Resuscitation duration inequality by patient characteristics in emergency department out-of-hospital cardiac arrest: an observational study
Article information
Abstract
Objective
Out-of-hospital cardiac arrest (OHCA) patients unresponsive to basic life support are frequently transferred to emergency departments (EDs) for further resuscitation. Although some survive with good neurologic outcomes, additional resuscitation in EDs is often futile. Without a dedicated termination of resuscitation (TOR) rule for ED resuscitation, the decision when to stop the resuscitation is up to emergency physicians. In this study, we assessed the association between patient characteristics and duration of resuscitation in EDs to understand how emergency physicians decide when to terminate cardiopulmonary resuscitation.
Methods
A retrospective analysis of the OHCA registry of a single ED was conducted. Adult (18 years or older) patients without any return of spontaneous circulation (ROSC) after unsuccessful ED advanced cardiac life support were included. The primary endpoint was duration of resuscitation attempts. Prehospital and demographic factors were assessed as independent variables. The relationship between these factors and duration of resuscitative attempts was analyzed with multivariable quantile regression.
Results
From January 2008 to August 2012, ED resuscitation was terminated without ROSC in 266 patients (53.5%). The duration of resuscitative attempts was significantly shorter if any of the currently recognized poor prognostic factors was present. Interestingly, controversial factors such as female sex and older age were significantly associated with shorter resuscitation duration, while factors definitively indicating poor prognosis, such as severe trauma and poor baseline neurological status, showed no significant association.
Conclusion
The results of this study suggest that physicians adjust the resuscitation duration according to their subjective prediction of futility despite the absence of evidence-based TOR guidelines.
INTRODUCTION
The prognosis of out-of-hospital cardiac arrest (OHCA) is grave, and prolonged resuscitation attempts for unresponsive OHCA patients are usually futile [1-4]. This has led to the development of the prehospital termination of resuscitation (TOR) rules [5-9]. However, OHCA patients not responding to prehospital resuscitation are often transferred to emergency departments (EDs) for further resuscitative attempts, and there is no TOR rule available for this situation. Therefore, the decision of when to terminate resuscitation attempts is largely determined by resuscitation team leaders [10,11]. However, such decisions are difficult to make and can be subject to significant personal biases [12-15], which might result in suboptimal care in certain patient groups. In this study, we assessed the validity of our hypothesis that there is significant inequality in the duration of resuscitation attempts and that such inequality is significantly associated with various patient characteristics.
METHODS
Study setting
The study facility was a 950-bed teaching hospital located in a city with a population of 480,000. The majority of the prehospital emergency care services in this area are provided by the Fire Service administered by the government [16]. The level of prehospital resuscitation care is primarily restricted to basic life support and, although some advanced cardiac life support (ACLS) interventions such as endotracheal intubation and rapid intravenous hydration are occasionally provided, ACLS is generally deferred until arrival in the ED in most cases. The management of cardiac arrest was based on the recommendations of the 2005 American Heart Association cardiopulmonary resuscitation (CPR) guidelines until the 2010 guidelines from the same organization were published and rapidly adopted. Field TOR rules are not usually considered except in unsalvageable cases in which clear indications of futility are present, such as massive traumatic injuries, putrefaction, or rigor mortis [16].
Study design and population
This was a retrospective analysis of a prospectively collected registry of OHCA patients extending from January 2008 to August 2012. Patients aged 18 years or older who received CPR on ED arrival were identified and included. The institutional review board at the study hospital approved the analysis and provided a waiver of consent.
ED cardiac arrest registry
The registry is managed by ED resuscitation researchers and includes all OHCA patients of the study facility [17,18]. It includes prehospital Utstein elements, ED resuscitation events, initial laboratory measurements, and patient outcomes. Utstein elements and ED resuscitation events are primarily collected by emergency medical technicians (EMTs) working in the study ED and reviewed by the researchers afterward. Patient outcomes are assessed by the review of electronic medical records and by telephone interview. The telephone interview is conducted by emergency medicine chief residents every month, and involves inquiries about the survival and functional status of the patient according to the published Cerebral Performance Category criteria [1].
