50% duty cycle may be inappropriate to achieve a sufficient chest compression depth when cardiopulmonary resuscitation is performed by female or light rescuers
Article information
Abstract
Objective
Current guidelines for cardiopulmonary resuscitation recommend chest compressions (CC) during 50% of the duty cycle (DC) in part because of the ease with which individuals may learn to achieve it with practice. However, no consideration has been given to a possible interaction between DC and depth of CC, which has been the subject of recent study. Our aim was to determine if 50% DC is inappropriate to achieve sufficient chest compression depth for female and light rescuers.
Methods
Previously collected CC data, performed by senior medical students guided by metronome sounds with various down-stroke patterns and rates, were included in the analysis. Multiple linear regression analysis was performed to determine the association between average compression depth (ACD) with average compression rate (ACR), DC, and physical characteristics of the performers. Expected ACD was calculated for various settings.
Results
DC, ACR, body weight, male sex, and self-assessed physical strength were significantly associated with ACD in multivariate analysis. Based on our calculations, with 50% of DC, only men with ACR of 140/min or faster or body weight over 74 kg with ACR of 120/min can achieve sufficient ACD.
Conclusion
A shorter DC is independently correlated with deeper CC during simulated cardiopulmonary resuscitation. The optimal DC recommended in current guidelines may be inappropriate for achieving sufficient CD, especially for female or lighter-weight rescuers.
INTRODUCTION
In cardiopulmonary resuscitation (CPR), achievement and maintenance of sufficient depth of chest compressions is critical for the survival of cardiac arrest victims [1-5]. Various efforts have been attempted to identify efficient means of maintaining sufficient chest compression depth [6-10]. Current CPR guidelines emphasize not only the depth, but also other technical components of chest compression, such as rate, recoil property, interruption time, and duty cycle (DC), in terms of achieving and maintaining good quality [11]. The term “duty cycle” means the proportion of the time spent compressing the chest from the start of 1 cycle of compression and the start of the next. Although DCs ranging from 20% to 50% can result in adequate coronary and cerebral perfusion [12-15], a DC of 50% is recommended in the current guidelines because it is easy to achieve with practice [11]. However, this recommendation does not consider possible interactions of the DC with other chest compression quality factors, such as the depth and rate, as has been studied elsewhere [16]. Moreover, a recent study has shown that a faster down-stroke, which is thought to induce a shorter DC, correlates with a deeper compression depth during metronome-guided CPR [17]. Baseline data of volunteers who participated in the study suggested a correlation between physical characteristics, such as sex, height, and weight, with the depth of chest compressions; further, there may be a possible interaction among the physical characteristics, DC, and depth. If so, the tendency of deeper compression with lower DC, as shown in the results, might differ between rescuers with different physical characteristics. Current recommendations for a 50% DC may be inappropriate for induction of chest compressions with sufficient depth for certain rescuers. We therefore aimed to assess true correlation of DC with the depth of chest compressions considering the interaction of physical characteristics, and determine if 50% DC is inappropriate to achieve sufficient chest compression depth in certain conditions, using the regression equation built from a previously collected data set.
METHODS
Three hundred twenty-four compression-only CPR performance data sets, independently conducted by 27 volunteers, were included in the analysis [17]. This prospective, randomized, cross-over trial was performed under the approval of our institutional review board. Senior medical students who had finished two sessions of regular CPR training courses based on the American Heart Association Basic Life Support course within the past year, performed 12 sets of continuous chest compressions for 1.5 minutes (30 seconds for practice and 1 minute for measurement) following the prepared metronome guidance in a random sequence with three down-stroke patterns (normal, fast, and very fast), and four rates (80, 100, 120, and 140 compressions/min), based on a random number table generated by Microsoft Office Excel 2007 (Microsoft Corporation, Redmond, WA, USA) (Fig. 1). A Resusci Anne manikin with a PC skill-reporting system (Laerdal, Stavanger, Norway) was used to measure and record CPR data. Chest compression guiding sounds were synthesized using Reason audio synthesis software (Propellerhead, Stockholm, Sweden) with the Waves gold bundle signal processing software package (Waves, Knoxville, TN, USA). Participant baseline data such as sex, age, body weight, and height measurements were collected, and physical strength was gauged through a self-assessment that used a 10-point visual analogue scale. Average compression depth (ACD, mm), average compression rate (ACR, numbers/min), DC (%), and proportion of chest compressions with incomplete release and incorrect hand position (%) were all measured and recorded using the PC skill-reporting system.
