Potential impact of cardiology phone-consultation for patients risk-stratified by the HEART pathway
Article information
Abstract
Objective
Bedside consultation by cardiologists may facilitate safe discharge of selected patients from the emergency department (ED) even when admission is recommended by the History, Electrocardiogram, Age, Risk factors, Troponin (HEART) pathway. If bedside evaluation is unavailable, phone consultation between emergency physicians and cardiologists would be most impactful if the resultant disposition is discordant with the HEART pathway. We therefore evaluate discordance between actual disposition and that suggested by the HEART pathway in patients presenting to the ED with chest pain for whom cardiology consultation occurred exclusively by phone and to assess the impact of phone-consultation on disposition.
Methods
We performed a single-center, retrospective study of adults presenting to the ED with chest pain whose emergency physician had a phone consultation with a cardiologist. Actual disposition was abstracted from the medical record. HEART pathway category (low-risk, discharge; high-risk, admit) was derived from ED documentation. For discharged patients, major adverse cardiac events were assessed at 30 days by chart review and phone follow-up.
Results
For the 170 patients that had cardiologist phone consultation, discordance between actual disposition and the HEART pathway was 17%. The HEART pathway recommended admission for nearly 80% of discharged patients. Following cardiologist phone-consultation, 10% of high-risk patients were discharged, with the majority having undergone a functional study recommended by the cardiologist. At 30 days, discharged patients had experienced no episodes of major adverse cardiac events or rehospitalization for cardiac reasons.
Conclusion
For patients presenting to the ED with chest pain, cardiology phone-consultation has the potential to safely impact disposition, primarily by facilitating functional testing in high-risk individuals.
INTRODUCTION
Chest pain is a highly prevalent reason for visiting the emergency department (ED) [1] and efficient risk-stratification of this patient population remains challenging. Prior work has examined the impact of a triage program in which cardiologists provide consultation to the ED to assist with patient flow and disposition decisions. These studies have demonstrated that contemporaneous bedside evaluation by a cardiologist often yields a lower History, Electrocardiogram, Age, Risk factors, Troponin (HEART) score [2] than the initial assessment by an emergency physician [3], which may contribute to the reported 15% to 20% discharge rate among patients consulted on by a triage cardiologist [4].
While formal in-person evaluation by a triage cardiologist remains preferable, this intensive and relatively time-consuming level of service may not be feasible in all cases due to high-volume or cardiologist availability. An in-depth phone conversation between emergency and triage cardiology physicians may be a mechanism by which increasing demand can be accommodated without impacting quality of care. In a previously described cohort [3], most triage cardiology consultations for patients presenting with chest pain were addressed via phone discussion, without in-person consultation. Coupled with the HEART pathway information collected as part of that work, this experience affords an opportunity to analyze the potential impact of phone-based triage cardiology consultation on disposition decisions.
The role of phone-triage may be most impactful in situations where the ultimate disposition, arrived at after discussion between emergency physician and triage cardiologist, is discordant from that suggested by the HEART pathway. An example of such discordance is pursuit of ED-based functional testing or direct discharge in patients for whom the HEART pathway algorithm would have suggested admission. If actual disposition is entirely congruent with that recommended by the HEART pathway, then phone consultation for patients presenting to the ED with chest pain may be superfluous.
By comparing actual disposition, influenced by phone discussions with a triage cardiologist, to that suggested by the HEART pathway, we aim to (1) quantify any discordance between phone triage-based and HEART pathway-recommended disposition; (2) evaluate determinants of discrepancy between actual and HEART pathway-recommended disposition; and (3) assess the potential impact of cardiology phone-consultation on disposition.
METHODS
Study design and setting
We performed a single-center, cross-sectional, retrospective study of adults presenting to the ED with chest pain whose emergency physician, for the purpose of obtaining assistance with management or disposition, engaged in a telephone discussion with a triage cardiologist. This study was approved by the institutional review board of Vanderbilt Medical Center (151085, 161632). Written informed consent was waived due to the retrospective nature of the study.
The details of the triage cardiology program have been described previously [3,4]. Briefly, 7 general cardiologists (referred to as triage cardiologists) provide consultation to the ED between 8 a.m. and 5 p.m. on nonholiday weekdays. Calls are placed by the emergency physician to a cardiology access center staffed by dedicated cardiac nurses. After documenting the time at which the request for consultation is made, a nurse routes the call to the triage cardiologist and documents the encounter. As depicted in the flow diagram (Fig. 1), this study focused on the subset of patients presenting with chest pain for whom a telephone consultation between an emergency physician and a triage cardiologist occurred.
