1,081,868 deaths as of October 14, 2020 [1].
While most COVID-19-related clinical conditions are associated with the respiratory system, cardiovascular involvement is also common and related to high mortality rates among hospitalized patients [2]. Previous studies have reported that SARS-CoV-2 can cause myocardial injury and elevated troponin levels [3]. However, it has been suggested that the myocardial injury is related to the systemic effects of COVID-19, rather than direct damage to the cardiac tissue [3]. A limited number of case reports have demonstrated myopericarditis in patients with COVID-19.
We report a case of COVID-19-associated myopericarditis and review the current literature to increase emergency physiciansŌĆÖ awareness of COVID-19-associated myopericarditis as they care for patients with COVID-19.
CASE REPORT
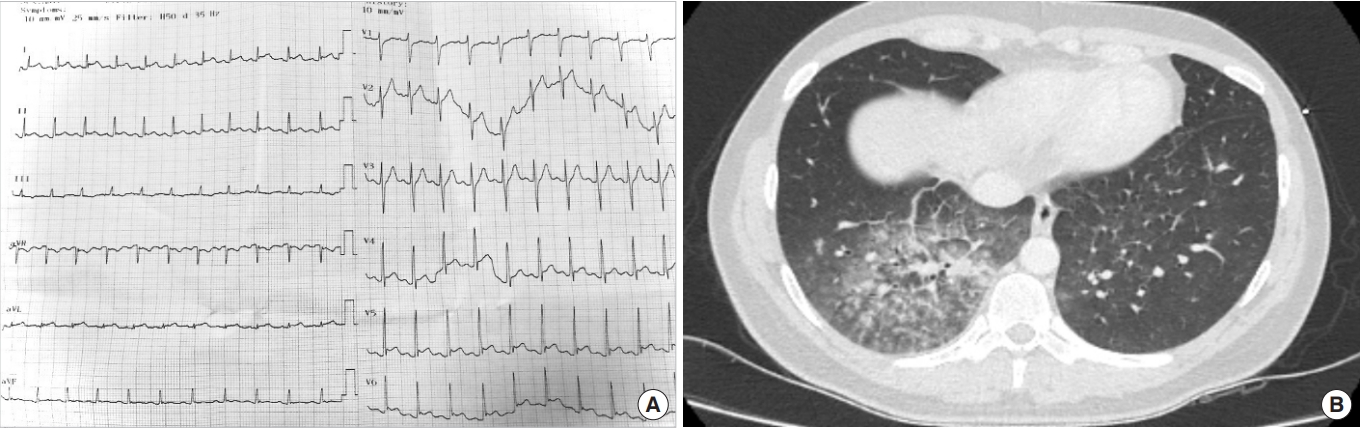
A 25-year-old man presented to the emergency department (ED) with acute onset chest pain and shortness of breath (SOB). The patientŌĆÖs medical history was unremarkable; however, the patient had a 4-day history of progressive fatigue and fever. In the ED, the patientŌĆÖs blood pressure was 130/80 mmHg, heart rate was 140 beats per minute, oxygen saturation was 98% in room air, and temperature was 37.1┬░C. A physical examination revealed tachycardia and coarse crackles in the both lower lung zones. An electrocardiogram (ECG) showed sinus tachycardia with ST segment elevation and PR depression in leads I, aVL, V5, and V6 and ST depression and PR elevation in aVR (Fig. 1A). The initial laboratory work-up revealed leukocytosis, lymphopenia, and elevated troponin (21.471 ng/mL; normal range, 0ŌĆō60 ng/mL). An echocardiogram demonstrated diffuse left ventricular hypokinesia with an ejection fraction of 35% and a pulmonary artery pressure of 30 mmHg. Consolidation and ground-glass opacities suggesting viral infection were detected in the right lower lobe on chest computed tomography (Fig. 1B). The patient was transferred to the cardiac care unit with the suspicion of COVID-19-related myopericarditis. Although the initial polymerase chain reaction testing for SARS-CoV-2 was negative, considering the high clinical suspicion of COVID-19, the patient was kept under isolation and empirical antibiotics, antivirals, and supportive therapy were initiated, including ampicillin-sulbactam (1.5 g four times a day), clarithromycin (500 mg twice a day), oseltamivir (75 mg twice a day), acetylsalicylic acid (81 mg once a day), and metoprolol (50 mg twice a day). An emergency coronary angiography was not performed as the patientŌĆÖs clinical condition was attributed to the viral infection. The patientŌĆÖs sputum, blood, and urine cultures were negative. The patient was treated in the cardiac care unit for 8 days, during which his laboratory and radiological findings normalized (Table 1). An echocardiogram showed a left ventricular ejection fraction of 55% prior to discharge. Antibody testing for COVID-19 was positive on the 8th day of hospitalization. The patient provided written informed consent for this report.
DISCUSSION
Myopericarditis is a challenging diagnosis encountered in the ED. Although it should be suspected in any patients with chest pain, increased troponin levels, and dynamic ECG changes, these findings are non-specific and can also be seen in patients with systemic infections, including those with COVID-19 [4]. The cardiovascular complications of COVID-19 have been previously reported [2]; however, reports of patients presenting to the ED with the suspicion of COVID-19-related myopericarditis are scarce.
Most patients with COVID-19 present to the ED with fever, cough, and SOB [5]. The presentation of patients with COVID-19ŌĆōassociated myopericarditis can be non-specific. To date, only a few cases of myocarditis or myopericarditis associated with COVID-19 have been reported in the literature [6-15]. The most common symptoms at presentation included SOB (6/10 cases) [6,9,11,13-15], chest pain (6/10 cases) [6,10-12,14,15], and fever (5/10 cases) [6,8-10,13]. However, diarrhea (4/10 cases) [8,9,13,15], fatigue (2/10 cases) [7,12], and cough (2/10 cases) [8,9] have also been reported (Supplementary Table 1). Therefore, even without chest pain or other common symptoms, COVID-19 can present with myopericarditis.
Cardiac biomarkers such as troponin or N-terminal pro-B-type natriuretic peptide (NT-proBNP) were elevated in patients with myopericarditis [2]. Previous studies reported that both troponin and NT-proBNP were simultaneously elevated in patients with COVID-19 and myopericarditis [6-8,10,11,13,15]. Therefore, these cardiac biomarkers should be tested in patients suspected of having COVID-19ŌĆōassociated myopericarditis. In this patient, NT-proBNP was not tested due to echocardiographic findings supporting the diagnosis.
Utilizing echocardiography as an initial diagnostic workup in the ED may facilitate the care of patients with myopericarditis [2]. Although cardiac magnetic resonance imaging is widely used to diagnose myopericarditis, it is not a feasible diagnostic tool in the ED. The most common echocardiographic findings are myocardial dyskinesia with a decreased left ventricular ejection fraction [6-8,10,11,13,15]. In this report, the patient had an initial left ventricular ejection fraction of 35% and diffuse myocardial hypokinesia, which were improved at the time of discharge.
In conclusion, myopericarditis is an insidious condition that can accompany COVID-19. Emergency physicians should consider myopericarditis as an important differential diagnosis for patients with COVID-19.