Pre-hospital i-gel blind intubation for trauma: a simulation study
Article information
Abstract
Objective
This study aimed to evaluate the efficacy of i-gel blind intubation (IGI) as a rescue device for definitive airway management in ground intubation for pre-hospital trauma patients.
Methods
A prospective randomized crossover study was conducted with 18 paramedics to examine intubation performance of two blind intubation techniques through a supraglottic airway devices (IGI and laryngeal mask airway Fastrach), compared with use of a Macintosh laryngoscope (MCL). Each intubation was conducted at two levels of patient positions (ground- and stretcher-level). Primary outcomes were the intubation time and the success rate for intubation.
Results
The intubation time (sec) of each intubation technique was not significantly different between the two positions. In both patient positions, the intubation time of IGI was shortest among the three intubation techniques (17.9±5.2 at the ground-level and 16.9±3.8 at the stretcher-level). In the analysis of cumulative success rate and intubation time, IGI was the fastest to reach 100% success among the three intubation techniques regardless of patient position (all P<0.017). The success of intubation was only affected by the intubation technique, and IGI achieved more success than MCL (odds ratio, 3.6; 95% confidence interval, 1.1 to 11.6; P=0.03).
Conclusion
The patient position did not affect intubation performance. Additionally, the intubation time with blind intubation through supraglottic airway devices, especially with IGI, was significantly shorter than that with MCL.
INTRODUCTION
Hypoxia and airway mismanagement contribute to up to 34% of pre-hospital deaths in trauma patients [1]. Several studies have shown that 7% to 28% of patients with trauma require definitive airway management, including endotracheal intubation (ETI) [2,3]. Moreover, paramedics mostly perform ground intubation in the pre-hospital setting for definitive airway management. However, during ground intubation using a Macintosh laryngoscope (MCL; GreenLite, Truphatek International, Netanya, Israel), it is not easy to expose the vocal cords, compared with a sternum-level bed setting [4]. Moreover, cervical immobilization of trauma patients makes it more difficult to visualize the vocal cords.
Video laryngoscopes (VL) have been tried to resolve hypoxia in pre-hospital trauma patients. The use of VL has advantages for securing a good view of the glottis in cervical-immobilized patients. Nevertheless, paramedics using VL encountered difficult circumstances in which the screen went black due to the camera of the VL being covered with blood or vomitus of patients [5].
Blind intubation using the laryngeal mask airway (LMA) Fastrach (LMF; Teleflex, Athlone, Ireland) has also been used in trauma patients for achieving ETI. It requires minimal head and neck movement while placing them into the patient’s oropharynx, and facilitates ETI as the patient is being simultaneously ventilated [6]. In previous studies using a sternum-level bed setting, LMF had a longer intubation time compared with MCL [7], but equivalent performance to i-gel blind intubation (IGI) regarding intubation time and success rate [8]. There has been no comparison study for IGI, LMF and MCL in the ground position.
Thus, we evaluated the efficacy of IGI as a rescue device for definitive airway management, compared with LMF and MCL in ground intubation for pre-hospital trauma patients. We hypothesized that IGI would have better intubation performance compared with LMF and MCL regarding intubation time and success rate.
METHODS
Study design
We conducted a randomized crossover manikin study to examine intubation performance using IGI, LMF and MCL at two different patient positions (ground- and stretcher-level). This study was performed at our hospital in June 2016. The local ethics committee approved this study and a waiver for participants was obtained in April 2016 (institutional review board no. 2016-03-27). We registered the study protocol in CRIS (Clinical Research Information Service, KCT0001942) in June 2016 before study initiation.
Equipment and material
At each patient position, participants attempted ETI using three types of intubation techniques: direct laryngoscopy using MCL and blind intubation with two different supraglottic airway devices (SADs). The MCL had a size-4 curved blade, and direct laryngoscopy was performed using with a Satin Slip Stylet (Mallinckrodt Medical, St. Louis, MO, USA). Two types of SADs were used for blind intubation in this study: a size-4 i-gel (Intersurgical, Berkshire, UK) and a size-4 LMF. A 7.0-mm internal diameter endotracheal tube (ETT) (Mallinckrodt Hi-Lo Oral/Nasal Tracheal Tube Cuffed Murphy Eye; Covidien, Dublin, Ireland) was used for direct laryngoscopy, and a 6.0-mm internal diameter ETT of the LMF was used for blind intubation through SADs. Each ETT was lubricated by airway lubricant (Airway lubricant glycerol version; Laerdal Medical, Stavanger, Norway) before performing ETI.
