Preventable deaths in patients with traumatic brain injury
Article information
Abstract
Objective
The objective of this study is to evaluate the rate of and etiology for preventable deaths in patients with traumatic brain injuries (TBIs).
Methods
We conducted a retrospective, multicenter review of patients with TBIs who died within 7 days of their traumatic event from June 2008 to May 2009. Three board certified emergency physicians independently reviewed every case using a structured survey format. Cases were considered preventable deaths only if all physicians independently agreed the death was preventable. Management errors contributing to the preventable death were determined.
Results
Forty-one patients who died from TBI were eligible. Preventable deaths were identified in nine (22%; 95% confidence interval [CI], 11 to 28) cases. Fifty-six management errors were identified including 36 (64%; 95% CI, 50 to 77) in the emergency department and 13 (23%; 95% CI, 13 to 36) in the prehospital phase. Thirty (54%; 95% CI, 40 to 67) management errors were process-related, and 26 (46%; 95% CI, 33 to 60) were structure-related.
Conclusion
An important and measurable rate of preventable mortality occurs in the initial care of TBI patients. Errors were common and most occurred in the emergency department. In addition, errors were common in the prehospital phase but did not always lead to mortality. When analyzed by type of problem, both process-related and structure-related errors occurred in similar proportions.
INTRODUCTION
In 2009, 32,661 people died from injuries in Korea, making it the third leading cause of death after cancer and cardiovascular disease [1]. Furthermore trauma is the leading cause of death and disability in those one to 40 years of age and is the leading cause of years of productive life lost and economic lost [1]. Preventable deaths include those deaths which would not have occurred had the patient received appropriate care in a timely fashion. The preventable trauma death rate is currently a method to determine the performance of a country’s or region’s emergency medical system [2].
A prior Korean study of 131 trauma deaths from two tertiary and four secondary hospitals suggested the preventable death rate may be as high as 40.5% [3]. Furthermore, in this study, the preventable death rate was 22% for those with traumatic brain injury and 63% in those without brain injury. Data from three regional and six local Korean hospitals suggested a preventable death rate of 40% but may be as high as 56% in those with traumatic brain injury [4].
Many cases of traumatic brain injury require emergent neurosurgery and without appropriate, timely treatment, secondary brain injury may rapidly occur [5,6]. Previous studies on preventable trauma death focused on all severely injured trauma patients regardless of the presence of traumatic brain injury. The objective of this study is to identify the preventable death rate and reasons in patients with traumatic brain injury.
METHODS
We conducted a retrospective study of adult patients with traumatic brain injury treated at five hospitals in the Korean Traumatic Brain Injury Surveillance Network. Two in five hospitals were regional emergency medical centers and three of them were local emergency medical centers. The study was approved by the institutional review boards at all sites.
Study population
Patients older than 15 years of age who were treated for traumatic brain injury and died within 1 week from their initial presentation between June 1, 2008 and May 31, 2009 were included. The patients had traumatic brain injury but, could have other injury also. The definition of traumatic brain injury followed the International Classification of Diseases 10th edition (ICD-10) and included patients with any of the following codes: S01.0–S04.0, S06.0–S07.9, S09.7–S09.9, T01.0, T02.0, T04.0, T06.0, T90.1–T90.9. This corresponds to patients with brain hematomas (including intracerebral, epidural, and subdural hematomas), contusions, hemorrhage, or cerebral edema.
Patients were excluded if they received cardiopulmonary resuscitation on arrival to the hospital or if cranial computed tomography scanning was not performed. In addition, we excluded patients with incomplete medical records where we were unable to determine either the time of death or if the death was preventable.
Study protocol
A preventable death was defined as a death that is preventable if appropriate treatment was provided in a timely fashion. To determine if the patient with traumatic brain injury experienced a preventable death, the following three criteria were required [2]. First, the traumatic brain injury must be of such a degree that the patient is viable (i.e., the traumatic brain injury cannot be severe enough to cause death). Second, the treatment provided to the patient must be considered insufficient compared to standard treatment of traumatic brain injury as provided in the Advanced Trauma Life Support (ATLS) course guidelines and the Brain Trauma Foundation (BTF) guidelines [7,8]. Finally, the insufficient treatment must contribute to the death of the patient either directly or indirectly.
