AbstractObjectiveThis study aimed to evaluate the association between the number and level of emergency medical technicians (EMTs) in the first-contact emergency medical services (EMS) unit and the clinical outcomes of out-of-hospital cardiac arrest (OHCA) with a dual dispatch response.
MethodsAdult nontraumatic EMS-treated OHCAs between 2015 and 2018 in a nationwide database, were enrolled. The main exposure was the number and certification level of first-contact EMS crew: three versus two members, proportion of EMT intermediate level (EMT-I) over 50% versus under or equal to 50%. Good neurologic recovery was selected as the primary outcome. Multilevel multivariable logistic regression analysis was conducted to calculate adjusted odds ratios and confidence intervals.
ResultsA total of 26,867 patients were enrolled and analyzed. Good neurologic recovery was different across the study groups: 5.4% in the two-member crews, 7.2% in the three-member crews, 5.9% in the low EMT-I proportion crews, and 6.8% in the high EMT-I proportion crews. In the main analysis, statistically significant differences for favorable outcomes were found between the three-member and two-member crews, and the high EMT-I proportion and low EMT-I proportion crews; for good neurologic recovery, adjusted odds ratios (95% confidence interval) were 1.23 (1.06ŌĆō1.43) for three-member crews, and 1.28 (1.17ŌĆō1.40) for a high EMT-I proportion.
INTRODUCTIONOut-of-hospital cardiac arrest (OHCA) is a major public health concern [1,2]. OHCA incidence increases every year, and the worldwide survival rate remains at approximately 10% [3-5]. Many studies have been conducted to improve OHCA outcomes, and rapid defibrillation, a short ambulance response time, and high-quality cardiopulmonary resuscitation (CPR) have been found to be core elements in prehospital resuscitation [6-9].
A dual dispatch response (DDR) system of emergency medical services (EMS), which dispatches multiple vehicles to the scene, has been applied in many countries to improve outcomes [10,11]. Dispatching multiple vehicles to a scene is associated with shorter EMS response time, which is the elapsed time interval between EMS activation and ambulance scene arrival, and a better prognosis [11-13]. Additionally, early defibrillation and a higher defibrillation rate are the other positive effects of multiple vehicle dispatch on clinical outcomes [14-16]. DDR has been shown to increase the number of on-scene EMS personnel, leading to better quality CPR and application of advanced procedures that improve survival outcomes [17,18].
The number and certification level of on-scene emergency medical technicians (EMTs) have been evaluated for their impact on OHCA outcomes. Higher number of EMTs and a higher ratio of high-level EMTs at the scene have been associated with better survival outcomes [18-20]. Tsai et al. [21] reported that a larger number of EMTs is needed to provide optimal teamwork performance and advanced procedures. However, other studies found no significant association between the number of EMS crew members and clinical outcomes [22-25], thus, this effect remains controversial.
In a DDR setting, EMS units are divided into first-contact and second-contact teams according to arrival time. A short response time and earlier advanced life support by the second EMS unit have been found to be associated with better outcomes [26,27]. However, the effect of the number and certification level of EMTs in the first-contact EMS unit have not been well evaluated. The purpose of this study was to evaluate the association between the number and level of EMTs in first-contact EMS units and the clinical outcomes of DDR-activated OHCA. We hypothesized that a higher number of EMS personnel and higher certification level proportion are associated with favorable outcomes.
METHODSEthics statementThis study complied with the Declaration of Helsinki, and its protocol was approved by the Institutional Review Board of Seoul National University Hospital with a waiver of informed consent (No. 1103-153-357).
Study design and data sourcesThis study is a retrospective observational cohort study based on a nationwide, prospective OHCA database in Korea from January 2015 to December 2018. This database system was developed in 2006 with the cooperation of the National Fire Agency and the Korea Centers for Disease Control and Prevention. In the database, EMS run-sheets and cardiac arrest registries that were recorded by the EMS crew immediately after OHCA transport and hospital record reviews collected by trained medical record reviewers were integrated. For DDR-activated cases, an additional multitier activation registry was filled out by the EMS crew or firefighters who did not transport victims.