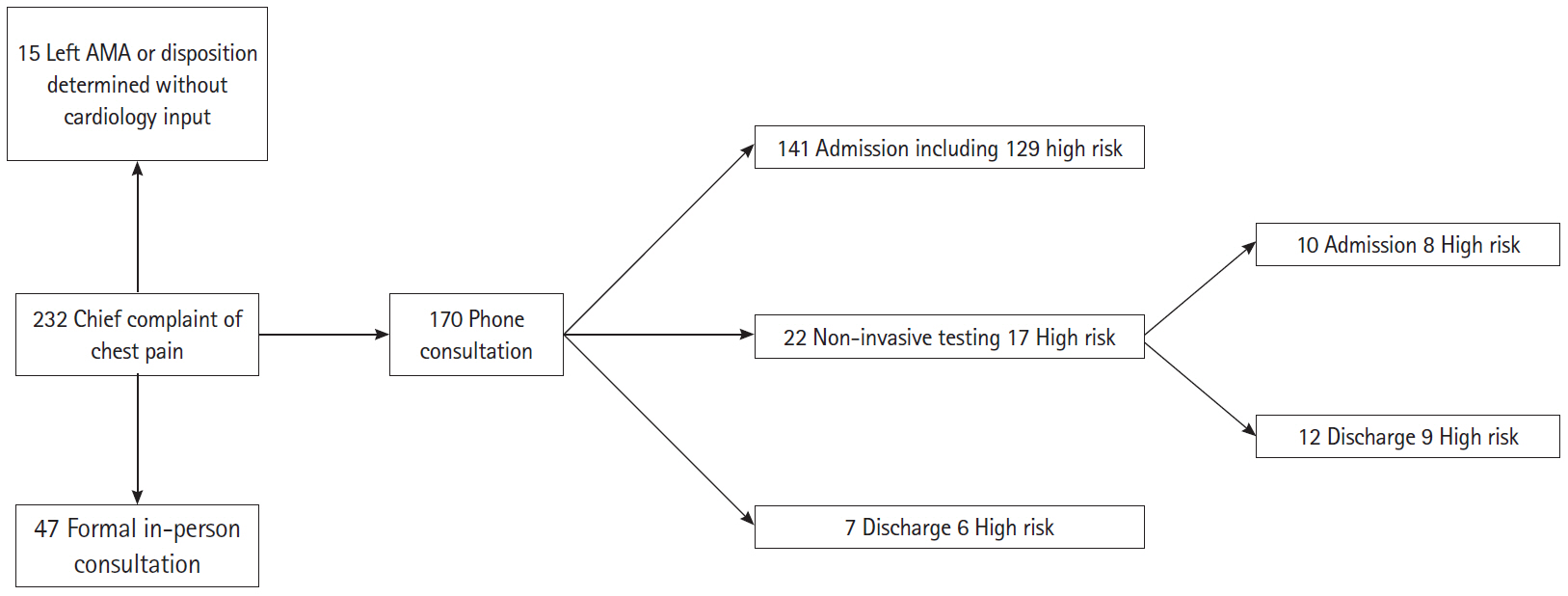
Study flow diagram. Of the 232 patients with a chief complaint of chest pain consulted on by the triage cardiology service during the study period, 170 were exclusively discussed by phone. Further information regarding History, Electrocardiogram, Age, Risk factors, Troponin (HEART) pathway risk category, the use of non-invasive cardiac testing in the emergency department, and disposition is also provided. AMA, against medical advice.
Study population
We conducted a retrospective chart review of patients ≥18 years of age who presented to our institution’s adult ED between January 1, 2015 and June 30, 2015 with a chief complaint of chest pain and for whom (1) the emergency physician’s concern for acute coronary syndrome prompted contact with the triage cardiology access center, (2) a telephone discussion between the emergency physician and triage cardiologist took place prior to a decision regarding disposition, and (3) the phone encounter was documented in the patient’s electronic medical record (EMR) by an access center nurse. Patients who had a formal bedside evaluation by the triage cardiologist during their ED stay were excluded.