Traumatic deaths were divided into three categories [9]. First, nonpreventable deaths include those injuries so severe they are not amenable to current medical care. These include patients with injuries categorized as Abbreviated Injury Scale (AIS) score of 6 [10]. Second, potentially preventable deaths are those with very severe injuries, but are survivable with the current level of medical treatment. An example of a potentially preventable death would include a patient with a massive subdural hematoma who arrives at the hospital in time for emergent surgical decompression however, the patient died as they were transferred to a hospital without emergent neurosurgical capabilities. Thus, the injury was potentially preventable if the patient had initially been transported to an appropriate hospital. Finally, definitely preventable deaths are those injuries that are treatable based on the type of brain injury and capabilities of the initial treating hospital. An example of a definitely preventable death is the patient who arrives at a hospital with the neurosurgical capabilities to treat an epidural hematoma but the patient dies of brain herniation prior to identification of the epidural hematoma (delayed diagnosis).
We considered preventability in context to the following: injury severity, condition of the patient, and adequacy of treatment. Injury severity was based on the AIS score. Patient condition was based on the Revised Trauma Score. The presence of underlying disease and complications was determined from review of the medical history. Adequacy of medical treatment was based on treatments recommended in the ATLS course and the BTF guidelines. Through this process, cases were classified into one of three categories; definitely preventable, potentially preventable, or non-preventable.
Treatment deficiencies were divided into the following six ‘location’ categories: prehospital phase, transfer phase between hospitals, emergency department phase, operating room phase, intensive care unit phase, and ward phase. Treatment deficiencies were further divided into structure-related problems and processrelated problems. Structure-related problems included those secondary to an absence of appropriate facility, personnel, or equipment for timely diagnosis and treatment. Process-related problems included those due to inadequate treatment, diagnosis, or procedure.
We used an expert panel (professional study panel) composed of three specialists in emergency medicine to determine the outcome of interest. The medical records (including all radiographs and treatment) were reviewed independently by each member of the team.
The team underwent two formal training sessions prior to performing the record review. The research team visited each hospital, reviewed the medical records and radiographic images of all eligible patients and independently determined the outcomes.
We further categorized all potentially preventable and definitely preventable deaths into those that occurred at any point in treatment (i.e., both prehospital and hospital phase) and those occurring only during hospital treatment. Preventable/definitely preventable deaths during hospital treatment were determined based on the patient’s condition upon arrival at the hospital. After the outcomes were determined by each member of the research team, agreement between investigators was determined.
Data analysis
We calculated the preventable death rate among all traumatic brain injury patients including those occurring at the hospital level. We also calculated the preventable death rate by patient characteristics including expected probability of survival based on ICD- 10 injury severity score (ICISS) including patient’s gender, age, and mechanism of injury.
A preventable death was only considered present if all investigators independently agreed. Results are described with simple descriptive statistics. Categorical data are compared with Fisher’s exact test due to small cell size. The degree of agreement between investigators was measured with weighted Kappa values and 95% confidence intervals (CIs) were calculated. We additionally collapsed the definitely preventable and potentially preventable categories into a single category (preventable deaths). Alpha Xi Bach (Cronbach’s alpha) reliability coefficients were calculated for cases analyzed to three categories (definitely preventable, potentially preventable, or non-preventable) and two categories (preventable deaths or non-preventable) to determine internal consistency.
RESULTS
General characteristics of the population
A total of 27,409 trauma patients were evaluated at the study sites from June 1, 2008 to May 31, 2009 and 7,131 patients had head trauma. One hundred (1.4%) of the 7,131 patients died. Fifty-nine patients were excluded (Fig. 1). Therefore, the study population consists of 41 patients who died from traumatic brain injury during the time period. Characteristics of the study population are presented in Table 1. The median age was 58 years (interquartile range, 43 to 73 years). The median probability of survival was 64% (interquartile range, 57% to 79%).
Among 100 patients with traumatic brain injury, 59 patients were excluded and 41 patients were enrolled finally.
