INTRODUCTION
There have been concerns about early neuroprognostication in cardiac arrest patients with highly malignant electroencephalogram (EEG) patterns because several patients have experienced good neurological outcomes despite a suppressed background or burst suppression 12 hours after hospital admission [1–3]. However, others have reported that highly malignant EEG patterns can predict neurologic outcomes at an early stage [4]. It is well known that EEGs are affected by sedative doses, but EEG suppression due to an appropriate use of sedatives in cardiac arrest patients is not sufficient to change the neurological outcomes [3,5]. To observe the change in the mean suppression rate (MSR) from the EEGs of patients with malignant and highly malignant EEG patterns, cardiac arrest patients in our hospital were monitored with frontal EEGs, which can automatically measure suppression (<10 µV) in an EEG background. We have found that two patients who did regain alertness were elderly, and frontal EEG monitoring showed a suppressed background and burst suppression. They were predicted to experience a poor neurological outcome. Similar episodes did not occur in our hospital in younger patients or even in most elderly patients when appropriate doses of sedatives were used; therefore, we report a severe increase in MSR caused by the appropriate augmentation of sedative doses. The patients provided informed consents for publication of the research details and clinical images.
CASE REPORTS
A case with suppressed background and a good neurological outcome
An 80-year-old male patient who had a history of unstable angina, hypertension, diabetes mellitus, and stage 3 chronic kidney disease was found on the street by a bystander. The bystander performed cardiopulmonary resuscitation (CPR) for 6 minutes after he immediately called the emergency services. When an ambulance arrived 6 minutes after the emergency phone call, an emergency medical technician performed CPR for 6 more minutes with two defibrillations. A return of spontaneous circulation (ROSC) was achieved. Upon arrival at the hospital, the patient was hypotensive with a blood pressure of 70/50 mmHg; pulmonary edema and cardiomegaly were visible on a chest X-ray. Initially, he exhibited stupor with a reactive pupillary reflex. Targeted temperature management (TTM) was induced with a surface-cooling device and sedation was initiated according to our TTM protocol; the starting dosages of propofol and remifentanil were 20 and 0.1 µg/kg/min, respectively, but the dosages were increased upon reevaluation as sedation was inappropriate due to the patient’s movement.