We used an airway trainer manikin (AirSim Advance Combo Bronchi; TruCorp, Belfast, Northern Ireland) to perform ETI. The simulation airway setting was regulated by cervical immobilization using a cervical collar (Perfit ACE; Ambu, Ballerup, Denmark). The stretcher-level patient position was simulated using a 91-cm-height of an ambulance stretcher (stretcher, 189×58×91 cm; Sungwoo Motors, Eumseong, South Korea).
Participants
The sample size was calculated based on a previous study regarding the time required for ETI [7]. The intubation times (mean±standard deviation) in that study were as follows: IGI (17.2±7.7 seconds) and LMF (26.3±13.6 seconds). To detect a 34% difference in intubation time with a power of 0.8, at least 16 operators were needed. We estimated that 20 operators would be adequate, considering an estimated 20% dropout rate.
We recruited healthy volunteer paramedics who were between 18 and 60 years of age and in charge of rescue departments. Any persons having cardiovascular, neurological, or musculoskeletal diseases affecting any part of the body and pregnant women were excluded.
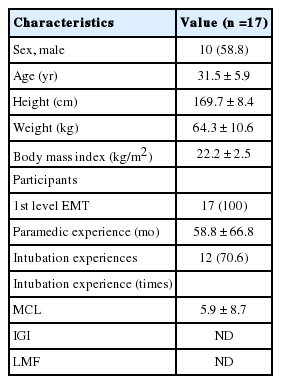
Interventions
All participants completed a brief questionnaire regarding demographic information (age, sex, body weight, and height) and prior clinical ETI experience with MCL, IGI, and LMF (Table 1). Before starting the experiments, instructors gave lectures, approximately 1 hour in duration, about ETI and SADs. Participants had a 10-minute ETI practice time to familiarize themselves with all devices.
Eighteen participants were finally enrolled, and they were randomly allocated into two groups: group A (n=9) and group B (n=9) (Fig. 1). After group allocation, the participants performed ETIs in a random order generated by a sequence generator (http://www.random.org) to minimize the learning effects for ETI. Only one ETI attempt was allowed for each device at phase 1 or 2. In phase 1, each participant of group A attempted ETIs using MCL or IGI or LMF according to the randomly given order at the groundlevel position. Similarly, the participants of group B (n=9) attempted ETIs at the stretcher-level position. After a mandatory rest period of 30 minutes, the participants of each group performed ETIs at the other level patient position in phase 2.
Outcomes
The primary outcomes were the intubation time and the success rate of ETI. The time required for SAD insertion (device insertion time, DT) was defined as the time from picking up SADs to complete insertion into the manikin. For MCL, DT was alternatively defined as the time from picking up the MCL to complete exposure of the larynx. The time required for ETT insertion (tube insertion time, TT) was defined as the time from picking up the SADs or MCL to successful insertion of the ETT. The time for first ventilation (FVT) was defined as the time from picking up SADs or MCL to successful first ventilation. Successful ETI was defined as a visible chest rise by bagging with bag valve mask. Intubation failure was defined as follows: esophageal ETI, incomplete progression of ETT in IGI or LMF, or exceeding the time limit of 120 seconds [9]. The glottis view was measured according to the Cormack and Lehane grade.
Statistical analysis
The data were compiled using a standard spreadsheet application (Excel; Microsoft, Redmond, WA, USA) and analyzed using the IBM SPSS Statistics ver. 20.0 (IBM Corp., Armonk, NY, USA). We generated descriptive statistics and presented them as frequencies and percentages for categorical data and mean±standard deviation for continuous data. To compare intubation times among the three intubation techniques, the Friedman test (nonparametric data) was used for continuous variables. A post-hoc analysis was conducted with the Wilcoxon signed rank test (nonparametric data) or a paired t-test (parametric data) using the Bonferroni correction. The McNemar test or Cochran’s Q test were used to compare categorical variables, such as the success rate for ETI and glottis view. Kaplan-Meier analysis was performed to analyze the cumulative success rate regarding intubation time. A post-hoc analysis was also performed using the logrank test with the Bonferroni correction. Additionally, multivariate logistic regression analysis was conducted to analyze the factors influencing successful ETI. For all analyzed data, P<0.05 was considered statistically significant. In contrast, in post-hoc analysis, P<0.017 was considered significant.
