Survival benefit of direct transport to trauma centers among patients with unintentional injuries in Korea: a propensity score-matched analysis
Article information
Abstract
Objective
This study investigated the characteristics and survival rates of patients with unintentional severe trauma who visited a regional trauma center (TC) or a non-TC.
Methods
This retrospective, national, population-based, observational, case-control study included patients with abnormal Revised Trauma Score from January 2018 to December 2018. We divided hospitals into two types, TC and non-TC, and compared several variables, including in-hospital mortality. Propensity score matching was used to reduce the effect of confounding variables that influence survival outcome variables.
Results
Of the 25,743 patients, 5,796 visited a TC and 19,947 visited a non-TC. Compared to patients treated at non-TCs, patients treated at TCs were more likely to have a higher Injury Severity Score (TC, 11.5; non-TC, 7.4; P<0.001), higher rate of surgery or transcatheter arterial embolization (TC, 39.2%; non-TC, 17.6%; P<0.001), and higher admission rate (TC, 64.7%; non-TC, 36.9%; P<0.001) through the emergency department. After propensity score matching, 2,800 patients from both groups were analyzed. Patients in the TC had a higher survival rate than patients that were not treated in the TC (TC, 83.0%; non-TC, 78.6%; P=0.003).
Conclusion
This study using Korean emergency medical services data showed that initial transport to trauma centers was associated with mortality reduction. Further research is required because of limitations with use of single-year data and retrospective design.
INTRODUCTION
Trauma is a leading cause of death in people under the age of 49 years, with more than 5 million patients dying each year from trauma [1]. Since trauma occurs more frequently in younger populations, it could negatively impact the labor market nationally [2]. Treatment for patients with severe trauma is resource-intensive; thus, patients who need higher levels of care should be transported to an appropriate trauma center (TC) [3].
Since the late 1960s, emergency medical services (EMS) have developed rapidly. The evolution of modern cardiopulmonary resuscitation and the recognition of motor vehicle crashes as one of the greatest public health problems in the United States have been well chronicled [4]. Most developed countries have established and implemented trauma delivery systems such as classification and transport of trauma patients from the prehospital stage. Consequently, the Korean government established a plan to design a national trauma system in 2012, with the main goal of establishing 17 TCs nationwide [5]. As of 2020, 17 TCs have been designated nationwide, and 15 have been officially opened and dedicated to treating patients with severe trauma. These centers receive annual financial support for dedicated personnel, along with government support for facilities and equipment [6].
The regional TC is a facility that allows a trauma team (traumatology, neurosurgery, and emergency medicine) to respond to patients within 10 minutes to provide integrated and essential treatment including resuscitation and initial treatment [7]. In the Korean emergency medical system, there are guidelines for transporting major trauma patients to TCs. But EMS has claimed that many of the major trauma patients who met the criteria for a TC were not transported appropriately due to unsupported conditions. At the non-TC, severe trauma patients who need a systematic response from the trauma team may receive inappropriately delayed initial treatment, such as emergency surgery or angiographic embolization [8].
In this study, we aimed to analyze the prognosis and related factors of patients with severe trauma by comparing the number of patients transported directly to regional TCs with those transported directly to non-TCs.
METHODS
Ethical statements
This study was approved by the Institutional Review Board of Kyung Hee University Hospital at Gangdong (No. KHNMC 2021-07-048). This study conforms to the ethical guidelines of the 1975 Declaration of Helsinki. The requriement for informed consent was waived due to the retrospective nature of the study.
Study design and setting
This was a nationwide retrospective cohort study of Korean patients with severe injuries and multiple casualties transported by the Korean EMS. The study period was from January 2018 to December 2018.
The study included severe trauma patients with abnormal Revised Trauma Score (RTS) at the scene of the injury and who were transported to emergency departments (EDs) during the study period in Korea. Patients whose RTS was unknown, including those who experienced out-of-hospital cardiac arrest and were dead on arrival, were excluded. Patients with normal RTS, such as those who were transported due to nontraumatic causes or who had mild injuries and those with missing records, were not considered trauma patients and were excluded from the study. Intentional injuries, such as self-injury and suicide, were also excluded from the study. The Korean EMS is a single-tier, government-provided system, headed by the National Fire Agency, which provides basic life support ambulance services throughout the 17 provincial headquarters. All EMS providers can apply advanced airway support and can provide intravenous fluid to a patient following the EMS cardiopulmonary resuscitation protocol [9].
