Rapid deployment of an emergency department-intensive care unit for the COVID-19 pandemic
Article information
Abstract
The coronavirus disease 2019 (COVID-19) pandemic mandated rapid, flexible solutions to meet the anticipated surge in both patient acuity and volume. This paper describes one institution’s emergency department (ED) innovation at the center of the COVID-19 crisis, including the creation of a temporary ED–intensive care unit (ICU) and development of interdisciplinary COVID-19–specific care delivery models to care for critically ill patients. Mount Sinai Hospital, an urban quaternary academic medical center, had an existing five-bed resuscitation area insufficiently rescue due to its size and lack of negative pressure rooms. Within 1 week, the ED-based observation unit, which has four negative pressure rooms, was quickly converted into a COVID-19–specific unit, split between a 14-bed stepdown unit and a 13-bed ED-ICU unit. An increase in staffing for physicians, physician assistants, nurses, respiratory therapists, and medical technicians, as well as training in critical care protocols and procedures, was needed to ensure appropriate patient care. The transition of the ED to a COVID-19–specific unit with the inclusion of a temporary expanded ED-ICU at the beginning of the COVID-19 pandemic was a proactive solution to the growing challenges of surging patients, complexity, and extended boarding of critically ill patients in the ED. This pandemic underscores the importance of ED design innovation with flexible spacing, interdisciplinary collaborations on structure and services, and NP ventilation systems which will remain important moving forward.
INTRODUCTION
Coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 virus, has rapidly become a worldwide pandemic with over 44,000 COVID-19 confirmed cases and greater than 25,000 deaths in New York State as of September 10, 2020 [1].
The Mount Sinai Hospital (MSH) emergency department (ED) diagnosed the first New York State case of COVID-19 on March 1, 2020 in New York State. By April 1, the ED was admitting an average of 33 patients with COVID-19 to the hospital per day and discharging many more without confirmatory testing, in line with guidelines at that time [2,3]. The physical layout of the ED was poorly suited to minimize the transmission risks of the COVID-19 virus with even more severely limited space for the high volume of critically ill patients. Thus, the pandemic forced a rapid adaptation and innovation of the ED physical space and workflows [4,5]. This study details the ED’s rapid structural changes, staffing transition, and physical updates for critically ill patients to offer lessons learned.
SETTING
