Transcatheter arterial embolization in a haemorrhagic renal cyst with “rising tide sign”
Article information
A 69-year-old male patient presented to our emergency department with sudden left-sided flank pain associated with macroscopic haematuria. There was no history of trauma. Haemoglobin was 11.4 g/dL and abdominal multidetector computed tomography demonstrated a left simple renal cyst with a thin line of blood collection (Fig. 1A). At 48 hours, a second episode of massive macroscopic haematuria occurred. Haemoglobin has dropped to 9.3 g/dL and multidetector computed tomography demonstrated an increased level of blood collection into the left renal cyst (Fig. 1B). The patient underwent selective (Fig. 2A) and superselective (Fig. 2B) left renal artery angiography that showed two microspots of blood extravasation. Endovascular embolization was performed. Final angiographic control demonstrated occlusion of bleeding extravasation (Fig. 2C). At 12 hours, macroscopic haematuria had resolved and haemoglobin data showed an upward trend to 11.0 g/dL. Imaging follow-up at 72 hours (Fig. 3A) and 1 month (Fig. 3B) demonstrated left renal cyst reduction in size.

Contrast-enhanced multidetector computed tomography axial image (A) showing a left simple renal cyst (arrowhead), hyperdense thin line of blood collection (arrows), and a volume of 165.7 mL, and (B) at 48 hours demonstrating a well-delineated left simple renal cyst (arrowhead) and increased level of hyperdense blood collection (imaging sign called “rising tide”; arrows) with a total volume of 347.6 mL.
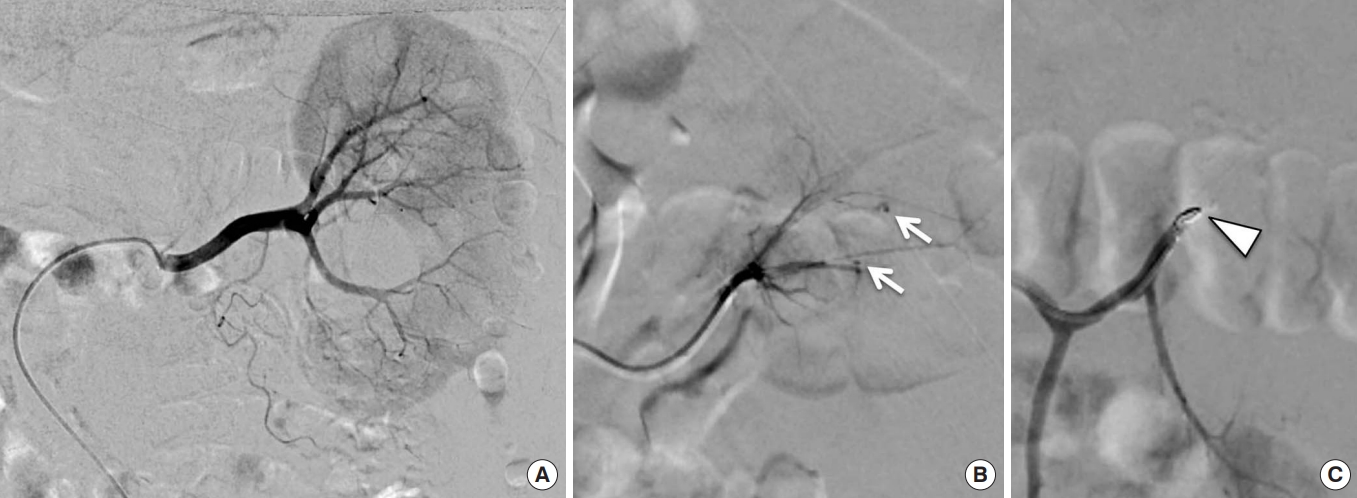
(A) Selective left renal artery angiography and (B) superselective intraparenchymal angiography demonstrating the presence of two focal microspots of extravasation due to bleeding (arrows) at the middle third of the kidney. (C) Postembolization superselective intraparenchymal left renal angiography control showing a metallic artefact of the deployed coil (arrowhead) and occlusion of the two pathological arterial branches.

(A) Left renal ultrasound control at 3 days confirming the presence of the left simple renal cyst (arrowhead) with initial reduction in size. (B) Contrast-enhanced multidetector computed tomography axial image at 1-month follow-up demonstrating significant reduction in size of the left simple renal cyst (arrowhead) to a volume of 67.8 mL. Note the metallic artefact of the deployed coil (arrow) into the embolized intraparenchymal branch of the left renal artery
Simple renal cysts are benign and usually asymptomatic, so no treatment is required. When they are symptomatic, as with haemorrhage, treatment might be necessary [1]. Only three cases of transcatheter arterial embolization of symptomatic patients with haemorrhagic renal cysts are described in the literature [2,3].
As demonstrated by our clinical case, transcatheter arterial embolization of renal intracystic active bleeding as definitive treatment (like other body regions) may have advantages over surgery of a less invasive procedure, the possibility to progress from diagnosis to treatment in the same session, and the possibility of minor loss of normal renal parenchyma [2-4]. The patient provided written informed consent for publication of the research details and clinical images.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
References
Article information Continued
Notes
Capsule Summary
What is already known
Symptomatic haemorrhagic renal cysts with macroscopic haematuria are usually treated by surgery.
What is new in the current study
We present a case of renal cyst with increased bleeding and “rising tide sign” on imaging that was treated by superselective arterial embolization with clinical resolution.