RESULTS
Baseline characteristics
Eighteen participants were enrolled in this study, and one participant was excluded. The baseline characteristics of the participants are shown in Table 1.
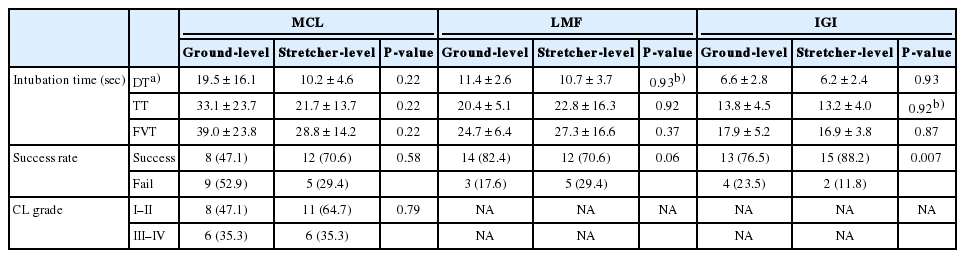
Intubation performance at two different positions
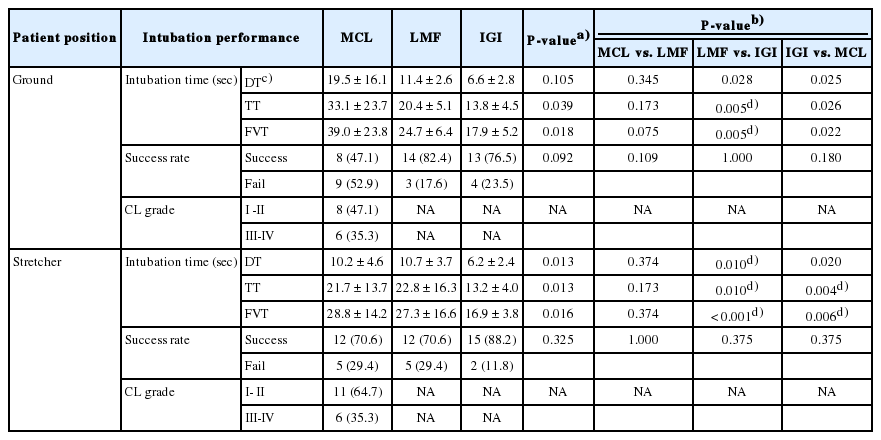
The intubation time was not significantly different between the two different positions regardless of the type of intubation technique (Table 2). The DT was not significantly different among the three intubation techniques in the ground-level position (P=0.10). At the stretcher-level position, the DT of IGI was significantly shorter than that of LMF (6.2±2.4 vs. 10.7±3.7, P=0.01)
The TT of IGI was significantly shorter than that of LMF in the ground-level position (13.8±4.5 vs. 20.4±5.1, P=0.005). At the stretcher-level position, the TT of IGI was the shortest among the three intubation techniques (P=0.005), although those of MCL and LMF were not significantly different.
For the comparison of FVT, the use of IGI reduced FVT compared with LMF in the ground-level position (17.9 ±5.2 vs. 24.7±6.4, P=0.005). At the stretcher-level position, the FVT of IGI was the shortest among the three intubation techniques, although those of MCL and LMF were not significantly different (LMF vs. IGI, P<0.001; IGI vs. MCL, P=0.006) (Table 3).
The success in the IGI was significantly related to patient position among three intubation techniques (P=0.007). The glottis view of MCL (Cormack and Lehane I–II) was not significantly related to patient position (P=0.79).
Cumulative success rate at two different positions
Regarding the cumulative success rates, IGI was the fastest among the three intubation techniques at both patient positions (all P<0.017). LMF was not significantly different from MCL at both patient positions (in ground-level, P=0.03; in stretcher-level, P=0.80) (Fig. 2).