Data collection
As previously reported [3], elements of the HEART score and HEART pathway were retrospectively collected and calculated [2]. Briefly, the HEART score is calculated from 5 components (history, electrocardiogram, age, risk factors, and troponin) each assigned 0 to 2 points based on previously published criteria; thus, the overall HEART score has a range of 0 to 10 points [2]. The HEART pathway incorporates a repeat troponin level (done approximately 3 hours after the initial troponin) and yields an assessment of risk; those with serially negative troponins and 0 to 3 points are typically low-risk and those with more than 3 points are categorized as high-risk. This pathway has been shown in a randomized trial [2] to identify those individuals that can be safely discharged from the ED and the worksheet for calculation of the HEART score and risk-assessment via the HEART pathway is located in an appendix to that trial. The use of retrospectively calculated HEART scores is not limited to our group’s prior work. Recently, a large study (n>100,000) that compared chest pain risk-stratification algorithms incorporated HEART scores derived retrospectively from clinical notes into the analysis [5]. Data elements that were recorded as ‘missing’ and those recorded as ‘not present’ were treated similarly. Our institution’s standard assay (contemporary troponin I) was used for the initial and 3-hour follow-up troponin levels.
Patients were classified as having cardiovascular disease if a history of any of the following was documented in their chart: coronary artery disease, myocardial infarction, dysrhythmia, systolic/diastolic heart failure, valvular surgery, or congenital heart disease [3,4].
The type and categorical outcome (i.e., ‘normal’ or ‘abnormal’) of any non-invasive cardiovascular testing ordered through the ED prior to a disposition decision were collected via review of the EMR. These tests included surface echocardiography, stress echocardiography, nuclear perfusion imaging, or dedicated coronary computed tomography angiography. For most patients, the results of cardiovascular testing were documented in emergency physician notes and described as having contributed to disposition decision-making. In cases where the test results were not explicitly mentioned, the test report was examined. Communication of the results to the emergency physician by the interpreting cardiologist or radiologist was documented uniformly, including the time of the discussion with the emergency physician. In all occurrences, the time of result notification preceded the relevant disposition order for admission or discharge from the ED.
Each patient’s primary attending emergency physician (i.e., the physician responsible for formulating or executing the disposition plan) was recorded. The completion date of each faculty member’s residency training was obtained using the department of emergency medicine’s personnel records.
For all discharged patients, 30-day outcomes were assessed by chart review (initial review by several co-authors and independently confirmed by the corresponding author). Patients were considered alive at 30-days if there was clear evidence in the EMR of clinical interaction at or beyond that timeframe (i.e., clinic visit, laboratory results, etc.) or if vital status was confirmed via phone call. Re-evaluation at our ED and re-hospitalization at our institution were also recorded by review of the EMR. ED visits or hospitalizations at other facilities were recorded if these events were clearly documented by review of outside records that were uploaded into our EMR as part of routine care or reference to them was made in subsequent notes. Major adverse cardiac events, defined as cardiac death, non-fatal myocardial infarction, or need for urgent coronary revascularization, were abstracted from the EMR. In addition, follow-up phone calls were placed approximately 18 to 24 months after the index ED visit to all discharged patients using a standardized script (several co-authors). When available, information regarding the above 30-day outcomes was obtained from discussions with patients, their spouses, or first-degree relatives. These outcomes were unknown at the time of initial data abstraction.
Data Analysis
For demographics and clinical characteristics, continuous variables were reported as mean±standard deviation and categorical variables as frequency and percentage. Attending physician experience was determined by calculating elapsed time (in years) between the completion of residency training and the day of the patient encounter. The timing of phone consultation was expressed as a percentage of the triage shift that had been completed when the request for consultation was made. This metric was calculated by determining the interval between the time of the request and the start of the shift (8 a.m.), dividing by the duration of the shift (9 hours), and multiplying the quotient by 100.
We analyzed discordance in disposition as recommended by the HEART pathway and actual disposition following phone-consultation with a triage cardiologist. Low-risk patients that were admitted and high-risk patients that were discharged were considered discordant. As in our prior work, the dataset used in this study was acquired prior to the introduction of the HEART pathway into routine practice at our institution. As a result, the HEART scores and HEART pathway recommendations were derived via retrospective application of those tools and, therefore, decisions regarding disposition were unbiased relative to the HEART score/pathway. Thus, for the purposes of this study, we presumed that (1) the impact on risk-stratification of any discrepancies between retrospectively and prospectively calculated HEART scores in this cohort would be small [3]; and (2) the HEART pathway recommendation would have been a key determinant of disposition [2]. Patients were stratified by actual disposition (admit or discharge) and risk category/recommended disposition as determined by the HEART score/pathway (≤3, low-risk/discharge; >3, high-risk/admission) [2]. Comparisons of HEART scores, HEART score components, ED physician experience, and consult timing were made between these groups.