Participants and data collection
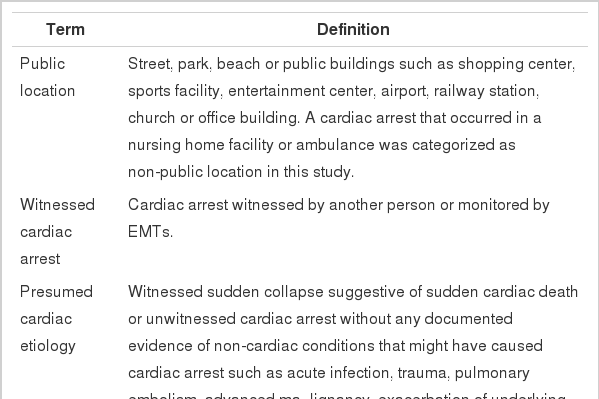
The primary endpoint of this study was the duration of resuscitation attempts when there is no return of spontaneous circulation (ROSC) during CPR. We defined ROSC as detection of any pulse regardless of its duration because we thought that even very brief ROSC could influence physicians’ decisions regarding the timing of TOR. Prehospital factors including arrest location, initial rhythm, cause of arrest, prehospital no/low flow time, and time of ED arrival, as well as patient factors such as sex, age, and presence of terminal illness, severe trauma, and poor baseline neurologic function were assessed as independent variables. The presence of terminal illness, severe trauma, and poor baseline neurologic function were determined from review of medical records. All of the other information regarding prehospital and patient factors was retrieved from the registry. The detailed definitions of the terms used in this study are provided in Table 1.
Statistical analysis
The median and interquartile range (IQR) of continuous variables were reported unless the variables followed a normal distribution, in which case the mean and standard deviation (SD) were reported. Analysis of variance, Kruskal-Wallis, chi-square, or Fisher exact test were performed for comparison between groups as appropriate. The association between resuscitation duration and independent variables was analyzed with multivariable quantile regression. The choice of the 25th and 75th percentiles in addition to the 50th percentile (median) was due to a non-obligatory tradition of routinely providing 30 minutes of CPR in the study facility. We presumed that the process of decision-making would be different according to whether CPR was terminated before or after the 30-minute margin. The results of quantile regressions are presented as regression coefficients (B) and their 95% confidence intervals (CIs). A P-value<0.05 was considered significant. All analyses were performed using STATA ver. 10.1 (Stata Corp LP., College Station, TX, USA).
RESULTS
Patient characteristics
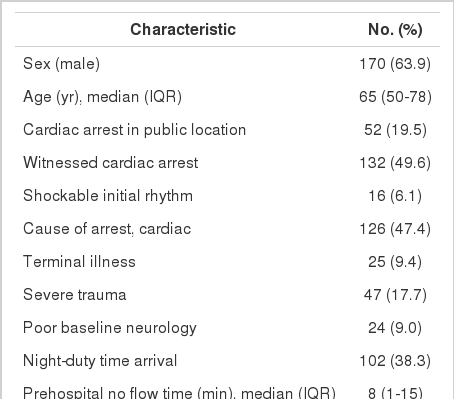
There were 594 adult (aged 18 or older) OHCA patients during the study period from January 2008 to August 2012, among which 572 were still in cardiac arrest upon ED arrival. After exclusion of patients with any ROSC event, a total of 266 were included for analysis. Prehospital and patient factors of the study population are described in Table 2. Of the patients, 170 (63.9%) were male, and the median patient age was 65 years (IQR, 50 to 78 years). Terminal illness, severe trauma, and poor baseline neurologic function were found in 25 patients (9.4%), 47 patients (17.7%), and 24 patients (9.0%), respectively. Further, 102 patients (38.3%)arrived at the ED during the night duty period. The duration of resuscitation attempts before termination had a median value of 29 minutes (IQR, 20 to 33 minutes) and its distribution showed a high peak around the median value with a kurtosis of 20.552 (P<0.001).