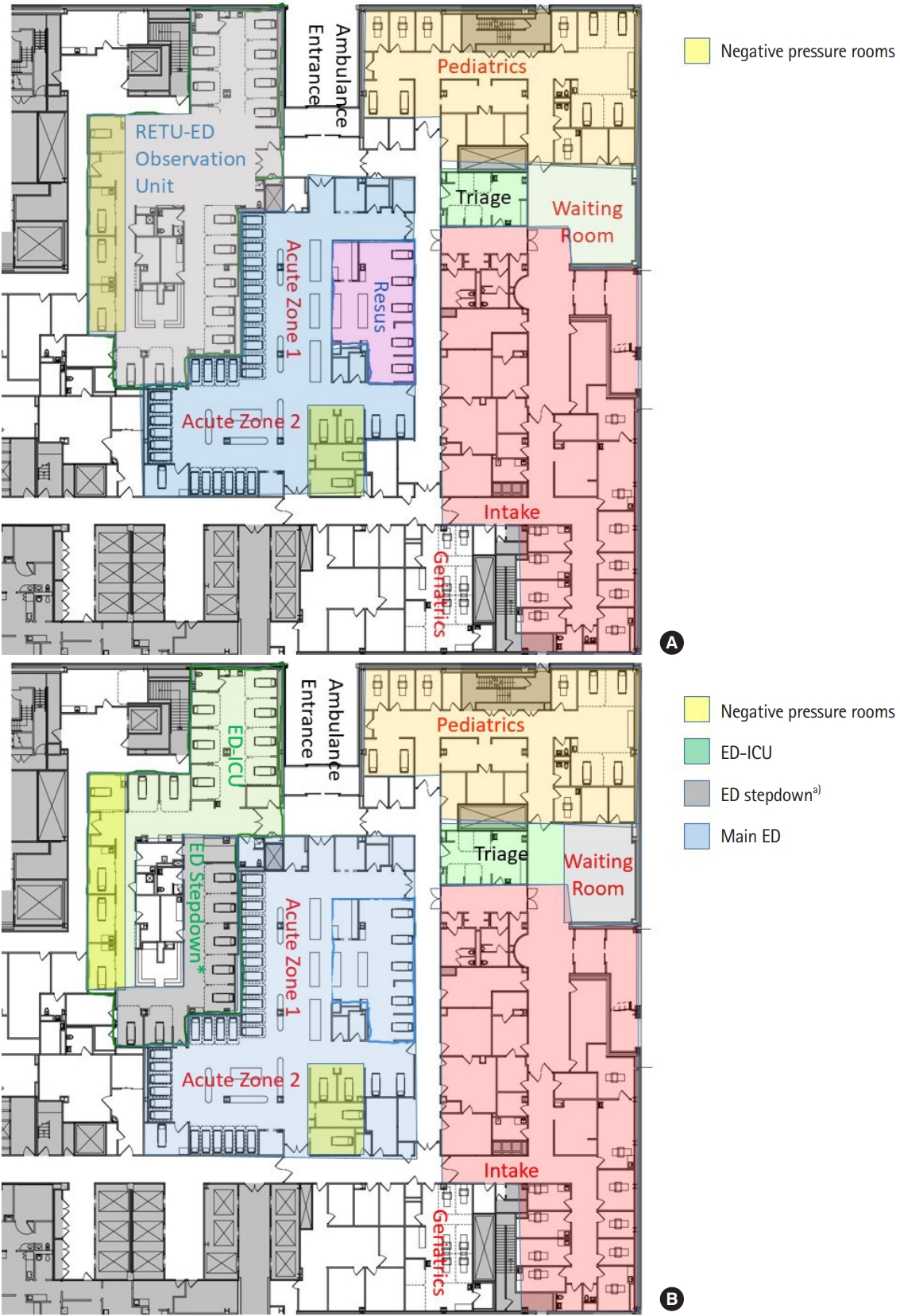
The MSH ED is located on the upper east side of Manhattan, in New York City. It is an 1,139-bed quaternary care academic hospital with 104 intensive care unit (ICU) beds, typically operating at an average >90% capacity. Over the past two decades, patient volumes have outgrown the 18,000-square foot department. The pre-pandemic layout of the department is detailed in Fig. 1. The adult MSH ED was divided into four main areas: one section for low acuity ambulatory patients, two sections for midacuity non-ambulatory patients, and a resuscitation area for high acuity patients (Fig. 1A). Adjacent to the adult ED was the pediatric ED and an observation unit. Across all ED sections, only ten rooms had respiratory isolation capabilities (i.e., negative pressure [NP] for airborne precautions). Due to high volume at baseline, physical space between critically ill patients was minimal throughout the department. During the 2 months between March and April 2019 the ED had 13,512 visits where during the COVID-19 pandemic that same period had 11,417 visits. The limitations of the ED size and layout were amplified during the pandemic.
INITIAL CHALLENGES
While the ED had a surge capacity plan prior to COVID-19, these emergency preparations were inadequate to meet the scale of the COVID-19 pandemic in New York City. The existing plans did not entail services, resources, and safeguards for such a large surge of critically ill patients, the high need for respiratory isolation, or the prolonged duration of disease activity. The principal challenge posed by COVID-19 was its transmissibility coupled with its unknown lethality and a lack of baseline population immunity. The initial goal for ED management was to accommodate every possible and confirmed COVID-19 patient (or family) in a NP room from arrival to discharge or admission [6-8]. However, increased daily ED volume of suspected or confirmed COVID-19 cases—a rise of 86% by week 2 of the pandemic—led to a shortage of isolation rooms. This was further exacerbated by the increasing frequency of boarding by admitted ED patients awaiting inpatient bed availability in ward isolation rooms and units. Providers were forced to perform aerosolizing procedures either in bays open to the entire ED or in a general isolation room without adequate ventilation, with limited options to transfer patients in and out of NP rooms due to the complexity of moving such unstable patients in a timely fashion. Furthermore, the shortage of NP rooms severely encumbered the initiation and utilization of non-invasive ventilation (NIV) (e.g., high-flow nasal cannula [HFNC] and non-invasive positive pressure ventilation [NIPPV]).