Comparisons between continuous variables were made using the two-tailed Student t test (if normally distributed) or the Mann-Whitney test (if non-normally distributed). Comparisons between categorical variables were made using the chi-square test or Fisher exact test. Given the relatively small number of discharges and the paucity of 30-day events, multivariate analysis of adverse outcomes was not performed. All analyses were completed in GraphPad Prism ver. 7.02 (GraphPad, La Jolla, CA, USA); P<0.05 was considered statistically significant.
RESULTS
During the 6-month study period, phone consultations with a triage cardiologist were conducted for 170 unique patients presenting to the ED with chest pain (Fig. 1). The vast majority (approximately 90%) were admitted to a cardiology service. A similar proportion (152/170, 89%) were characterized as high-risk by application of the HEART score/pathway. Less than 13% (22/170) of patients underwent non-invasive cardiac testing prior to the decision regarding disposition. Review of the access center notes and the ED physician notes with attention to the intent of the call to the access center by the ED physician reveals that of the 19 patients that were discharged, the goal of the ED call to the access center was to request admission for 15 of those patients and to discuss candidacy for functional testing for the remaining 4 patients.
Cohort characteristics, stratified by HEART pathway risk, are shown in Table 1. As expected, high-risk patients were significantly older than the low-risk group and had a higher prevalence of cardiovascular disease and diabetes mellitus. There was no difference in the gender distribution between the groups. No patient in this cohort had a positive troponin value, either initially or on 3-hour follow-up re-check.
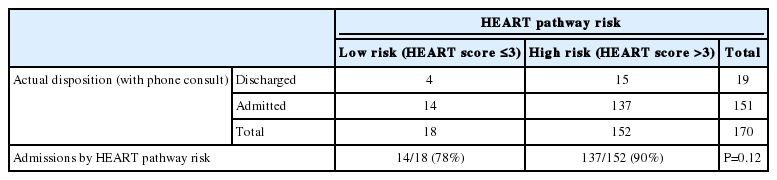
Table 2 displays the primary discordance data and stratifies actual/phone triage-based disposition by HEART pathway risk category. The majority of discharged patients were considered high-risk according to the HEART pathway (15/19, approximately 80%). The overall discordance rate for this cohort was 17% (29/170) with nearly 10% of high-risk patients having been discharged. There was no difference in actual disposition based on HEART pathway risk as 78% of low-risk patients were admitted and 90% of high-risk patients were admitted (P=0.12, Fisher exact test).
The distribution of HEART scores as a function of actual disposition is shown in Fig. 2A. For both the whole cohort and the (substantial) sub-group of admitted patients, the full range of HEART scores is represented and is essentially normally distributed. Fig. 2B stratifies the cohort by HEART pathway risk in addition to actual disposition and demonstrates that two-thirds of the high-risk discharge group had a HEART score at least a full point higher than the minimum needed to qualify for the high-risk designation.

Distribution of History, Electrocardiogram, Age, Risk factors, Troponin (HEART) scores by disposition and HEART pathway risk category. (A) HEART scores for the entire cohort and admitted patients are essentially normally distributed and encompass the entire range. Discharged patients have higher HEART scores than expected with approximately 80% exceeding the HEART pathway threshold for admission. (B) HEART scores stratified by disposition and HEART pathway risk. Two-thirds of the high-risk discharge cohort had a HEART score at least a full point higher than the HEART pathway threshold for admission.
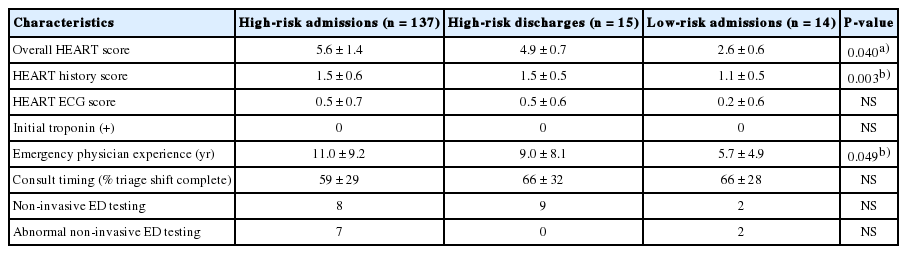
Overall HEART scores and additional factors that may have influenced disposition are compared in Table 3. The high-risk discharges have a significantly lower total HEART score than high-risk admissions (4.9±0.7 vs. 5.6±1.4, P<0.05). However, the mean HEART score between these groups differs by less than a full point and the median HEART scores are the same (5 for both groups).
