Usefulness of ultrasonography for the evaluation of catheter misplacement and complications after central venous catheterization
Article information
Abstract
Objective
To assess whether ultrasonographic examination compared to chest radiography (CXR) is effective for evaluating complications after central venous catheterization.
Methods
We performed a prospective observational study. Immediately after central venous catheter insertion, we asked the radiologic department to perform a portable CXR scan. A junior and senior medical resident each performed ultrasonographic evaluation of the position of the catheter tip and complications such as pneumothorax and pleural effusion (hemothorax). We estimated the time required for ultrasound (US) and CXR.
Results
Compared to CXR, US could equivalently identify the catheter tip in the internal jugular or subclavian veins (P=1.000). Compared with CXR, US examinations conducted by junior residents could equivalently evaluate pneumothorax (P=1.000), while US examinations conducted by senior residents could also equivalently evaluate pneumothorax (P=0.557) and pleural effusion (P=0.337). The required time for US was shorter than that for CXR (P<0.001).
Conclusion
Compared to CXR, US could equivalently and more quickly identify complications such as pneumothorax or pleural effusion.
INTRODUCTION
Central venous catheterization is required for the administration of medications such as vasopressors and chemotherapeutic agents, parenteral nutrition, hemodynamic monitoring, hemodialysis, or in case of a failure of peripheral venous access [1]. However, central venous catheter (CVC) insertion is associated with various complications. According to previous studies, the rates of complications are variable [2-4]. The complications of CVC insertion include arterial puncture, bleeding, misplacement, arrhythmia, air embolism, pneumothorax, hemothorax, cardiac tamponade, and infection [4-13]. Therefore, confirmation of complications is needed following the procedure. Chest radiography (CXR) has been used, but has several disadvantages, namely a limited ability to detect complications such as misplacement, cardiac tamponade, and hemothorax [14-16]. Furthermore, it is also often time-consuming and associated with risks related to radiation exposure. Recently, ultrasound (US) is increasingly used in emergency departments (EDs). US can be performed at the bedside and is associated with fewer risks than CXR. However, few studies have assessed catheter position and complications using US after CVC insertion [17-20]. The purpose of our study was to evaluate whether US performed in EDs could be used to evaluate catheter position and complications after CVC.
METHODS
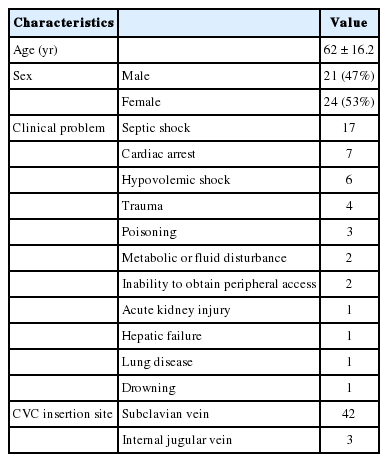
This was a prospective, observational study. Institutional review board approval (05-2014-009) was obtained, and all subjects provided written informed consent. The study was performed at the EDs of two university hospitals, with a combined annual census of approximately 68,000 adult visits. Patients aged ≥18 years undergoing central venous catheterization at the ED between January and June 2014 were included. The baseline characteristics of the study population are shown in Table 1.
Before the start of the study, a board-certified physician presented a 4-hour didactic lecture and scanning training to the residents. The residents then performed at least 20 studies under staff supervision. After the training, the residents had clinical experience with ultrasonographic studies of at least six months. A CVC was inserted via the subclavian or internal jugular vein. The rightside vessels were used in all but a few cases. Three-way Blue Flex-Tip ARROWgard Blue catheters (Arrow International, Bernville Road Reading, PA, USA) were used (7 French, 20 cm long). CVC insertion was performed without ultrasonographic guidance. Immediately after CVC insertion, we asked the radiologic department to perform a portable CXR scan. A junior and senior resident on shift each performed ultrasonographic evaluation of the position of the catheter tip and complications such as pneumothorax and pleural effusion (hemothorax). We assumed that the catheter tip was at the level of the superior vena cava when the catheter was not visualized in the right atrium or in the right internal jugular, left internal jugular, right subclavian, and left subclavian veins (excluding the catheterized vein). For example, when the right subclavian vein was used for catheterization, if the catheter was not visualized in the right atrium or right internal jugular, left internal jugular, or left subclavian veins, we determined that the catheter tip was at the superior vena cava. The right atrium was scanned using apical four-chamber or subcostal views. Internal jugular veins were scanned at the triangle formed by the two heads of the sternocleidomastoideus muscle and the clavicle. The subclavian veins were scanned below the middle of the clavicle. The vessels were scanned longitudinally and cross-sectionally. If we could not determine if the vessel was a vein, we distinguished the vein from arteries by compression of the vessel or the Valsalva maneuver. Pneumothorax was assessed at the level of the third and fourth intercostal spaces of both midclavicular lines. Pneumothorax was diagnosed as the absence of normal lung sliding, lung point present in the B-mode, and stratosphere sign present in the M-mode. Pleural effusion (hemothorax) was assessed at the level of the 8–11th intercostal spaces of both posterior axillary lines. We regarded hypoechoic lesions between the parietal pleura and the visceral pleura as pleural effusion. We also estimated the time required for US and CXR. The time interval between turning the US machine on and off was defined as the time required for US. The time interval between requesting the scan and registration of the image to the picture archiving and communication system (PACS) was defined as the time required for CXR. CXR was performed using a Mobilett Hybrid XP (Siemens Medical System, Erlangen, Germany). All radiological images were uploaded to a PACS. The PACS used was Marosis ver. 5.4 (Infinite, Seoul, Korea). US was performed using a z.one ultra US system (Zonare Medical System, Bernardo Anenue, CA, USA).