An additional challenge was ED crowding and boarding of inpatients, especially those on invasive mechanical ventilation. Prolonged boarding of ICU patients in the ED has been repeatedly associated with worse patient outcomes in prior studies [9-13]. Unsurprising, daily arrivals of critically ill patients with COVID-19 outpaced the hospital’s expansion of existing inpatient ICUs and construction of new ICUs. Compounding this situation, hospital cohorting required patients to wait for the in-house severe acute respiratory syndrome coronavirus two polymerase chain reaction assay results before unit and inpatient team assignments. Further, the critical care physicians who previously co-managed boarding ICU patients were deployed to care for patients in the expanded inpatient ICUs [14]. As a result, the ED needed a significantly modified or expanded critical care space, change in the critical care staffing approach, and redesigned services to accommodate the ongoing influx and complex care of critically ill patients [15-18].
EVOLUTION OF THE SPACE
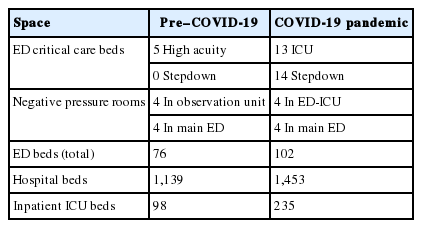
The observation unit, adjacent to the ED, was an ideal place for critical care expansion due to existing access to the ambulance bay, four large NP rooms, and present infrastructure for critical care bay support. Supported by both ED and hospital leadership, steps began to convert this space into a temporary ED-based ICU [15,16,19]. An overview of physical space changes is found in Table 1.
Thirteen critical care bays and 14 step-down beds were constructed in partnership from hospital engineering, biomedical supplies, respiratory therapy, and supply management. The department of pharmacy, led by ED pharmacists, restocked the medications available in the new ED-ICU zone to include rapid sequence intubation agents, vasopressors, inotropes, paralytics, and sedatives.
Infection precautions for COVID-19 positive patients throughout the hospital were a combination of ‘contact isolation’ requiring a gown and gloves and ‘special droplet’ precautions requiring a surgical mask and face covering, plus an N-95 mask for aerosolizing procedures. N-95 masks and face shields were worn continuously in this zone to conserve personal protective equipment. Intubations required full personal protective equipment and to be done in a NP room, discarding all personal protective equipment except for the N-95 mask after the procedure.
STAFFING EXPANSION
The severity of illness associated with COVID-19, nursing resources needed at the bedside during intubation or initiation of NIPPV, as well as requirements of minute-to-minute provision of ICU and stepdown level of care were all factors taken into consideration when developing the staffing model for the ED-ICU. An overview of staffing changes is found in Table 2.
Nurse and ED technician staffing
Nursing leadership determined that five nurses 24/7 for the 27-bed zone, with an additional three nurses 12 hours per day with staggered shifts during peak day hours was needed to staff the new ED-ICU. After direct feedback from frontline providers, nursing assignments were designated to certain rooms instead of the entire unit. New patients in need of immediate airway intervention received a dedicated nurse. Once intubated or on stable HFNC/NIPPV settings, patients were handed off to a nurse covering multiple stable, critically ill patients. To help manage throughput, a sixth full-time registered nurse (RN), designated as Lead RN, was added at the end of the first week to the ED-ICU. Three full-time ED technicians provided ancillary support to the area.
Depending on critical care patient volume, the ED nursing director made real-time deployment decisions and shifted staff including RNs and technicians to the busiest areas in the department. Additional experienced nurses were deployed to the ED from closed procedural areas to support staffing the other areas of the ED while the primary ED RN staff were flexed to the ED-ICU.
Provider staffing
Given the anticipated volume and acuity, the new COVID-19 critical care section was staffed with expanded physician and advanced practice practitioner (APP) coverage. In contrast to the original model with only 11 hours a day of attending physician support, the new ED-ICU had full-time support by a dedicated emergency medicine attending and two trainees or APPs (either PGY-2 or above emergency medicine residents or senior physican assistants) 24/7. The new ED stepdown was staffed with a dedicated attending 16 hours per day and two EM residents or physican assistants. This staffing enabled two full resuscitations to occur simultaneously by two different ED attending’s when needed.