Study settingKorea, which has approximately 50 million residents within a land area of 100,210 km2, has a government-operated EMS system. Under the National Fire Agency, a total of 17 provincial fire headquarters administer approximately 200 fire stations and 8,400 EMS personnel. For emergency calls, ambulances that are assigned to the EMS agencies belonging to the fire stations are dispatched from the headquartersŌĆÖ dispatch centers [28]. The primary call dispatcher asks questions about altered mental status and abnormal breathing to identify cardiac arrest. For suspected OHCA, the call is passed to a medical call dispatcher to give CPR instructions [29]. The EMS CPR protocol at the scene and in the ambulance follows the American Heart Association guidelines [30]. Korean EMS workers provide basic-to-intermediate levels of intervention, including intravenous fluid administration and advanced airway management under physician-direct medical oversight. Because EMS crew members cannot pronounce a declaration of death, all EMS-treated OHCAs must be transported to the nearest emergency department (ED). EDs are designated as levels 1, 2, and 3 by the Ministry of Health and Welfare based on the case volume and quality of resources. Level 1 and 2 EDs must be staffed by emergency physicians 24/7 and have more resources.
DDR systemSince 2015, a DDR system has been implemented nationwide for suspected OHCA cases in Korea. The dispatcher asks two key questions for identification, consciousness, and respiration, and considers OHCA if both responses are abnormal. When the dispatcher suspects OHCA and activates DDR, a nearby ambulance and an additional available ambulance or fire engine could be dispatched. Ambulance selection is based on distance proximity only for both first-contact and second-contact EMS units, regardless of the number of EMS crews or certification level available. Each fire engine has two first responders, equivalent to emergency medical responder in United States, and provides a basic life support level of resuscitation with automated external defibrillators only. There are two certification levels of EMTs in the ambulance: EMT basic level (EMT-B) and EMT intermediate level (EMT-I). EMT-I can perform advanced airway and intravenous management under direct medical oversight. EMS providers with a nurseŌĆÖs license perform the same scope of work as EMT-I. The first arriving EMS crew starts chest compressions immediately and provides defibrillation when necessary. Advanced cardiovascular life support (ACLS) is provided when resources are sufficient because there is no definite protocol for ACLS timing. The first-contact EMS crew decides whether to activate DDR in cases where the victimŌĆÖs OHCA status was not recognized by the dispatcher.
Study populationEMS-treated adult OHCA cases from January 2015 to December 2018 were enrolled. We excluded cases where the cardiac arrest was witnessed in the ambulance, without EMS time information, where only fire engines or a single ambulance was dispatched, and where two ambulances arrived simultaneously.
Outcome measuresThe primary outcome was good neurologic recovery, defined as cerebral performance category score 1 (no neurologic disability) or 2 (moderate disability, able to perform daily activities independently). Medical record reviewers determined patient scores based on discharge summary abstracts or physiciansŌĆÖ medical record notes. Survival to discharge and prehospital return of spontaneous circulation were used as the secondary outcomes, respectively.
Variables and measurementsThe main exposure of this study was the number and level of firstcontact EMS crew. The first-contact EMS team was identified based on scene arrival time variables in the OHCA database. There were two or three members in each ambulance, including the driver participating in resuscitation at the scene, and the EMS crew members were either EMT-B or EMT-I (Fig. 1).
Demographic findings and clinical information were collected and categorized: age (Ōēź65 years), sex, residential area (metropolitan area), location of cardiac arrest (public or private property), witnessed by bystander, bystander CPR, initial electrocardiogram rhythm (shockable), prehospital defibrillation, scene EMS management (advanced airway, intravenous access, and medication), EMS time interval (response time, scene time, and transport time), time interval between EMS unit arrivals (first-contact EMS unit and second-contact EMS unit), and level of ED (level 1, 2, or other).