All statistical analyses were performed using SPSS ver. 11.0 (SPSS Inc., Chicago, IL, USA). Fisher’s exact tests were used to compare the concordance between US and CXR for evaluation of catheter tip position, pneumothorax, and pleural effusion. The interobserver agreement of US was evaluated by Cohen K tests. Kruskal-Wallis tests were used to compare the scanning times between US and CXR. P-value <0.05 were considered statistically significant.
RESULTS
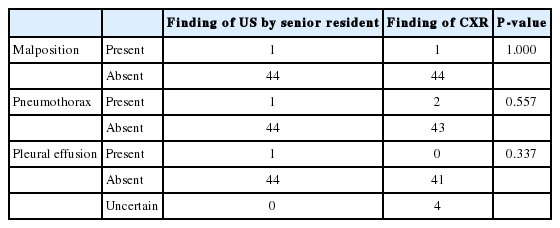
A total of 45 patients were included in the study (Fig. 1). In many cases, US failed to verify the presence of the catheter tip in the atrium. This occurred in 19 US examinations conducted by junior residents, and 16 examinations conducted by senior residents. Compared to CXR, US conducted by junior residents could equivalently identify the catheter tip in the internal jugular vein (P=1.000). Only one case of a misplaced catheter was observed. In this case, the CVC was inserted through the subclavian vein, with the catheter tip in the internal jugular vein. Compared to CXR, US conducted by senior residents also equivalently identified the catheter tip in the internal jugular vein (P=1.000) (Tables 2, 3).
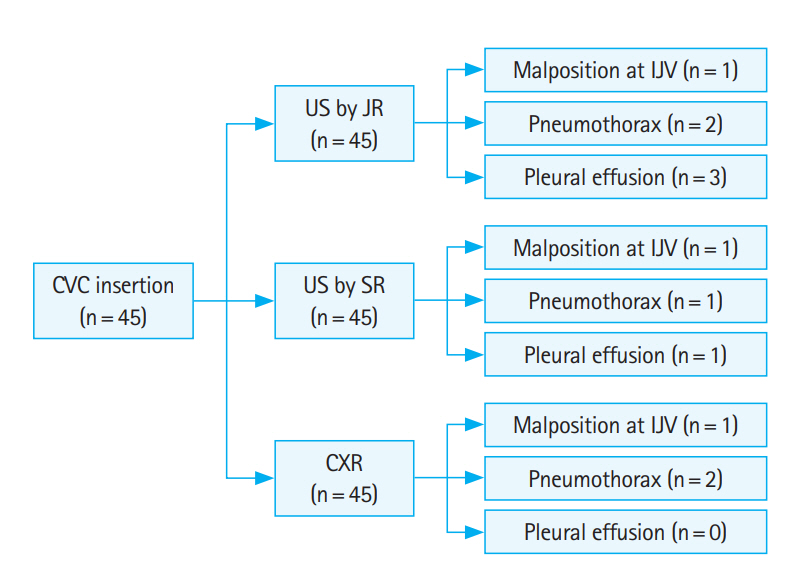
Study enrollment. CVC, central venous catheter; US, ultrasound; JR, junior resident; IJV, internal jugular vein; SR, senior resident; CXR, chest radiography.
Compared with CXR, US examinations conducted by junior residents equivalently evaluated pneumothorax (P=1.000), while US examinations conducted by senior residents could equivalently evaluate pneumothorax (P=0.557) and pleural effusion (P=0.337) (Tables 2, 3). When we compared US and CXR with respect to the evaluation of pleural effusion, we excluded those cases with uncertain CXR results. The inter-rater agreement between junior and senior residents for US evaluation of pneumothorax was unsatisfactory (kappa=0.656, P<0.001). This was the same in the case of pleural effusion (kappa=0.483, P<0.001).