MSH ED has six emergency physicians that are dual boarded in both emergency medicine and critical care medicine. While these physicians preferentially staffed the ED-ICU, inpatient ICU staffing demands led to the majority of ED-ICU shifts being covered by non-intensivist faculty. The ED intensivists worked to help develop novel protocols and adapt existing inpatient ICU for the critically ill COVID-19 patients in the pre-ICU setting, with implementation at all the EDs in the Mount Sinai Health System [20].
Respiratory therapy
Prior to March, the ED had one dedicated respiratory therapist (RT) per shift. However, the volume of procedures and intubated patients required two full-time RTs with a third added for 12 hours a day during peak hours to help support the new demand. Several solutions were implemented to help support patient care for respiratory management, including ED physician training on a new ventilator and non invastive positive-pressure ventilaltion (NIPPV) machines setup and operation, hospital leadership allowance for a physician and RN to transport patients on portable ventilators and NIPPV without respitortory therapist (RT) assistance, and Operating Room CRNAs (certified registered nurse anesthetists) deployment to the ED to help with intubations and ventilator management.
ELASTICITY OF SERVICES AND WORKFLOW
Triage
In the beginning of the pandemic, it was posited that a subset of critically ill patients would have a low-enough pretest probability of COVID-19 that they should be separated from the high-likelihood COVID-19 patients [21]. However, this split triage model was abandoned after a three-day trial due to the rapid drop-off in non–COVID-19 patients [22], and the high proportion of patients without respiratory complaints who nonetheless had COVID-19. All Emergency Severity Index 1 patients, and the majority of Emergency Severity Index 2 patients were triaged directly to the ED-ICU. Patients in need of rapid respiratory intervention (intubation or NIV initiation) were triaged directly into one of the four NP rooms. The remainder were triaged to the ED-ICU or stepdown depending on their perceived stability. The ED-ICU and stepdown saw a large number of critical patients during the COVID-19 pandemic (Table 3).
Respiratory resuscitation workflow
During the first 5 weeks of the pandemic (March 22, 2020 to April 26, 2020), 878 patients were seen in this new space, with the number of intubated or NIV patients well exceeding the NP room capacity. Use of the four NP rooms was reserved for intubations and NIV use. In this time period, 127 patients required intubation in the ED, almost five times the number of patients intubated in 2019 (27). Once intubated, the patients were rapidly moved to one of the nine open ED-ICU bays where further care was provided. To further conserve limited NP space, intubated patients were deemed safe for regular isolation due to the ventilator’s closed circuit with an attached viral filter. Similarly, patients on stable NIPPV or HFNC settings were moved to the four NP rooms in the other ED zones to save ED-ICU NP rooms for possible intubations.
Continuously moving patients out of the NP rooms to maintain their immediate availability for new arrivals was a great logistical challenge. Collaboration with environmental services was crucial to increase staffing to enable the cleaning and rapid turnover of the NP rooms which allowed for safe intubations. A nurse was assigned to solely manage the NP rooms to ensure that these critically ill patients received dedicated attention. This designated RN, the RTs and providers were able to continually assess for respiratory deterioration. Importantly, this nurse and the RT gained critical experience in rapidly moving recently intubated patients out of the NP rooms and providing nurse-to-nurse ICU-level handoffs in the ED-ICU and to the inpatient teams. The group that executed this transition included doctors, nurses, APPs, operational management staff and the ED performance improvement specialist. This group met daily, at a minimum, to ensure that we did not leave critical components out of the transition.
Radiography
All patients with suspected COVID-19 and any respiratory symptoms received a portable, anteroposterior chest radiograph. This was done to maintain the ED X-ray zone for non-respiratory plain films and reduce the deep cleaning needed between patients. Computerized tomography scans required coordination with the computerized tomography suite to maintain isolation precautions and protect the radiology staff.