Clinical factors included the RTS and Injury Severity Score (ISS) as indicators to determine the degree of damage to individual patients. The RTS is a convenient tool for trauma triage and initial severity estimation. This physiological scoring system consists of the Glasgow Coma Scale, systolic blood pressure, and respiratory rate [10]. The ISS is the most widely used score to assess the extent of damage in patients with severe trauma in the hospital [11]. The ISS is based on the Abbreviated Injury Scale, which describes the severity of injury to different body parts (head, face, chest, abdomen, limb, and external), and the scores of the three most seriously damaged body parts are squared and summed to produce the ISS score [12]. The proportion of patients with ISS 16 or higher was used to compare injury severity.
Data collection and process
Patient data consisted of prehospital data acquired from the National Fire Agency and data confirmed through medical record surveys. Nonidentification measures were taken based on the Personal Information Protection Act and Statistics Act. According to the national statistics law, the Korea Disease Control and Prevention Agency dispatched trained medical record investigators to hospitals and collected hospital data by medical record review. An investigator in charge of community-based trauma status visited the medical institution confirmed by the 119 paramedic transport information, checked whether it was a patient with severe injuries and multiple casualties, collected necessary information, and conducted an interfacility transfer investigation to confirm additional treatment and results. Trauma data consisted of sociodemographic information, injury information, progress during treatment, and results after hospitalization [13].
In this study, patients were assigned to either a TC or a non-TC. The outcome variable was in-hospital mortality, as reported in the nationwide trauma registry. The exposure variable of interest was whether a patient with ISS≥16 received definitive trauma care, such as surgery or embolization at a designated TC or non-TC. In addition to the primary exposure variable (TC vs. non-TC), we considered multiple confounders, predictors, and effect modifiers for all multivariable outcome models: sex, injury mechanism (traffic-related, falls, stabbing or penetrating wound, burn, other), insurance, and interfacility transfer status [14].
Statistical analysis
Continuous variables are presented as means and standard deviations or medians and interquartile ranges. Categorical variables are presented as numbers and percentages. Patients were divided into two groups (TC and non-TC). To compare the two groups, Student t-test was used for continuous variables, and the chi-square test was used for categorical variables. Patients who underwent surgery or transcatheter arterial embolization (TAE) were selected and analyzed according to type of treatment center. Subgroup analysis of patients with ISS ≥16 among patients who underwent surgery and TAE was also performed.
To reduce the effects of confounding variables that influence outcome variables, when analyzing patients with severe trauma who underwent surgery or TAE, propensity score matching (PSM) was used to collect data in both groups. Trauma center patients were matched 1:1 with non-TC patients according to propensity score, using exact matching. To assess bias reduction in the PSM method, absolute standardized differences were calculated, with a value >20% indicating a significant imbalance in the baseline covariate.
All statistical analyses were performed using R ver. 3.6.2 (R Foundation for Statistical Computing), and P-values were based on a two-sided significance level of 0.05.
