Successful full-term delivery after out-of-hospital cardiac arrest during the second trimester of pregnancy: a case report
Article information
Abstract
Out-of-hospital cardiac arrest in pregnancy is extremely rare. In this case report, a 43-year-old female patient at 24.0 weeks of gestation collapsed outside her home after cardiac arrest. The paramedics performed cardiopulmonary resuscitation with defibrillation for ventricular fibrillation. Spontaneous circulation was achieved after 19 minutes. The fetus was stable during postarrest care. The patient exhibited high blood pressure with seizure-like symptoms for 2 days afterwards, which resolved with magnesium sulfate. She gradually recovered and returned to her daily activities while on treatment with beta blockers for cardiomyopathy and premature ventricular contractions until delivery. At 37.2 weeks of gestation, she underwent elective Cesarean section under spinal anesthesia. The baby weighed 2.55 kg and did not present with any complications. Here, we report a case of successful full-term delivery in a patient who underwent cardiopulmonary resuscitation for sudden cardiac arrest during the second trimester of pregnancy.
INTRODUCTION
Cardiopulmonary arrest in pregnancy is rare; it occurs in 1:12,000 admissions for delivery [1]. The incidence of out-of-hospital cardiac arrest (OHCA) in pregnant women is lower than that of in-hospital cardiac arrest [2]. Only a few OHCA cases have been reported worldwide. The maternal survival rate after OHCA is approximately 12% to 16% [2-10]. Despite its rarity, the low survival rates of this condition indicate that appropriate guidelines and training are required for such events. However, there is no scientific evidence for managing cardiac arrest during pregnancy. Because clinicians must simultaneously manage the patient and the fetus, cardiac arrest management in pregnancy is challenging. Here, we report the first case of successful full-term delivery in a Korean patient who received appropriate initial cardiopulmonary resuscitation for OHCA and who achieved spontaneous circulation at 24.0 weeks of gestation.
CASE REPORT
An unidentified pregnant woman was witnessed to collapse because of cardiac arrest. The paramedics arrived at the site 6 minutes after the event occurred. They activated the basic life support system and found that the initial heart rhythm was ventricular fibrillation. They shocked her heart five times with an automated external defibrillator. Another 6 minutes later, the specialist paramedics applied the adult-advanced life support system. They administered 1 mg of intravenous epinephrine and 500 mL of normal saline during the resuscitation. Following this, a supraglottic airway device (i-gel; Intersurgical Ltd., Wokingham, UK) was inserted. Eventually, return of spontaneous circulation (ROSC) was achieved 19 minutes after the start of active basic life support (Fig. 1).
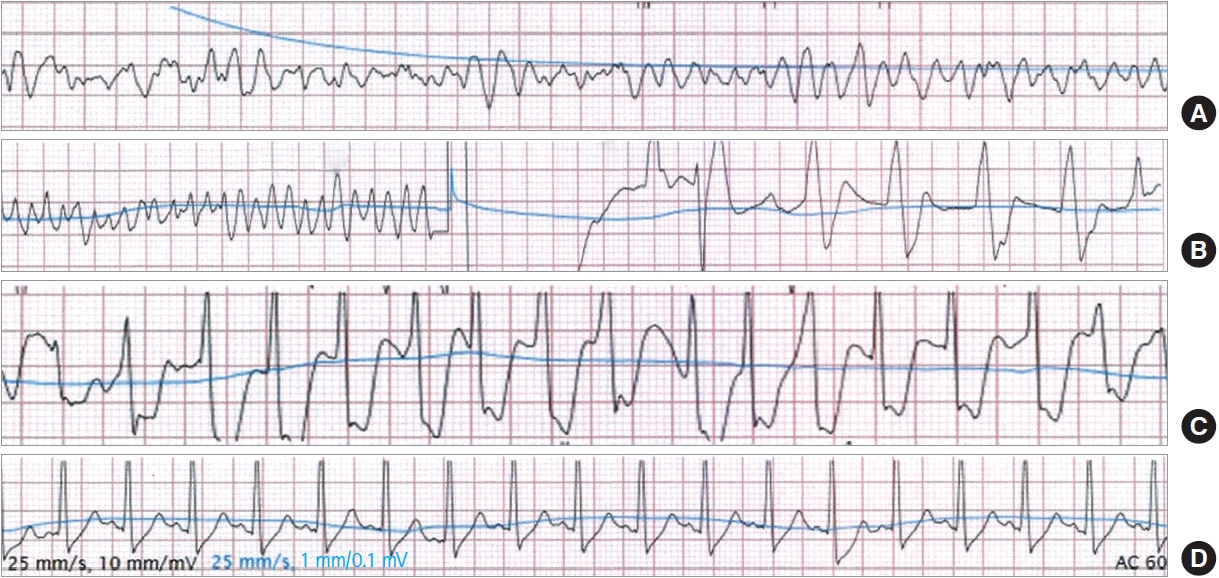
Serial electrocardiogram monitoring. (A) Ventricular fibrillation was the initial heart rhythm. (B) The heart rhythm after the fifth defibrillation. (C) Return of spontaneous circulation 19 minutes after initiating active cardiopulmonary resuscitation. (D) A normal sinus rhythm in the patient upon hospital arrival.