Statistical analysesDescriptive analysis was conducted to compare the distribution of demographic findings and clinical information according to the number and level of first-contact EMS crew. The level of first-contact EMS crew were categorized according to whether the EMT-I ratio within the ambulance was greater than 50%. The Wilcoxon rank-sum test was used to compare continuous variables, and the chi-squared test was used for the categorical variables. Univariable and multivariable logistic regression analyses by number and level of first-contact EMS crew were conducted to calculate adjusted odds ratios (AORs) and confidence intervals (CIs). Considering the nested nature of EMS operations according to districts, a multilevel analysis with a series of random-intercept models by 17 provincial headquarters was applied. Potential confounders, including age group, sex, residential area, location of cardiac arrest, witness status, bystander CPR, initial electrocardiogram rhythm, prehospital defibrillation, response time interval, time interval between EMS unit arrivals, transport time interval, number and level of second-contact EMS crew, and level of ED were adjusted for in the model.
We assumed the effect of the number of first-contact EMS crews can differ depending on the level of EMS providers in the unit. Interaction analysis by EMT-I proportion across the number of first-contact EMS crews was performed. A P-value <0.05 was considered significant for all analyses. All statistical analyses were performed using SAS ver. 9.4 (SAS Institute Inc., Cary, NC, USA) and R ver. 3.5 (The R Foundation for Statistical Computing, Vienna, Austria).
RESULTSDemographic findingsAmong 112,999 EMS-treated OHCAs from 2015 to 2018, 26,867 victims were included in the final analyses. We excluded pediatric patients (n=2,391), traumatic OHCA (n=29,080), cardiac arrest witnessed in the ambulance (n=5,696), missing time variables (n=606), single dispatch response (n=36,614), fire engine dispatched (n=4,143), and no time difference between vehicles (n=7,602) (Fig. 2).
Table 1 describes the demographic findings and clinical information according to the number and level of first-contact EMS crew members. In DDR cases, patients treated by a lower number of EMS personnel or low EMT-I proportion crew in the first-contact EMS unit were more likely to live in nonmetropolitan areas, undergo bystander CPR, and were less likely to receive an advanced procedure by EMS providers. Good neurologic recovery showed significant differences according to the number and level of first-contact EMS crew: 5.4% in the two-member EMS crews, 7.2% in the three-member EMS providers, 5.9% in the proportion of EMT-I under or equal to 50%, and 6.8% in the proportion of EMT-I over 50% (Table 1).
Main analysesIn the multivariable logistic regression model, statistically significant differences for the following favorable outcomes were found between three-member and two-member first-contact EMS units: AORs (95% confidence interval [CI]), 1.23 (1.06ŌĆō1.43) for good neurologic recovery; 1.18 (1.07ŌĆō1.31) for survival to discharge; and 1.29 (1.21ŌĆō1.39) for prehospital return of spontaneous circulation (ROSC). EMT-I proportion over 50% showed a higher probability of favorable prognosis: AORs (95% CI), 1.28 (1.17ŌĆō1.40) for good neurologic recovery; 1.16 (1.08ŌĆō1.25) for survival to discharge; and 1.28 (1.17ŌĆō1.40) for prehospital ROSC (Table 2).
In the interaction analysis, EMT-I proportion equal or under 50% showed a positive interaction effect with three EMS providers for good neurologic recovery compared with two EMS providers in the first-contact EMS units: AORs (95% CI), 1.26 (1.02ŌĆō1.54) for good neurologic recovery in EMT-I equal or under 50%, and 1.07 (0.97ŌĆō1.18) in EMT-I over 50% (Table 3 and Fig. 3).
DISCUSSIONIn this study, we analyzed the association between the number and level of first-contact EMS crews and survival outcomes in DDRactivated OHCA. Statistically significant differences were found for good neurologic recovery, survival to discharge, and prehospital ROSC among the high number of EMS providers and high EMT-I proportion crews for first-contact EMS units. In the interaction analysis, the effect of a high number of EMS providers was strengthened by a low EMT-I proportion.