RESULTS
Characteristics of study subjects
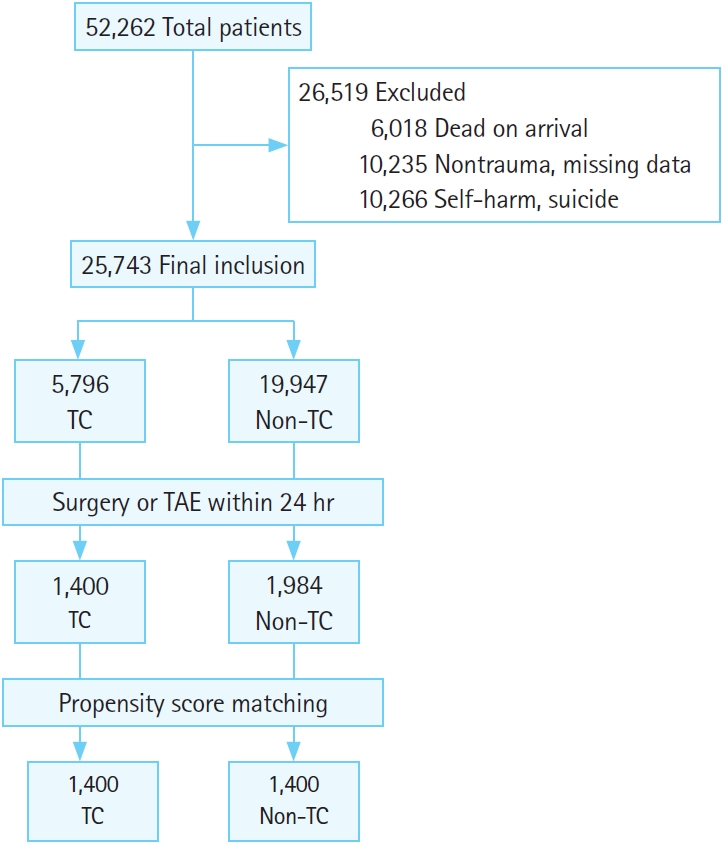
Of the 52,262 patients transported to EDs in Korea during the study period, 25,743 were considered suitable for the study and were included in the analysis. Patients who experienced cardiac arrest before ED visit (n=6,018), visited the ED with nontraumatic causes and inadequate data for analysis (n=10,235), and suffered an intentional injury (n=10,266) were excluded. Among the included patients, 5,796 visited TCs and 19,947 visited non-TCs. Patient matching was achieved in 10.9% (2,800 of 25,743) of all patients, 24.2% (1,400 of 5,796) of those who visited TCs, and 7.0% (1,400 of 19,947) of those who visited non-TCs (Fig. 1).
Main results
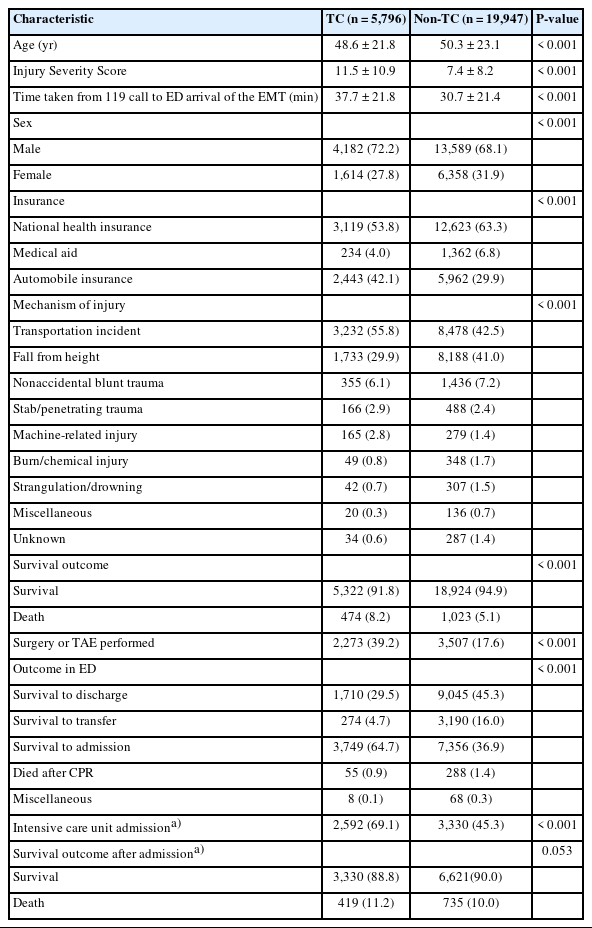
We compared patient characteristics, including demographic variables, ISS, and injury mechanism, between the two groups. Compared with patients treated at non-TCs, patients treated at TCs were younger, predominantly male, had a disproportionately higher number of traffic-related injuries, and were more seriously injured, according to ISS. Notably, patients treated at non-TCs showed a shorter time from the 119 call to ED arrival by the emergency medical technician. Patients’ medical outcomes were summarized by level of definitive trauma care. Compared to patients treated at non-TCs, patients treated at TCs were more likely to have a higher rate of surgery or TAE and higher admission rate through the ED. However, there was no significant difference in the survival rate of inpatients in the two groups (Table 1).