Association between resuscitation duration and patient characteristics
Patient characteristics were stratified into quartiles according to the duration of resuscitation attempts (Table 3). Median age, witnessed arrest, presumed cardiac etiology, and the presence of terminal illness were factors that differed significantly (P=0.015, 0.011, 0.002, and 0.003, respectively). To identify independent factors associated with the duration of resuscitation attempts, multivariable quantile regression analysis was performed (Table 4, Fig. 1). Age ≥65 years (B, -2.62; 95% CI, -4.47 to -0.76), public location (B, 2.17; 95% CI, 0.72 to 3.62), witnessed arrest (B, 6.07; 95% CI, 3.21 to 8.93), terminal illness (B, -9.43; 95% CI, -14.70 to -4.16), night duty arrival (B, 2.42; 95% CI, 0.85 to 4.00), prehospital no flow time (B, -0.18; 95% CI, -0.33 to -0.03), and prehospital low flow time (B, -0.11; 95% CI, -0.20 to -0.03) were independently associated with the median duration of resuscitation attempts. Multivariable quantile regression analysis at the 25th and 75th percentiles was also performed to identify independent factors associated with the resuscitation duration during the early (25th percentile) and late (75th percentile) resuscitation periods. During the earlier resuscitation period (25th percentile), male sex (B, 3.15; 95% CI, 0.85 to 5.46), age ≥65 years (B, -3.62; 95% CI, -6.16 to -1.07), public location (B, 3.62; 95% CI, 0.95 to 6.28), witnessed arrest (B, 6.23; 95% CI, 2.81 to 9.65), cardiac etiology (B, 4.15; 95% CI, 1.24 to 7.07), terminal illness (B, -9.69; 95% CI, -15.25 to -4.14), prehospital no flow time (B, -0.15; 95% CI, -0.30 to -0.01), and prehospital low flow time (B, -0.08; 95% CI, -0.20 to 0.05) were significant factors, while only age ≥ 65years (B, -3.79; 95% CI, -6.40 to -1.18), witnessed arrest (B, 3.12; 95% CI, 0.66 to 5.57), and night duty arrival (B, 2.23; 95% CI, 0.23 to 4.23) were significant during the later resuscitation period (75th percentile).
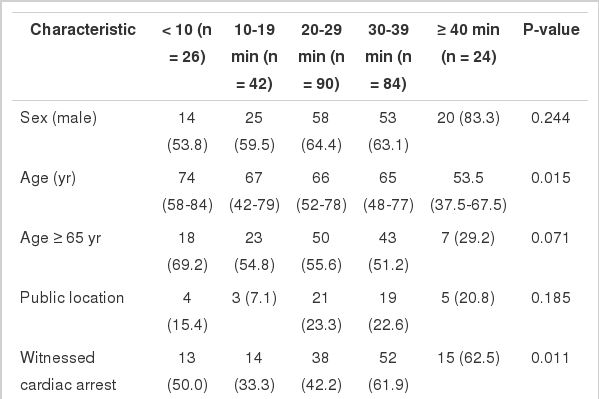
Characteristics of patients without return of spontaneous circulation stratified by resuscitation duration
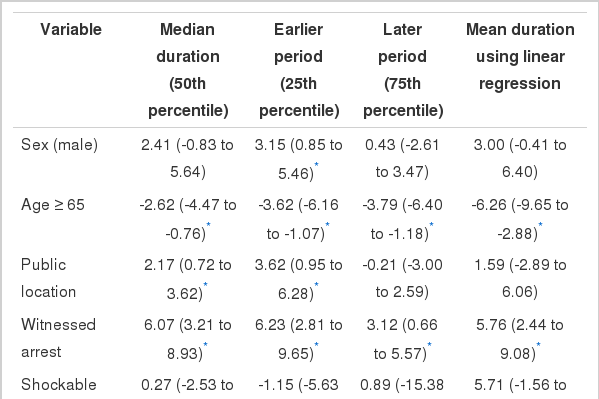
Multivariable quantile regression analyses of the association between resuscitation duration and patient characteristics
DISCUSSION
In this study, we found significant disparities in the duration of resuscitative attempts. As we had hypothesized, significant inequality was observed in the duration of resuscitation attempts, and such inequality was significantly associated with the presence or absence of various patient characteristics. In general, favorable prognostic findings were associated with longer resuscitation duration while unfavorable findings were associated with shorter duration. These results suggest that physicians are adjusting the resuscitation duration according to their estimation of prognosis despite the lack of published guidelines [10,11]. This finding is important, as it is possible that the duration of the resuscitation attempts can influence the overall outcomes. Goldberg et al. [19] reported significant interinstitutional variation in the duration of in-hospital resuscitation attempts. In their study, patients at hospitals with shorter resuscitation duration had a decreased likelihood of ROSC and survival to discharge. If resuscitation attempts for certain patient groups are terminated earlier, for whatever reason, the prognosis of those groups will be poorer. Furthermore, this association will perpetuate itself into a “self-fulfilling prophecy” if providers continue adjusting the resuscitation duration according to their estimation of prognosis.