Preventable death rate
Nine (22%; 95% CI, 11 to 28) of 41 cases were determined to be potentially or definitely preventable. This included five (12%; 95% CI, 4 to 26) cases definitely preventable and four (10%; 95% CI, 3% to 23%) cases potentially preventable. Seven (17%; 95% CI, 9 to 25) cases of preventable deaths occurred secondary to errors in the hospital, including four (10%; 95% CI, 3% to 23%) cases definitely preventable and three (7%, 95% CI, 2% to 20%) cases potentially preventable (Table 2). The remaining two cases of potentially preventable deaths occurred prior to hospital arrival. The median age of patients with potentially/definitely preventable deaths was 70 years (interquartile range, 58 to 80 years).
As we focused on variables that influence preventable trauma death, preventable death rate was lower in the case of death caused by head trauma compared to non-head trauma (P=0.692). At the hospital level, it was higher in the case of death caused by head trauma (P=1.00). However both were not statistically significant.
When the ‘potentially preventable’ and ‘definitely preventable’ categories were collapsed into a single ‘preventable’ category, the preventable death rate was lowest (14.3% at the overall phase and 0% at the hospital phase) when probability of survival by ICISS was less than 50%. Interestingly, preventable death rate was highest (23.8% both at the overall and hospital phase) when probability of survival by ICISS was between 50% and 75%.
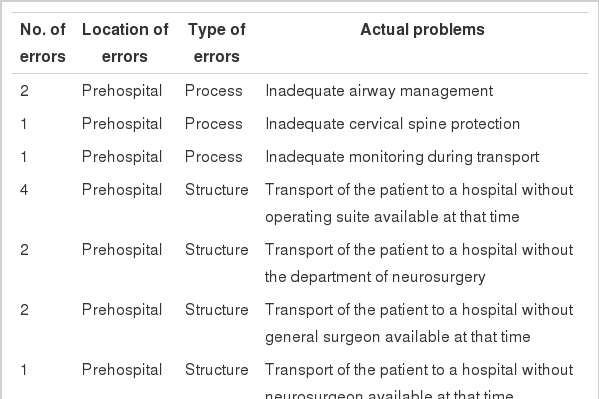
Errors related to the treatment process
Fifty-six treatment errors were identified in the 41 patients (1.4 errors/patient). Locations of errors were as follows: emergency department 36 (64%), pre-hospital phase 13 (23%), interhospital transfer 4 (7%), and intensive care unit 3 (5%). Types of problems include structure-related 26 (46%) and process-related 30 (54%). Process-related errors determined to be directly related to the death occurred in 26 (58%) cases. A list of the errors identified is presented in Table 3 (Appendix 1 for the details of actual errors and Appendix 2 [3,4] for the problem codes to classify the problems).
Agreement among investigators
Kappa values demonstrated moderate agreement between reviewers (kappa=0.46 for overall preventable death and 0.43 for hospital preventable death). Cronbach’s alpha reliability coefficient (for the categories of definitely preventable, potentially preventable, and non-preventable) showed good internal consistency (0.83 for overall preventable death and 0.86 for hospital preventable death). Cronbach’s alpha reliability coefficient (for the two categories-preventable versus non-preventable) showed very high internal consistency (0.91 for overall preventable death and 0.90 for hospital preventable death).
DISCUSSION
This study demonstrates that a substantial portion of traumatic deaths in patients with traumatic brain injuries are either definitely or potentially preventable. Furthermore, almost all of these preventable deaths occurred at the hospital stage of care and such data can be used to improve future care of patients with head injuries.
Our determined rates of preventable death are slightly lower than previously reported by Kim et al. [4] In that study, 29% of deaths were determined to be preventable. In the present study, preventable deaths were only considered to occur if there was a unanimous decision among reviewers. Thus, classifying preventable death into three categories may have produced slightly lower results. Establishing multi-investigator agreement in the likelihood of the possibility of preventable death and reclassifying preventability into two categories rather than three resulted in more internal consistency as expected.
We identified a small but measurable rate (4.9%) of preventable death in the pre-hospital processes. The result in this study (4.9%) was less than the 13.9% identified in Kim’s study [4]. Although primary traumatic brain injury occurs at the time of head injury, secondary brain injury can occur at a variety of times including the prehospital phase. Preventing secondary or delaying brain injury can substantially reduce the mortality rate [11]. Errors identified in the prehospital transport included inadequate airway management, inadequate monitoring, inadequate cervical spine protection, and transport to an inappropriate hospital.