The median time required for CXR was 10 minutes (interquartile range [IQR], 7 to 13 minutes). The median times required for US conducted by junior and senior residents were 5 minutes (IQR, 4 to 6 minutes) and 3 minutes (IQR, 3 to 5 minutes), respectively. The time required for US was shorter than that for CXR (P<0.001) (Fig. 2). Post-hoc analysis revealed that the required times for US did not differ between the junior and senior residents.
DISCUSSION
The use of US has been increasing in clinical practice. Traditionally, US has been considered for the evaluation of the heart, but many reports suggest that US is more useful for assessing the lungs and pleura than CXR [21-23]. In particular, US has become popular in EDs because it is less time-consuming, easy to perform, and safe. Moreover, large blood vessels such as the internal jugular and subclavian veins, and pleural pathologies such as pneumothorax and hemothorax, can be easily evaluated by US. Our study also showed that US and CXR have not different in evaluating these vessels and complications. There was a slight difference in the identification of pleural effusion between CXR and US by junior residents, but this was not statistically significant. These cases involved misdiagnosed pleural effusions from US examinations performed by junior residents, but the effusions were not visible on CXR. Abdominal computed tomography (CT) revealed abdominal ascites instead of pleural effusion. The diaphragms were elevated above normal levels due to abdominal ascites, so the junior residents misdiagnosed the ascites as pleural effusions during US. Therefore, we believe that abdominal scans should be performed to confirm the presence of abdominal ascites if pleural effusion is observed by US. The inter-rater agreement between junior and senior residents for US evaluation of pneumothorax and pleural effusion was relatively unsatisfactory. This was due to the patients with ascites who were misdiagnosed as having pleural effusion as well as the small sample size.
The evaluation of misplacement and complications after CVC insertion by CXR can sometimes take a long time; in this study, it took up to 30 minutes. The time required for US was shorter than that required for CXR. The complications due to CVC insertion can be a matter of great urgency and sometimes lead to mortality [8,11]. Mechanical complications occur in 7.1% to 33.2% of all cases [2-4,6]. Most of the cases were failed attempts and arterial puncture. Few cases of pneumothorax and hemothorax complications were reported. In our study, we found similar risks to those reported by other studies. However, there may be a bias in favor of the small number of experienced operators who performed central venous catheterization. US can help in the management of CVC insertion-related complications by detecting them faster than with CXR. In addition, CXR cannot conclusively identify pericardial effusion. In addition, when the patient is lying face-up, the condition most patients in critical condition tend to assume, CXR cannot identify pleural effusion.
While few studies have compared the accuracy of US with that of CXR [17-20], to our knowledge, no study has compared the accuracy of US with that of CT. While chest CT could detect complications such as pneumothorax or pleural effusion that were not seen on CXR or US, this difference was not significant enough to affect hemodynamic prognoses. Chest CT can be useful to assess pericardial effusion or CVC position after insertion. Thus, further studies that include a larger number of patients who undergo CT may help to substantiate the use of US in assessing catheter position or pericardial effusion.
Although the assessment of catheter tip position in the internal jugular or subclavian veins could be easily performed using US, deciding whether the catheter tip was at the level of the superior vena cava or the atrium was difficult because we could not identify the atrial cavity accurately using US. Characteristic of many critical patients, many patients refused to undergo US. When a four-chamber view was not well defined, we could not determine whether the catheter had entered the heart. Therefore, we believe that operator experience and patient cooperation are important for the evaluation of the position of catheters in the atrium.
The limitations of this study include the small number of study centers and patients. In addition, although we trained the US operators before proceeding with the study, their skills were not completely standardized and the atrium could not be scanned correctly in many US examinations. Catheter tip malposition was limited to the atrium or internal jugular vein, but the inferior vena cava, mammary vein, and pericardiophrenic vein were not considered, which when catheterized can also lead to lethal complications.
In conclusion, compared to CXR, US equivalently and more quickly identified complications such as pneumothorax and pleural effusion.
Notes
No potential conflict of interest relevant to this article was reported.
References
Article information Continued
Notes
Capsule Summary
What is already known
Ultrasound is more useful than chest radiography for assessing the lungs and pleura. Moreover, large blood vessels such as the internal jugular and subclavian veins, and pleural pathologies such as hemopneumothorax can be easily evaluated by ultrasound.
What is new in the current study
Ultrasound and chest radiography offer similar efficacy in evaluating large blood vessels and complications from their cannulation. Ultrasound can help in the management of central venous catheter insertion-related complications by detecting them more quickly than with chest radiography.