There were no differences in HEART history score, HEART electrocardiogram score, emergency physician experience, or consult timing between the high-risk admission and high-risk discharge groups. All non-invasive testing was negative for the discharged group, although 40% (6/15) of these individuals were discharged without additional cardiac testing, despite being classified as high-risk. Of note, the low-risk admission group had lower HEART history scores than the high-risk admission group and statistically similar HEART ECG scores. The interval between completion of residency training and the patient encounter was almost 50% shorter for emergency physicians involved in the care of the low-risk admission group compared to those caring for the high-risk admission group.
For the low-risk admission group (n=14), 2 patients had cardiac testing through the ED, the results of which prompted admission. One patient had an abnormal nuclear perfusion study, then was found to have multi-vessel coronary disease on angiography, and ultimately underwent coronary artery bypass graft surgery. Another patient had an abnormal coronary computed tomography angiography and had percutaneous coronary intervention the following day. Of the remaining 12 patients, 2 left the ED against medical advice and 6 had no further cardiac testing during their admission. The other 4 patients had normal nuclear perfusion studies the following day. In each of these 4 cases, functional testing was not available through the ED due to the time of day and all 12 patients were hospitalized for no more than 48 hours.
Of the discharged patients (n=19), 17 were confirmed to be alive at 30 days by chart review or phone discussion. Two patients had no data in our EMR subsequent to their index ED visit and were unable to be reached by phone for follow-up. There were no discrepancies between information obtained from patient phone calls and from the EMR. There were no episodes of major adverse cardiac events in the 30-day follow-up period for these individuals. Two patients revisited our ED during the follow-up period and both were admitted to non-cardiology services. One patient presented with altered mental status and the other patient was found to have abdominal pain and diabetic ketoacidosis. For both patients, no cardiac abnormalities (or suspicion for cardiac pathology) were documented by the emergency physicians or the inpatient teams.
DISCUSSION
We have expanded the analysis of a triage cardiology program to include patients for whom consultation was provided solely by phone. Our results suggest that phone consultation with a triage cardiologist can safely facilitate discharge from the ED in patients whose HEART scores would have otherwise suggested admission. While the overwhelming majority of patients were both high-risk and were admitted to a cardiology service, nearly 10% were safely discharged when the HEART pathway would have recommended admission. The access center and ED physician documentation suggest that without a discussion with the cardiologist, these patients would have been admitted to an inpatient cardiology team and those that underwent functional testing would not have been considered candidates for such testing by ED physicians had the ED-cardiology discussion not occurred.
There were no differences in history and ECG findings between the high-risk discharge group and the high-risk admission group. Likewise, emergency physician experience and timing of the consult request do not account for the discordance. It is plausible emergency physicians may have felt more comfortable ordering cardiac testing after discussion with the triage cardiologist as 60% of the high-risk discharge group had reassuring test results prior to discharge. This finding provides evidence in support of the premise that a high-risk HEART score does not automatically exclude the possibility of ED testing. The value-added by cardiologist phone-consultation may be in the facilitation of ED testing in a population for whom that option would not be considered otherwise. If demonstrated in a larger prospective cohort, a strategy of ED testing guided by cardiology phone-consultation in selected high-risk HEART pathway patients could safely result in less time spent in the hospital and reductions in the cost of care, analogous to the strategy of early discharge for low-risk HEART pathway patients [6].
For several of the high-risk discharges that did not undergo ED testing, the triage cardiologist was able to discuss the case with the patient’s primary cardiologist or facilitate timely follow-up in cardiology clinic, which likely also assisted with discharge plans. As ECGs can be readily reviewed during a phone conversation, it is possible that a more reassuring interpretation of the ECG by the cardiologist may have lowered the threshold for discharge with or without further testing, as suggested in a prior report [3].