The paramedics and the patient arrived at the hospital 34 minutes after the cardiac arrest. Based on the initial neurological examination, the patient was comatose (Glasgow Coma Scale score, 5). Her blood pressure was 176/100 mmHg, and her peripheral oxygen saturation was 100% on manual ventilation. The 12-lead electrocardiogram showed sinus tachycardia (131 beats per minute [bpm]). Because she was already unconscious, she was ventilated with an endotracheal tube and only 100 mg of suxamethonium and no additional sedatives. The patient’s cardiac ejection fraction (EF) was only 37%. After a few minutes, her heartbeat became irregular with premature ventricular complexes (PVCs) and tachycardia (150–160 bpm), for which 150 mg of amiodarone was administered. The patient also experienced short but repeated tonic seizure-like symptoms. To control the tonic seizure and rigidity, 2 to 5 mg of lorazepam and midazolam were alternatively administered, to totals of 8 mg lorazepam and 10 mg midazolam. A computed tomography scan of the head, chest, and abdomen was performed in the emergency room, and the results were normal.
During the emergency rescue, no information was available regarding the patient’s duration of gestation. Her gravid uterus was at the level of the umbilicus. Hence, we assumed that she was approximately 20 weeks pregnant. The fetal cardiac activity was 160 to 170 bpm, and the fetal abdominal circumference on transabdominal ultrasonography was 194 mm, which is normal for 24 weeks of gestation. The fetus had no abnormalities in the umbilical and middle cerebral arteries on Doppler ultrasonography. Moreover, there was no heartbeat deceleration during postarrest care in the emergency room. Therefore, we focused on the patient, and an emergency Cesarean section was not considered.
The patient was 43 years old and was at 24.0 weeks of gestation (gravida 5, para 1). After admission to the intensive care unit, she received sedative agents until absence of irritability. Furthermore, magnesium sulfate was administered for 6 days because eclampsia was suspected due to her symptoms, such as seizure-like motion, high blood pressure, and a urinary protein level of 3+. Her vital signs gradually stabilized, with the fetus remaining in a stable condition. All laboratory results were normal. Electroencephalography was performed to assess consciousness, and the findings revealed no abnormalities in background brain activity. The patient’s level of consciousness improved without any additional seizure-like symptoms. Therefore, she didn’t receive therapeutic hypothermia.
However, the echocardiographic evaluation showed an EF of 34.6% and dilated cardiomyopathy. Thus, the patient was treated daily with 100 mg metoprolol, a beta blocker for cardiomyopathy and PVCs until delivery. There were no other complications, and the patient and her baby were followed up at an outpatient clinic. At 37.2 weeks of gestation, she underwent elective Cesarean section under spinal anesthesia. The patient gave birth to a male infant weighing 2.55 kg (15th percentile) with an Apgar score of 7 after 1 minute and 8 after 5 minutes. After delivery, the baby underwent brain sonography and echocardiography, and the results showed no abnormalities. Subsequently, the patient and her son were discharged without any complications.
The Institutional Review Board at of Jeju National University Hospital approved this study (No. 2022-03-016). Informed consent for publication of the research details and clinical images was obtained from the patient.
DISCUSSION
In previous studies of pregnant women with OHCA, the maternal and neonatal survival rates were 28.6% (8 of 28) and 25.0% (7 of 28), respectively. Of these 28 total patients, four experienced sudden cardiac arrest during the second trimester of pregnancy. However, only one had a successful full-term delivery without maternal or neonatal complications after OHCA during the second trimester of pregnancy [6].