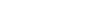
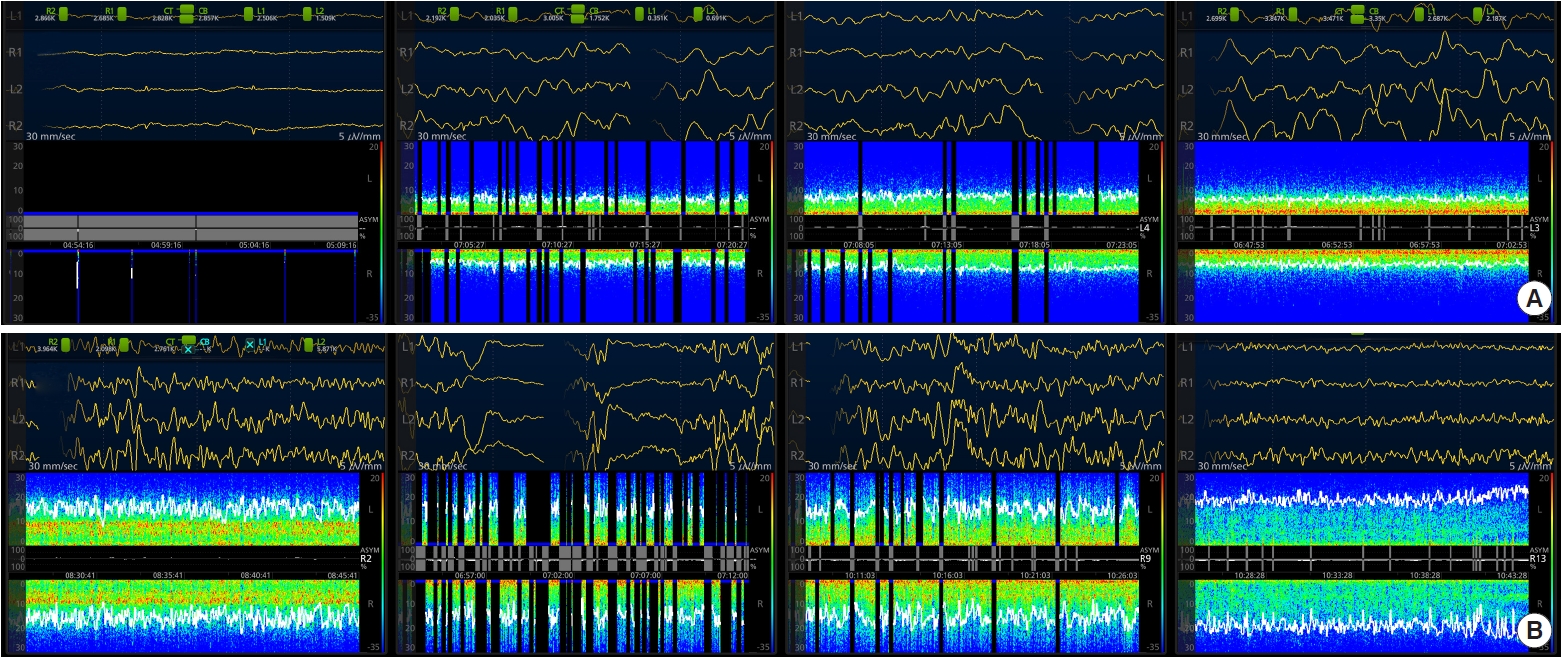
Sedatives were started; the dosage (propofol 50 µg/kg/min and remifentanil 0.2 µg/kg/min) was higher than an ordinary starting dosage, but it was still tolerable and has been reported in other studies [6,7]. The sedatives were maintained at the same dose for 58 hours and then afterwards tapered by reducing propofol by 10 µg/kg/min and remifentanil by 0.2 µg/kg/min every 4 hours. Frontal EEG monitoring was performed at the start of the TTM using a Sedline brain function monitor (Masimo Corporation, Irvine, CA, USA), which consists of four flexible electrodes placed on the forehead at Fp1, Fp2, F7, and F8. Initially, the background EEG showed a normal trace, but 2 and 4 hours after the start of sedation and TTM, the MSR rose to 85.5%–100%, and a poor neurological prognosis was predicted due to the suppressed background (Figs. 1A, 2). On day 2 (over 18 hours after the initiation of sedatives), the MSR had been reduced to 24.9% (discontinuous background) and 4.4% (Figs. 1A, 2). The MSR changed to 3.9%–13% on day 3 before tapering the sedatives, and no suppression was observed on day 4, when the sedatives were stopped 72 hours after beginning TTM.
On day 4, the mental status of the patient had improved from a semicomatose state to a deep stupor, and he began having spontaneous eye opening when asked to do so. During day 5, his consciousness gradually recovered becoming drowsy and responsive to commands. He was eventually diagnosed with cardiac arrest due to heart failure and pulmonary edema, and on day 21 after admission, he was alert and discharged in stable condition after receiving supportive care to treat the pulmonary edema, delirium, and wound infection during admission.
A case with burst suppression and a good neurological outcome
An 83-year-old female patient suddenly collapsed in front of her place of residence. A lay rescuer witnessed her fall and performed CPR for 5 minutes. Soon after, an emergency medical technician arrived at the scene and performed CPR with one defibrillation at 10 minutes. The patient’s initial heart rhythm showed pulseless electric activity, but she eventually achieved ROSC. Upon arrival at the hospital, she was stuporous, and her pupil size and reflexes were 2+/2+. Her initial blood pressure was 80/40 mmHg but improved shortly thereafter. TTM was induced with a surface-cooling device after admission, and she was given sedation according to our TTM protocol.