These results can be explained by the influence of a single EMS team resuscitation during the entire DDR phase. Even if an emergency call is suspected to be an OHCA by the dispatcher and DDR is activated, practical resuscitation provided before the secondcontact EMS crew arrives will be less effective than team-based resuscitation. The difference in CPR quality during that period would be strongly dependent on the number and level of EMS personnel, as found by Sun et al. [19] in a Taipei study. Although the total number of EMTs is thought to be sufficient in a DDR setting, during the early phase of field resuscitation prior to arrival of the second crew, the number of EMTs and their level of training may be critical.
Significant probabilities for favorable clinical outcomes have been found among crews with higher proportions of higher level EMTs (EMT-I). ACLS procedures, such as advanced airway management or epinephrine delivery, had potential associations with OHCA outcomes, especially short-term survival and prehospital ROSC [31,32]. In Korea, EMT-I can perform ACLS procedures at the scene, and high EMT-I proportion crews could deliver higher provision rates (Table 1).
We assumed that the magnitude of the effect of the number of first-contact EMS crew members would be strengthened by a higher proportion of EMT-I crew members. However, the magnitude of the difference between two and three EMS personnel in first-contact EMS unit increased according to a lower proportion of EMT-I, which suggests that the lower the level of the individuals in the team, the more effective the additional personnel are for prehospital resuscitation. Thus, it may be beneficial to increase EMS personnel, especially in regions with few high-level EMTs.
Based on our results, policy makers should consider allocating more human resources, including number and level of EMS providers, to regions where second-contact EMS units cannot arrive to the scene fast enough. Our findings indicate that the first-contact EMS unit responding to an OHCA should add additional crew as the first priority in conditions where there are only two EMT-Bs allocated. Similarly, a further interaction analysis by number of second-contact EMS crews showed that the effect of three members in first-contact EMS crew was strengthened when there were fewer EMS personnel in the second-contact ambulance (Supplementary Table. 1).
Reducing the response time of a relatively higher grade of EMS units would be important. Because it is mostly impossible to allocate the entire EMS unit to a maximum number and level, a dispatch protocol assigning suspected OHCA cases to a specific EMS unit can be considered. Currently, the Korean EMS system is operated in a nationwide universal dispatch protocol with DDR activation for suspected OHCA, in which the nearest EMS unit is sent as quickly as possible without consideration of the team characteristics. Table 1 showed that there is no significant difference in proportion of dispatcher recognition between the team characteristics.
The Korean government has been working to cultivate EMS staffing for many years, and the proportion of EMT-I and number of three-member EMS crews among first-contact EMS units is constantly increasing (Supplementary Fig. 1). It may be appropriate to consider categorizing EMS units according to their CPR performance and give priority to suspected OHCA cases. EMS units with more EMS providers and higher proportions of EMT-I should be on standby, and the other EMS units should have priority over dispatch to clear non-OHCA cases or as second-contact EMS crews in DDRs. The accuracy of dispatcher recognition of OHCA would also be important to evaluate.
This study has several limitations. First, main exposure was defined according to the number and certification level of the EMS crew, not by individual performance. To measure each crewŌĆÖs detailed resuscitative procedures, feedback devices and video records are needed, which were limited in our data sources. Similarly, quality of CPR and early defibrillation cannot be measured. Second, the number of crews in an EMS unit and the types of certification levels varies according to country, which limits the generalizability of the study. Third, the Korean EMS system adopted the ŌĆ£scoop and runŌĆØ model, in which the scene resuscitation time is usually short, which affects the results. Findings are likely different for other countries that allow resuscitation termination at the scene. For generalizability, further investigation across various environments is needed. Last, this study is a retrospective observational cohort study from which causality cannot be determined, and the data may contain significant potential uncontrolled biases. Additionally, unmeasured confounders could not be collected, such as team dynamics among EMS personnel.
For adult medical OHCA treated by a dual dispatch EMS response system, the number and level of first-contact EMS crew is associated with neurologic recovery and survival outcomes. These study findings may serve as a basis of policy development for EMS dispatch protocols and allocation of emergency resources.