Although the incidence of OHCA in pregnancy is low, several methods can be used to increase patient survival rates during these emergencies. Early ROSC after cardiac arrest indicates a good prognosis for both the mother and the fetus. To decrease the time required to achieve ROSC in pregnant patients, high-quality resuscitation with aortocaval blood circulation against a gravid uterus and urgent transport are important [1,2,11]. The 2020 American Heart Association guidelines recommend that paramedics apply a new cardiac arrest algorithm and prioritize treating pregnant women [11]. In particular, a gravid uterus in a woman at more than 20 weeks of gestation compresses the aorta and vena cava and reduces cardiac output. Hence, manual left lateral uterine displacement (LUD) is required to facilitate aortocaval blood circulation [1]. If ROSC is not achieved, perimortem Cesarean delivery (PMCD) is required immediately after hospital arrival [1,11,12]. PMCD within 5 minutes is an effective method to improve blood flow [1,11].
There are no data supporting the usefulness of manual LUD after ROSC. However, a previous study showed that the full left lateral decubitus position can reduce aortocaval compression [13]. Thus, the patient was placed in the left lateral decubitus position without manual LUD. Moreover, there are no guidelines for whether PMCD should be implemented after ROSC. Five-minute PMCD is not satisfactory in 93% of cases, even for in-hospital cardiac arrest [12]. Nonetheless, this procedure was not performed in any maternal OHCA cases [9]. The average duration of transport from the scene to the hospital was 94 minutes based on French data [2], and it was more than 30 minutes according to Canada data [9]. In this case, although the patient reached the hospital 28 minutes after the paramedics arrived, she survived. Maurin et al. [2] reported that a pregnant woman at 31 weeks of gestation with prehospital ROSC did not survive despite PMCD. Therefore, obstetricians should consider PMCD depending on the pregnant woman’s gestational status and the circumstances to which she is exposed during the emergency.
A multidisciplinary team should perform postarrest care after resuscitation if the patient has achieved ROSC without PMCD. Although therapeutic hypothermia can be considered after cardiac arrest (even in pregnant women), its effects on the fetus are unknown [1,11,13]. Two studies have reported successful use of therapeutic hypothermia [4,6]. In one case, fetal demise occurred during hypothermia [5]. In the current case, the patient experienced seizure-like motions on the 1st day of hospitalization. Thus, the use of therapeutic hypothermia was considered. However, after administration of magnesium sulfate to control the symptoms of eclampsia, the patient did not present with any symptoms and had normal electroencephalography findings. The patient made a successful recovery without the need for therapeutic hypothermia.
It is also important to consider the cause of cardiac arrest during pregnancy. An accurate diagnosis via proper examination can help facilitate lifesaving therapies [1]. In this case, further echocardiography and electrocardiogram showed that the patient’s EF was 30% to 35%, and her left ventricle was dilated. Moreover, her heartbeat was irregular with PVCs. A cardiologist made the diagnosis of peripartum cardiomyopathy with underlying dilated cardiomyopathy. Patients with this condition have the highest mortality rate (2%–24%) [14]. Patients with an EF <40% must undergo appropriate counseling and receive joint multidisciplinary care and appropriate medications [14]. Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers are contraindicated during pregnancy. The use of beta blockers in pregnant patients with an EF <40% have been shown to improve symptoms and survival [14,15]. Therefore, in this case, the patient was treated with metoprolol, a beta blocker used for cardiomyopathy and arrhythmia.
Early delivery can be considered if there are signs of nonreassuring fetal status [1]. Nevertheless, there are no guidelines regarding the preferred type of delivery in a full-term pregnant woman with stable status after cardiac arrest. The EF of our patient did not improve to 40%. Thus, we performed elective Cesarean section at 37.2 weeks gestation under spinal anesthesia according to the 2018 European Society of Cardiology guidelines [14].
In conclusion, if OHCA occurs in pregnant women, maternal and fetal outcomes show remarkable improvement with early recognition of arrest and rapid initiation of maternal resuscitation. A multidisciplinary team can facilitate a safe full-term delivery if appropriate treatment is provided with consideration of the conditions of the pregnant women and their fetuses.
Notes
CONFLICT OF INTEREST
The authors have no potential conflict of interest to disclose.
FUNDING
None.
Acknowledgements
The authors thank all paramedics for their heroic efforts to save lives.
References
Article information Continued
Notes
Capsule Summary
What is already known
Cardiac arrest in pregnant women is extremely rare. There are some available treatments, such as a perimortem Cesarean delivery or hypothermia therapy. However, stability is not guaranteed. Hence, recommendations cannot be equally applied to all pregnant women.
What is new in the current study
After appropriate initial resuscitation, a pregnant woman who experienced out-of-hospital cardiac arrest during the second trimester achieved spontaneous circulation. The patient was able to maintain her pregnancy while receiving suitable treatment. To our knowledge, this is the first report of a case in Korea in which the patient successfully delivered her baby at full term after out-of-hospital cardiac arrest.