Factors influencing successful intubation
The success of intubation was affected by the type of intubation technique. Although the success using LMF was equal to that of MCL, IGI achieved more success than MCL (odds ratio, 3.6; 95% confidence interval, 1.1 to 11.6; P=0.03). In contrast, the patient positions, the paramedic experience, and intubation experience were not independent factors affecting the success of intubation (Table 4).
DISCUSSION
To our knowledge, this is the first study for prehospital ground level intubation using IGI for trauma patients. In our study, IGI had a better performance compared with LMF and MCL, regardless of patient positions.
Head and neck trauma can cause airway obstruction via blood or vomitus of patients. In addition, ETI may become more difficult in cervical-immobilized patients. One previous study reported that blood or vomitus may impair visualization of the glottic inlet in out-of hospital patients when using MCL [5]. Although paramedics performed VL assisted ETI, they were unable to perform ETI in 7.5% of patients, primarily because of obstructed glottic views due to secretions and blood [10]. Therefore, we investigated the intubation performance of IGI and LMF as a rescue device in traumatic patients.
We compared intubation performances according to patient positions at stretcher- and ground-level. In the ground intubation using MCL, intubators have difficulty in laryngeal exposure. Hence, we considered stretcher-level positions similar to the sternum-level of intubators that makes an excellent view of the glottis possible [11]. We anticipated that MCL in the stretcher-level would show a better intubation performance compared with ground intubation. However, there were no differences of the intubation time and success rate of MCL between the two patient positions, as shown in Table 2. This result was similar to a previous study of paramedic ETI in different patient positions [12]. In obtaining a good glottic view using MCL, the ETI in the stretcherlevel was not significantly different from ground intubation.
DT of IGI was significantly shorter than that of LMF at the stretcher-level position, as shown Table 3. The shortened DT of IGI might be considerably affected by the i-gel as a non-inflationcuff device. When using IGI, intubators can save the time of inflating a cuff compared with other inflation-cuff devices, such as the LMF. Additionally, i-gel has the additional advantage of the thermoplastic elastomeric cuff design, which allows an optimal seal and reliable insertion of the i-gel. Hence, there might be some benefit for hypoxia in trauma patients from the shortened intubation time of IGI comparing with LMF. However, we thought that there was no significant difference of clinical efficacy as a rescue device for trauma patients between IGI and LMF since the success rates of both devices were similar.
Kim et al. [9] reported that the significant factors affecting intubation time were intubation experience and the type of laryngoscope, not the patient position, in the comparison of VL with MCL. Similarly, our study found that the type of intubation technique significantly affected intubation success, and IGI achieved more success than MCL (Table 4). As shown in Table 1, we measured intubation performance of less experienced paramedics. If experienced paramedics are enrolled in the next study, the measured intubation performance could differ from that of this study.
There were several limitations to this study. First, we used an airway trainer manikin, reflecting a regulated simulated airway using cervical immobilization in trauma patients. However, we did not simulate the distorted laryngeal anatomy in the manikin. Hence, the measured intubation performance could differ from that of traumatic patients who have a distorted larynx. Second, we did not simulate blood or vomitus in traumatic patients. If blood or vomitus occurs in ETI using MCL, it could shorten the required time for enduring hypoxia and interfere with the laryngeal exposure. Third, regardless of 30-minute washout period for crossover, a learning effect might still remain and it could affect the intubation performance of participants in phase 2.
In conclusion, the patient position did not affect intubation performance. Regardless of patient position, the intubation time of ETI through SADs, especially IGI, was significantly shorter than that of MCL.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This research was supported by Ministry of Public Safety and Security (MPSS-Fire Safety-2015-76).
References
Article information Continued
Notes
Capsule Summary
What is already known
Blind intubation using supraglottic airway devices such as the laryngeal mask airway Fastrach has also been used in pre-hospital trauma patients for achieving endotracheal intubation. There has been no study for the efficacy of i-gel blind intubation as a rescue device for definitive airway management.
What is new in the current study
Regardless of patient position, the intubation time of i-gel blind intubation was significantly shorter than that of laryngeal mask airway Fastrach and Macintosh laryngoscope. Therefore, i-gel blind intubation might be the appropriate option as a rescue device in pre-hospital traumatic patients