SUPPLEMENTARY MATERIALSupplementary┬ĀTable┬Ā1.Interaction analysis by proportion of number of second-contact EMS crews across number of first-contact EMS crews and clinical outcomes Supplementary┬ĀFig┬Ā1.Yearly trend in first-contact emergency medical services (EMS) crew according to the study group. Supplementary materials are available at https://doi.org/10.15441/ceem.22.205.
ACKNOWLEDGMENTSThe authors thank the National Fire Agency of Korea and the Korea Centers for Disease Control and Prevention for their cooperation.
REFERENCES1. Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart Rhythm 2018; 15:e73-189.
2. Myat A, Song KJ, Rea T. Out-of-hospital cardiac arrest: current concepts. Lancet 2018; 391:970-9.
3. Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of- hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation 2010; 81:1479-87.
4. Grasner JT, Bossaert L. Epidemiology and management of cardiac arrest: what registries are revealing. Best Pract Res Clin Anaesthesiol 2013; 27:293-306.
5. Yan S, Gan Y, Jiang N, et al. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care 2020; 24:61.
6. Gold LS, Fahrenbruch CE, Rea TD, Eisenberg MS. The relationship between time to arrival of emergency medical services (EMS) and survival from out-of-hospital ventricular fibrillation cardiac arrest. Resuscitation 2010; 81:622-5.
7. De Maio VJ, Stiell IG, Wells GA, Spaite DW; Ontario Prehospital Advanced Life Support Study Group. Optimal defibrillation response intervals for maximum out- of-hospital cardiac arrest survival rates. Ann Emerg Med 2003; 42:242-50.
8. Meaney PA, Bobrow BJ, Mancini ME, et al. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation 2013; 128:417-35.
9. Kleinman ME, Brennan EE, Goldberger ZD, et al. Part 5: adult basic life support and cardiopulmonary resuscitation quality. 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015; 132(18 Suppl 2):S414-35.
10. Park JH, Shin SD, Ro YS, et al. Implementation of a bundle of Utstein cardiopulmonary resuscitation programs to improve survival outcomes after out-of-hospital cardiac arrest in a metropolis: a before and after study. Resuscitation 2018; 130:124-32.
11. Nordberg P, Hollenberg J, Rosenqvist M, et al. The implementation of a dual dispatch system in out-of-hospital cardiac arrest is associated with improved short and long term survival. Eur Heart J Acute Cardiovasc Care 2014; 3:293-303.
12. Raun L, Pederson J, Campos L, Ensor K, Persse D. Effectiveness of the dual dispatch to cardiac arrest policy in Houston, Texas. J Public Health Manag Pract 2019; 25:E13-21.
13. Hasselqvist-Ax I, Nordberg P, Herlitz J, et al. Dispatch of firefighters and police officers in out-of-hospital cardiac arrest: a nationwide prospective cohort trial using propensity score analysis. J Am Heart Assoc 2017; 6:e005873.
14. Saner H, Morger C, Eser P, von Planta M. Dual dispatch early defibrillation in out-of-hospital cardiac arrest in a mixed urban-rural population. Resuscitation 2013; 84:1197-202.
15. Hollenberg J, Riva G, Bohm K, et al. Dual dispatch early defibrillation in out-of-hospital cardiac arrest: the SALSA-pilot. Eur Heart J 2009; 30:1781-9.
16. Lee SY, Song KJ, Shin SD. Effect of implementation of cardiopulmonary resuscitation-targeted multi-tier response system on outcomes after out-of-hospital cardiac arrest: a beforeand-after population-based study. Prehosp Emerg Care 2020; 24:220-31.
17. Kim JH, Ryoo HW, Kim JY, et al. Application of a dual-dispatch system for out-of-hospital cardiac arrest patients: will more hands save more lives? J Korean Med Sci 2019; 34:e141.
18. Warren SA, Prince DK, Huszti E, et al. Volume versus outcome: more emergency medical services personnel on-scene and increased survival after out-of-hospital cardiac arrest. Resuscitation 2015; 94:40-8.