Flow diagram of study performances. The participants performed 12 sets of continuous chest compressions for 1.5 minutes (30 seconds for practice and 1 minute for measurement) following the prepared metronome guidance in a random sequence. To avoid the effect of rescuer fatigue, sufficient rest time was allowed between the trials (more than 60 minutes), and the maximum number of performances in a day was limited to 4. CPR, cardiopulmonary resuscitation.
Every performance was analyzed to assess the effect of DC, ACR, baseline data, and self-assessed physical strength on ACD. Analysis of covariance (ANCOVA) was performed to detect differences in ACD by rescuer sex, while considering the effect of other covariates that were significant on univariate analysis. Multiple linear regression analysis was performed, including every parameter showing significant result in ANCOVA as an independent variable and ACD as a dependent one. Expected ACD values of performances with 50% DC, by compression rate, were calculated for each sex based on median body weight and self-assessed physical strength. The same calculation was performed according to the quartile values of weight in each sex.
Mean and standard deviation values were used to report the data with a normal distribution, and a median with interquartile range was used for the nonparametric variables. The results of the statistical tests were considered significant when the P-value was less than 0.05. Microsoft Office Excel 2010 (Microsoft Corporation) was used to record and analyze the data, and IBM SPSS Statistics ver. 21.0 (IBM Corp., Armonk, NY, USA) was used for statistical calculations.
RESULTS
Participant baseline data are summarized in Table 1. The distribution of participant body weight is described in Fig. 2. There was a significant difference in mean value of ACD between female and male rescuers (Fig. 3A). Not only DC and ACR, which were major determinant of compression depth in previous works [16,17], but also height, weight, and self-assessed physical strength of rescuer, which showed significant correlation with ACD in newly performed analysis, were included in ANCOVA as covariates (Fig. 4). ANCOVA revealed that sex and all covariates were correlated with ACD except the height of rescuer (P-values of self-assessed physical strength and height = 0.010, 0.794, respectively, all other < 0.001) (Fig. 3B).

Depth of chest compression by rescuer sex. (A) Distribution of average compression depth (ACD) according to the sex of participants. The P-value was calculated from the Mann-Whitney U-test. (B) Estimated marginal means of ACD according to the sex of participants, which were calculated from analysis of covariance.

Correlation of the average compression depth with (A) height of the participant, (B) weight of the participant, and (C) self-assessed physical strength of the participant. Line, equation, and P-values were calculated from simple linear regression analysis.
DC, ACR, body weight, male sex, and self-assessed physical strength were significantly correlated with ACD on multiple linear regression analysis (adjusted R2 = 0.595, P < 0.001) (Table 2). Expected ACDs according to ACR and sex calculated from the regression equation are shown in Table 3. Similar calculations according to the quartiles of weight and sex of the rescuers are shown in Table 4.

Results of the multiple linear regression analysis to determine the factors contributing to the average depth of chest compression
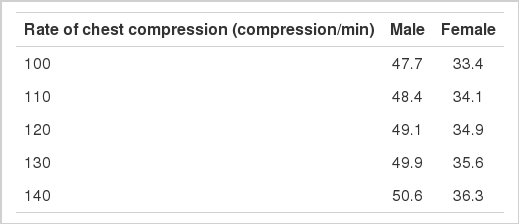
Expected values of average compression depth (mm) with the duty cycle of 50%, according to the rate of chest compressions and the sex of rescuer, calculated from the regression equation
DISCUSSION
This is the first study to assess DC of chest compression and other components that may interact with each other during CPR. Results suggest that a shorter DC is an independent predictor of deeper chest compression and imply that the 50% DC recommended in current CPR guidelines may be inappropriate.
Participant baseline data suggest the possibility of an association between depth of chest compression and rescuer body weight, height, sex, and self-assessed physical strength. Body weight, height, and self-assessed physical strength showed linear association with ACD in simple regression analysis. A possible sex effect on ACD was supported by the result of ANCOVA, which confirmed that the difference in ACD was caused by the rescuer’s sex.