Initial guidelines for the treatment of brain injured patients were introduced in 1995 and continue to be revised based on current evidence [8,12]. This includes guidelines for both the prehospital and hospital treatment of head injured patients. Following these guidelines improves survival rates [13]. These treatment guidelines are not uniformly adopted in emergency medical facilities in South Korea; therefore, it is difficult to determine if the facilities are in accordance with guidelines for the treatment of patients with traumatic brain injury. In this study, the majority of errors occurred in the emergency department with the transfer phase being the second most common location. Thus, in order to reduce death rates due to traumatic brain injury, introduction, uptake, and application of treatment guidelines in the emergency department is necessary.
The study by Kim et al. [4] suggested that as ICISS survival probability increased, preventable mortality increased. In this study, however, preventable mortality was not higher in those patients with a predicted survival >75%. In many countries, attempts are made to evaluate mortality by using Trauma and Injury Severity Score (TRISS) methodology. Expected ICISS probability is calculated from the ICD-10 empirical probability of survival, and is a substitute for the existing TRISS [14]. Proposed categories using TRISS probability of survival include the following: less than 25% probability of survival in the non-preventable cohort, 25% to 50% in the potentially preventable cohort; and 50% or more in the definitely preventable cohort [15,16]. These studies, however, demonstrate a higher probability of observed survival. As medical treatment has advanced since the TRISS methodology was developed in the 1980s, applying TRISS to current data, likely results in the higher than expected survival rates. Current evidence does not support this classification of ICISS probability of survival, but a categorization system is needed to compare rates of preventable death.
We identified a substantial number of medical errors in the treatment of head injured patients (Table 3). Most errors occurred in the emergency department treatment, and many of these could have been prevented. Actual errors in the emergency department are related to the consultation and work-up process (Appendix 1). These errors may perhaps be related to emergency department system or overcrowding. The second most common location for errors was in the prehospital phase although these contributed to patient mortality less often. We did not identify errors from the operating suite, although this likely reflects a limitation of the medical record review as opposed to an actual absence of errors. In this study, an important and measurable rate of preventable mortality was identified in head injured patients. Errors were common and most occurred in the emergency department. Furthermore, errors were common in the prehospital phase but did not always lead to mortality. When analyzed by type of problem, both process-related and structure-related factors occurred in similar proportions.
This study has a number of limitations. It is a retrospective medical record review subject to the limitations of that methodology. The sample size included was insufficient to statistically identify small differences. Second, the selected panelists’ area of expertise is in emergency medicine, and the results may be impacted by this expertise. A neurosurgeon or trauma surgeon may identify additional cases including errors that occurred in the operating suite or intensive care unit, or may have evaluated the preventability of cases differently.
This study enrolled patients at five hospitals belonging to the Korean Traumatic Brain Injury Surveillance Network. Although including multiple centers increases generalizability, it does not necessarily represent the entire population [17]. Despite these limitations, this study is the first study to calculate preventable mortality of severe traumatic brain injury patients. A larger multicenter study on patients with traumatic brain injury would further clarify the questions raised by this research.
In addition, it took several years to publish the results following our study. If possible, it would be valuable to incorporate more recent data and evaluate results from the larger population over a longer period.
Our small population study found that an important and measurable rate of preventable mortality occurs in the initial care of traumatic brain injury patients. Patient care errors were common, and most occurred in the emergency department. Errors were also common in the prehospital phase but did not always lead to mortality. When analyzed by type of problem, both process- and infrastructure-related errors occurred in similar proportions.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
Korea Centers for Disease Control and Prevention supported this study financially.
References
Appendices
Article information Continued
Notes
Capsule Summary
What is already known
Preventable death rate is currently a method to determine the performance of emergency medical system for trauma. Some reports from Korea showed the preventable death rate ranges from 30% to 40%.
What is new in the current study
Previous studies on preventable traumatic death focused on all severely injured trauma patients regardless of the presence of traumatic brain injury. We identified the preventable death rate and etiology in patients with traumatic brain injury.