19. Sun JT, Chiang WC, Hsieh MJ, et al. The effect of the number and level of emergency medical technicians on patient outcomes following out of hospital cardiac arrest in Taipei. Resuscitation 2018; 122:48-53.
20. Kajino K, Kitamura T, Iwami T, et al. Impact of the number of on-scene emergency life-saving technicians and outcomes from out-of-hospital cardiac arrest in Osaka City. Resuscitation 2014; 85:59-64.
21. Tsai BM, Sun JT, Hsieh MJ, et al. Optimal paramedic numbers in resuscitation of patients with out-of-hospital cardiac arrest: a randomized controlled study in a simulation setting. PLoS One 2020; 15:e0235315.
22. Martin-Gill C, Guyette FX, Rittenberger JC. Effect of crew size on objective measures of resuscitation for out-of-hospital cardiac arrest. Prehosp Emerg Care 2010; 14:229-34.
23. Eschmann NM, Pirrallo RG, Aufderheide TP, Lerner EB. The association between emergency medical services staffing patterns and out-of-hospital cardiac arrest survival. Prehosp Emerg Care 2010; 14:71-7.
24. Hagiwara S, Oshima K, Aoki M, et al. Does the number of emergency medical technicians affect the neurological outcome of patients with out-of-hospital cardiac arrest? Am J Emerg Med 2017; 35:391-6.
25. Fang PH, Lin YY, Lu CH, Lee CC, Lin CH. Impacts of emergency medical technician configurations on outcomes of patients with out-of-hospital cardiac arrest. Int J Environ Res Public Health 2020; 17:1930.
26. Grunau B, Kawano T, Scheuermeyer F, et al. Early advanced life support attendance is associated with improved survival and neurologic outcomes after non-traumatic out-of-hospital cardiac arrest in a tiered prehospital response system. Resuscitation 2019; 135:137-44.
27. Park JH, Song KJ, Shin SD, Hong KJ. Does second EMS unit response time affect outcomes of OHCA in multi-tiered system? A nationwide observational study. Am J Emerg Med 2021; 42:161-7.
28. Lee S, Park JH, Ro YS, Hong KJ, Song KJ, Shin SD. Time to first defibrillation and survival outcomes of out-of-hospital cardiac arrest with refractory ventricular fibrillation. Am J Emerg Med 2021; 40:96-102.
29. Song KJ, Shin SD, Park CB, et al. Dispatcher-assisted bystander cardiopulmonary resuscitation in a metropolitan city: a before-after population-based study. Resuscitation 2014; 85:34-41.
30. Lee MJ, Rho TH, Kim H, et al. Part 3. Advanced cardiac life support: 2015 Korean guidelines for cardiopulmonary resuscitation. Clin Exp Emerg Med 2016; 3(Suppl):S17-26.
Fig.┬Ā1.Categorization of study groups according to the number and certification level of emergency medical services (EMS) crews in each ambulance in a dual dispatch. EMT-B, emergency medical technician basic level; EMT-I, emergency medical technician intermediate level; OHCA, out-of-hospital cardiac arrest. 