Accurate prognostication is often difficult, and the clinical significance of known prognostic factors is difficult to quantify [14,15]. Therefore, the tendency toward early TOR in elderly patients and women observed in this study is noteworthy. There are many reports suggesting that old age itself is not significantly associated with poor outcome [20-23]. As for the sex difference, female sex has generally been associated with better outcomes [24-27]. The shorter resuscitation duration in women found in this study might provide an explanation for the findings reported by Akahane et al. [28] that neurologic outcomes in women of younger age were superior despite superior survival in men. These results could be due to the younger women undergoing relatively shorter resuscitative attempts, leading to selective survival of patients with lesser ischemic brain injury.
Interestingly, patient characteristics defining clear futility, such as traumatic cardiac arrest and poor baseline neurological function, did not show a significant association with the duration of resuscitative attempts in the current study. Traumatic cardiac arrest has been known to have very high mortality [29]. Thus, although there is plenty of room for improvement in trauma resuscitation, this patient characteristic should be considered as an indication for early termination if a shorter resuscitative attempt is to be justified by the expectation of poor outcome. On a similar note, resuscitation of a patient with poor baseline neurologic function should be assessed as futile because there is no way to improve that patient’s functional status following cardiac arrest. The exact reason why these factors were not associated with early termination in the present study remains unknown. Do emergency physicians overestimate the prognosis of traumatic cardiac arrest patients? Do they neglect obvious prognostic indicators such as baseline neurologic status? Further research on the capacity of emergency physicians for long-term prognostication might provide some clues to answer these questions.
This study has several limitations. First, the results of this study are based on a retrospective analysis of an ED OHCA registry and medical records, and are thus limited by possible biases that are intrinsic to such a design. Second, the results of this study do not provide additional clinical data that either support or oppose the appropriateness of the differences in the duration of resuscitation attempts. What the results do provide is evidence of the inequality in the duration of resuscitation attempts, which might play a role as a source of a “self-fulfilling prophecy.” Third, this is a single center study, and the results may not be generalizable to other facilities. There can be significant interinstitutional variation in resuscitation duration according to ED policy. For example, some institutions may put more effort into resuscitating futile cases in order to procure organs. Similarly, other institutions might adopt a policy of an equal duration of resuscitation attempts in every unresponsive patient for simplicity.
In summary, the results of this study suggest that physicians are adjusting the duration of resuscitation according to their subjective prediction of futility despite a lack of evidence-based guidelines. We suggest that this disparate care applied within the OHCA population should be considered (or controlled for) in future research, at least when newly discovered or biologically equivocal prognostic factors are studied.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This study was supported partially by Seoul National University Bundang Hospital (SNUBH) grant 02-2012-072.
References
Article information Continued
Notes
Capsule Summary
What is already known
It is unknown how emergency physicians decide when to terminate resuscitation attempts for out-of-hospital cardiac arrest patients in emergency departments (EDs).
What is new in the current study
The results of this study suggest that emergency physicians adjust the duration of resuscitation effort according to their subjective prediction of futility despite the absence of an ED-based termination of resuscitation guideline.