The starting dosage of propofol was 40 µg/kg/min, while that of remifentanil was 0.1 µg/kg/min. Frontal EEG monitoring was performed at the start of the TTM. Alpha and beta waves in her frontal lobe were largely observed on day 1, but MSR on day 2 was abruptly increased from 0% to 13.3%. A physician raised the dosages of the sedatives to 50 µg/kg/min of propofol and 0.2 µg/kg/min remifentanil because her patient state index was increased on day 2 and thereafter, and her EEG also showed a burst suppression, which was increased to 68.1% of MSR (38 hours after starting sedatives, 14 hours after raising the dose) (Figs. 1B, 2). Moreover, the patient developed a pinpoint pupil after increasing the remifentanil dosage from 0.1 to 0.2 µg/kg/min. The burst suppression was changed to a discontinuous background, and the MSR was gradually reduced to 15.7% (41 hours after starting sedatives and 18 hours after raising the dose), although the dose of the sedatives was not decreased (Figs. 1B, 2). As the doses of the sedatives were decreased over the rewarming period, her EEGs recovered with normal background activity and without any suppression on day 4. Sedatives were totally stopped at 72 hours after starting TTM.
On day 4, the patient was still in a coma, and nonreactive pinpoint pupils were noted. However, on day 5, she started waking and was responsive to commands. Small multiple lacunar infarctions were noted on her brain magnetic resonance imaging scan, but those lesions were not considered to be of much clinical significance. She was eventually diagnosed with a non-ST elevation myocardial infarction due to an unknown cause, and on day 10 after admission, she had stable vital signs and was transferred to another hospital in an alert to drowsy mental condition.
DISCUSSION
Physicians who treat cardiac arrest patients need to consider early neuroprognostication so they may counsel families and make management decisions to urge aggressive treatment or to avoid inappropriate treatment [8]. For accurate early neurological prognostication, it is essential to note that very elderly patients may present with a suppressed background or burst suppression, especially at the beginning of sedation, because the brains of elderly patients may be very sensitive to sedatives [9,10].
The causes that have led to considerably suppressed backgrounds during propofol-remifentanil anesthesia in surgical patients have been previously studied [11]. Age was the most important risk factor; patients >80 years old were noted to be at highest risk with an odds ratio of 10.59, while patients who were 60 to 80 years old had an odds ratio of 4.8. Our patients were 80 and 83 years old, respectively, and the increase in sensitivity to sedatives in their brain was most likely due to their advanced age. An immoderate impact on the brain after a mild opioid dose was identified in the female patient because she developed a pinpoint pupil that occurred after appropriately increasing the remifentanil dose. This pinpoint pupil arose in conjunction with burst suppression.
The brain’s susceptibility to sedatives in elderly patients has never been described in studies on the neuroprognostication of cardiac arrest patients. A suppressed background and burst suppression are considered to be highly malignant EEG patterns and have rarely been observed in patients who go on to experience a good neurological outcome. Nonetheless, a study that included 240 patients reported that all patients with an isoelectric EEG (<2 µV) died, but there were several patients with a good neurological outcome who had a suppressed background (11 patients) and burst suppression (four patients) at 12 hours after a cardiac arrest [1]. The authors surmised that a suppression pattern on EEG was still compatible with neurological recovery 12 hours after ROSC, but the reason for such a phenomenon was not revealed. The patients were a mean of 60.8 years of age, and the third interquartile value was 95 years. The vulnerability of their brains to sedatives due to their advanced age might have increased the suppression pattern in these patients. Another study could not exclude the possibility that the onset of suppressed background in the patients who survived might result from an interference between the EEG and propofol, but vulnerability due to a very old age was still disregarded [2].
The increased MSR that resulted from using routine sedative doses in elderly patients with good neurological outcomes may be persistent for 12 hours or more before gradually decreasing regardless of any tapering of the doses of sedatives; patients may still completely recover while the effects of sedatives on EEGs disappear by day 3 or 4. For early neuroprognostication upon EEG testing in patients who are quite elderly (approximately 80 years of age or older), sedatives should be started at a lower dose when possible. An early prediction of a poor neurological outcome based solely on the EEG without considering a patient’s advanced age and sedative dose might lead to false prediction. In very aged patients who are restored from cardiac arrest, physicians should recognize that even ordinary sedative doses can affect the brain’s cortical activities and create more suppressions.