Low-risk patients were admitted at approximately the same rate as high-risk patients were discharged. In 2 of those cases, the emergency physician’s concern was sufficient to warrant cardiac testing, which turned out to be abnormal despite a HEART pathway score that recommended discharge. It is possible that these cases could be due to undercoding of the HEART score during chart review, although they could also represent actual ‘false-negatives,’ as perfect discrimination cannot be a realistic expectation of any risk-stratification tool, including the HEART pathway. Examining the experience levels of emergency physicians caring for this group of patients admitted despite low HEART scores suggests that disposition decisions favoring admission may have been driven by a lower comfort level with either discharge or ED-based cardiac testing, which is consistent with prior work in this area [7,8]. In addition, less experienced emergency physicians may not be as familiar as their more experienced colleagues with the option of engaging the triage cardiologist to assist with arranging robust outpatient follow-up.
Limitations
This study has several important limitations. The absolute number of discordant outcomes is relatively small, as the cohort was primarily composed of high-risk patients that were admitted at a single institution, which may also limit generalizability. Similarly, the relatively small number of discharges, coupled with the retrospective calculation of the HEART score, makes assessing the safety of triage-cardiology phone consultation less robust. In addition, complete assessment of safety outcomes was not achieved, although reliable follow-up in this regard was obtained for approximately 90% of discharged patients. The temporal lag between the index ED visit and follow-up phone calls may have led to under-reporting of adverse events due to incomplete recall by patients. There may be as yet unidentified factors that influence disposition decisions that were not accounted for in this study. Again, small sample size limited our ability to conduct multi-variate analyses to more precisely quantify the contributors to discordance.
In this study, HEART scores were derived retrospectively from ED physician documentation, as was the case in prior work [3] and in a larger, more recent study [5]. We suggest that the impact of this approach in the current cohort is small and that the main source of discrepancy between retrospective and prospective HEART scores would be ‘missing’ data rather than inaccurate data (i.e., we presume that data that were recorded in ED documentation are accurate, but acknowledge there exists the possibility of missing data because ED physicians were not prospectively instructed to focus on specific historical points). The key component of the HEART score that is susceptible to retrospective/prospective discrepancies is the history, as the other components are objective and were universally obtained/collected in a prior cohort [3]. If history features were not present in the ED documentation, it is possible that these ‘missing’ data could have influenced the history component of the HEART score (in either direction) and thus resulted in a different categorization of HEART score-based risk. Therefore, for there to be a possible discrepancy, there needs to be not only an ample amount of missing history features data that, if present, could have resulted in a change in the history score, but also an overall risk-categorization that would be ‘susceptible’ to that change in the history score. For example, if a patient were already in the high-risk category based on a retrospectively calculated HEART score and, hypothetically, the analogous prospectively calculated history score were higher due to capturing previously ‘missing’ data, the risk-category of that patient would not change. In reviewing the primary data in our predominantly high-risk cohort, <10% of all patients and approximately 5% of discharges meet these criteria, which suggests a relatively small impact on our results of retrospectively calculated HEART scores.
In summary, for patients undergoing evaluation for chest pain in the ED, our findings suggest it may be reasonable to consider extending the purview of triage-cardiology input to phone-consultations, when circumstances do not permit bedside evaluation. These phone discussions, which could include simultaneous review of ECGs and a summary by the cardiologist in the EMR, may help facilitate cardiac testing and aid in disposition planning (i.e., by facilitating timely outpatient follow-up), particularly when the emergency physician is unsure of the optimal disposition strategy or the HEART pathway suggests the patient should be admitted.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This work was supported by CTSA award No. UL1TR000445 from the National Center for Advancing Translational Sciences. Its contents are solely the responsibility of the authors and do not necessarily represent official views of the National Center for Advancing Translational Sciences or the National Institutes of Health. Dr Yiadom was supported by K12 National Heart, Lung, and Blood Institute’s Emergency Care K12 Research Training Program at Vanderbilt Medical Center, award number 5K12HL109019 (not specifically for this work).
The authors wish to acknowledge Jacob Fleming, Alec Pawlukiewicz, David Stonko, and Kaitlyn Weeber for their assistance with chart review and follow-up phone-calls.
References
Article information Continued
Notes
Capsule Summary
What is already known
Efficient and effective risk-stratification of the >8 million patients that visit the emergency department each year for evaluation of chest pain remains challenging for emergency physicians, inpatient providers, and hospital administrators.
What is new in the current study
In approximately 20% of cases, disposition recommended by the History, Electrocardiogram, Age, Risk factors, Troponin (HEART) pathway is discordant with actual disposition made after phone consultation with a cardiologist; and following phone-consultation with a cardiologist, selected patients categorized as high-risk and in need of admission by the HEART pathway may be able to undergo functional testing in the emergency department and be safely discharged if test results are reassuring.