Fig.┬Ā3.Interaction plot by emergency medical technician intermediate level (EMT-I) proportion across number of first-contact emergency medical services (EMS) crews and clinical outcomes. (A) Good neurologic recovery, (B) survival to discharge, and (C) prehospital return of spontaneous circulation. 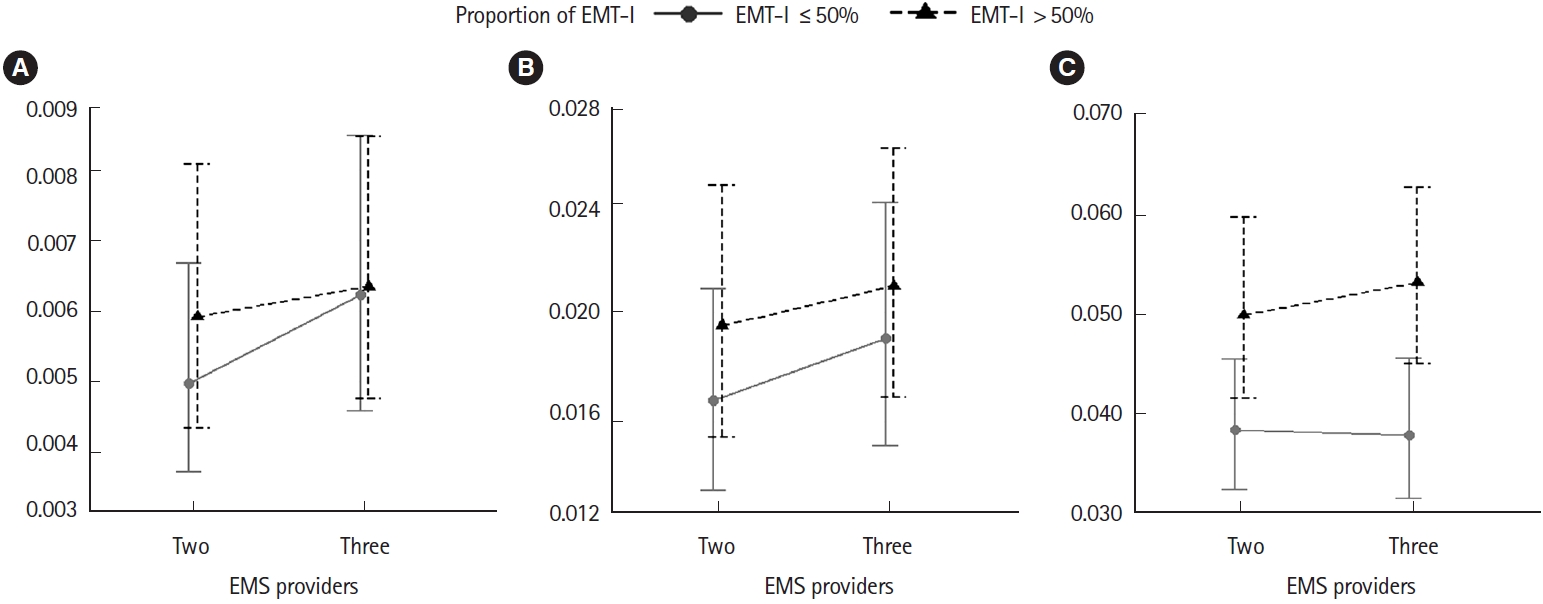
Table┬Ā1.Study population demographics according to number and level of first-contact EMS unit Values are presented as number (%) or median (interquartile range). EMS, emergency medical services; EMT-I, emergency medical technician intermediate level; ECG, electrocardiogram; CPR, cardiopulmonary resuscitation; RTI, response time interval; STI, scene time interval; TTI, transport time interval; ED, emergency department; ROSC, return of spontaneous circulation. Table┬Ā2.Multivariable logistic regression analysis by number or EMT-I proportion of first-contact EMS crews on clinical outcomes ORs were calculated after adjusting for age group, sex, public versus private location, metropolitan area, witness status, dispatcher recognition, bystander cardiopulmonary resuscitation, initial electrocardiogram rhythm, response time interval, time interval between EMS unit arrival, transport time interval, number and level of second-contact EMS crew, and level of emergency department. EMT-I, emergency medical technician intermediate level; EMS, emergency medical services; ROSC, return of spontaneous circulation; OR, odds ratio; CI, confidence interval. Table┬Ā3.Interaction analysis by EMT-I proportion across number of first-contact EMS crews and clinical outcomes
Odd ratios were calculated after adjusting for age group, sex, public versus private location, metropolitan area, witness status, dispatcher recognition, bystander cardiopulmonary resuscitation, initial electrocardiogram rhythm, response time interval, time interval between EMS unit arrival, transport time interval, number and level of second-contact EMS crew, and level of emergency department. EMT-I, emergency medical technician intermediate level; EMS, emergency medical services; ROSC, return of spontaneous circulation. |
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||