As shown in our previous work, a shorter DC, which was interpreted as a shorter compression-phase, is correlated with a deeper chest compression in a linear manner, regardless of the speed of chest compressions [17]. Results of the multiple linear regression analysis confirmed that a shorter DC is an independent predictor of deeper chest compressions, which means that a shorter DC is correlated with a deeper compression regardless of the sex or body weight of the rescuer. Moreover, the direct correlation between ACR and ACD supported the results of Chung et al. [16], which showed that a higher compression rate is associated with deeper chest compression. We also identified a significant difference in ACD based on sex; male rescuers achieved a significantly greater ACD than female rescuers. This finding is consistent with that of Peberdy et al. [18], which showed that the sex and age of the caregiver affect chest compression depth. Age was not a statistically significant variable in our study, even on simple comparison. This discordance may be due to the narrow age range of our participants, as we enrolled only students from one class in our medical school. The association between self-assessed physical strength and ACD is also an interesting result. However, participant baseline characteristics should not be generalized as factors that directly influenced the quality of chest compressions (although they were statistically significant on multivariate analysis), solely based on our results. Rather, they would be better treated as covariates correcting the effect of the factors that were directly assessed during every independent performance, including DC and ACR, because the baseline data were used repeatedly in the analysis. Further study is necessary to investigate the actual association of self-reported physical strength with the depth of chest compressions.
The independent inverse correlation between DC and ACD observed in our study may be somewhat contrary to the results of previous studies, which suggested that longer DC induces increases in aortic pressure and cerebral blood flow [13,19]. However, it should also be noted that DC increased, while the force of chest compression was fixed in both studies; this did not allow us to analyze the interaction between the DC and compression force. Considering this information, our finding of a correlation between DC and ACD may suggest an interacting effect of DC on chest compression force.
Expected ACDs calculated from the regression equation provide one of the most important findings: 50% DC, as recommended in the current CPR guidelines, may not be appropriate to achieve sufficient chest compression depth, especially for female and lighter-weight rescuers. Furthermore, some guidelines recommend an ACR ranging between 100/min and 120/min and a DC of 50%; however, considering these values, our expected ACDs were below the recommended depth of chest compressions. The expectation of sub-optimal chest compression depth with 50% DC even with faster rates, which were known to enhance ACD in previous studies [16,17], implies the necessity for a shorter DC than the current recommendation. Calculation of results according to rescuer weight quartiles indicated that expected ACD for only male rescuers with body weights of quartile 3 (75 percentile) are in the recommended range, which also supports the inappropriateness of the recommended 50% DC. This calculation result suggests that the currently recommended DC may be generally inappropriate for light rescuers, considering that the multivariate analysis identified the body weight of the participant as an independent predictor of chest compression depth. Although our results were from a crossover trial, because of which the specific results obtained from the baseline data of the participants should not be directly accepted (as mentioned above), their strong association with ACD might reflect the trend. Hence, the recommendation of 50% DC should be reconsidered at least for female or lighter-weight rescuers.
Our study had a few limitations. First, the study was a reanalysis of previously collected data derived from simulated CPR performances. Subsequently, direct implementation of our findings to a clinical setting should be performed with great caution. Furthermore, baseline data of the participants were used repetitively in the multivariate analysis, because the datasets were obtained from cross-over trials conducted by a relatively small number of participants. Hence, it might cause some deviation of the results, even if the performances were conducted in a fully independent manner. Second, every chest compression in the study was performed with audio tone guiding because of the need to induce a certain DC range. Therefore, there could have been an additive effect of metronome guidance on the chest compression quality. Third, baseline fitness of the participants was measured by a self-reported scale, which was not an objective method and might cause some flaws in the results.
In conclusion, shorter DC is independently correlated with deeper chest compression during simulated CPR and the recommended DC in the current guidelines may be inappropriate for achieving sufficient compression depth, especially for female or lighter-weight rescuers.
Notes
No potential conflict of interest relevant to this article was reported.
References
Article information Continued
Notes
Capsule Summary
What is already known
A duty cycle of 50% is recommended for chest compressions during cardiopulmonary resuscitation due to its ease of achievement with training.
What is new in the current study
Current recommendations for duty cycle may be inappropriate to achieve a sufficient chest compression depth especially for female or light rescuers.