Palliative care
Recognizing the need for expanded services with limited patient contact, the palliative care department initiated a 24/7 hotline for palliative care consults for all six Mount Sinai Health System EDs and deployed an in-person attending (often accompanied by a fellow or resident) to the MSH ED 12 hours per day. They functioned as core members of the team, continuously rounding and consulting on the majority of new patients as well as those with rapidly worsening clinical statuses [23]. They assisted not only in helping to cognitively offload the stretched ED providers, at a time when patient’s family could not be at the bedside due to infection risks, but also in helping providers feel that despite the crisis they were continuing to provide care consistent with patient/family wishes [24].
Admission flow and boarding time
All hospital inpatient beds, including ICU beds, were rapidly divided into COVID-19 positive or negative units. The median turnaround time for this test was 7 hours, with a 95th percentile of 12 hours over the period in question. Additionally, whether due to collection technique or viral aggregation away from the upper airway, patients with negative COVID-19 swabs but with high suspicion of COVID-19 infection required repeated swabbing, thus extending boarding times. As such, no admitted patient could receive an inpatient bed assignment until a nasopharyngeal polymerase chain reaction resulted. Critically ill patients were similarly affected, as patients’ infection status had to be confirmed before assignment to either a COVID-19 specialized ICU or a nonisolation ICU, increasing numbers of ICU patients boarded in the ED for longer than average times, requiring ED-specific innovation to meet the needs of the patients.
DISCUSSION
The MSH ED rapidly adapted the delivery of critical care to meet the challenges of the COVID-19 pandemic [20]. An ED-ICU was rapidly built by converting the prior observation area (a 27-bed zone) [15,16,19,25]. A redesign of a new space in a large US academic hospital often requires months, if not years, of planning and negotiations with the varying hospital interests involved. With the pressure of high COVID-19 demand, this conversion was executed in approximately 1 week, from initial decision to full activation. Moreover, the unit functioned during the peak of the New York City COVID-19 epidemic largely as envisioned and required surprisingly few spaces or workflow modifications mid-course. Its success was due to the hard work of the leadership team and front-line providers and the collaboration across the institution.
Strong intradepartmental and interdepartmental relationships were critical to the implementation of the ED-ICU unit. Success required the rapid cooperation of leadership from departments across the hospital. ED medical, nursing, and operations leadership had weekly meetings with all these departments. The transition to daily or twice-daily huddles required little change. With all these departments rapidly assisting to modify their own workflows and/or staffing, the new space achieved more optimal function, effectiveness, and safety for patients and staff with caregivers supported and operating in a more familiar environment.
There were and remain many challenges. Despite the relative strengths of the new space relative to the main ED, it is worth noting that not every COVID-19 patient was able to be treated behind a closed door, let alone in a NP room. Efforts to convert the whole zone to NP ventilation systems were deemed impossible given engineering constraints. As the process of redesigning the main ED begins—a process initiated before the pandemic—these lessons from the COVID-19 ED-ICU will better prepare the department for the future.
The COVID-19 pandemic was a strain on the healthcare system of New York City as a whole. The Mount Sinai Health System rapidly adapted to meet the needs of the patients. The ED rapidly designed and created an ED-ICU to help optimize critical care for the sickest patients presenting to the ED. The space was adapted to help facilitate safe, high-quality care for many critically ill patients, as well as providing continued ICU level care as these patients waited for ICU beds.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
We would like to thank Dr Jagoda for all his support, mentorship, and leadership on this manuscript. We would also like to thank Hospital Throughput, Engineering, Environmental Services, Internal Medicine, The Institute for Critical Care Medicine, Patientn Transport, Radiology, Supply Chain Management, Respiratory Therapy, Security, Pharmacy, Laboratory, Office of the Chief Nursing Officer, Office of the Hospital President and CMO, Nutrition Services, and likely others who helped built and make the ED-ICU so successful.
References
Article information Continued
Notes
Capsule Summary
What is already known
COVID-19 pandemic hit New York City early in 2020 and resulted in a huge surge of patients to the emergency rooms across the New York City region.
What is new in the current study
We discuss the methods used to convert a zone of the emergency department into a critical care space able to take care of COVID-19 patients.