In previous results, patients treated at TCs had a higher hospitalization rate, resulting in a relatively lower interfacility transfer rate than patients treated at non-TCs. Subsequently, transferred patients from TCs showed a lower intensive care unit (ICU) admission rate and a higher survival rate than patients from the nonTCs (Table 2). It was not known whether the transferred patients attended a TC or non-TC as the follow-up hospital.
We also compared non-TC and TC groups for patients who underwent surgery or TAE for their severe trauma treatment. Compared to patients treated at non-TCs, patients treated at TCs were notably younger and had higher ISS. Time taken for surgery or TAE at TCs was shorter (Table 3).

Subgroup comparison of severe trauma patients who underwent surgery or TAE within 24 hours (n=3,384)
This study used PSM to control for age, sex, and ISS in patients with severe trauma who underwent surgery or TAE. From each group, 1,400 patients were selected. The proportion of patients with ISS ≥16 was matched between the two groups. Lower in-hospital mortality was observed in the TC group than in the non-TC group (Table 4).
DISCUSSION
In a past clinical analysis of patients with severe trauma, shortening the time from trauma to appropriate treatment was associated with reduced mortality [15]. Patients with severe trauma may not be able to quickly receive high-quality care when they are transported to non-TCs. Repeated interfacility transfer of patients and imaging may affect prognosis [16,17]. However, there is currently no clear distinction between non-TCs and TCs when transporting patients with severe trauma in Korea [10]. In this context, this study aimed to understand the effect of direct transport to the TC. Because the data were collected nationwide, this study should have a lower risk of sampling bias than previous studies.
In this study, patients transported directly to TCs were younger, and the proportion of male patients was higher than those transported to non-TCs. Trauma severity, identified as ISS, was higher and transportation to the emergency room took longer in TCs. Additionally, the proportion of traffic accidents tended to be higher in TCs. Regarding the characteristics of injuries related to traffic accidents, some studies have reported increased risk for young men and their greater inclination to engage in risky behaviors, such as speeding and consumption of alcohol or drugs, compared with women [18–21]. The overall mortality and neurological outcomes for men are not better, despite their younger age [22]. All these factors may affect treatment outcomes at TCs. Consistent with previous studies, there is a selection bias in which more severely impaired patients have priority transport to TCs. To the extent that selection bias is present, the TC population will be systematically different from the non-TC population [23]. This can complicate comparisons of survival rates between TCs and non-TCs and should be controlled in statistical analyses.
Patient treatment results were evaluated at the level of definitive treatment, such as surgery or arterial embolization [24,25]. Compared with patients treated in non-TCs, patients treated in TCs had more than twice the rate of surgical or arterial embolization, and the resulting hospitalization rate tended to be higher. Additionally, the ICU hospitalization rate for patients in non-TCs was higher than that for patients in TCs due to their high severity. However, there was no difference in survival rate between the two groups, possibly due to a combination of factors. Patients who were interfacility transferred from a non-TC had low survival-to-transfer rates, whereas all patients who were transferred from a TC had lower rates of ICU hospitalization and mortality. It can be interpreted that, among patients with severe trauma who needed immediate intensive care, fewer had to be transferred to a higher hospital level. In this respect, the effects of primary treatment in trauma centers can also be compared.
Because there was no difference in mortality between the two groups in the initial analysis, subgroup analysis was performed on patients who underwent surgery or TAE. A recent study by Ball et al. [26] suggested that the reduction in mortality in patients with vascular impairment was associated with an actual decrease in time spent within the ED and surgeon commitment to rapid transport to the operating room. In our study, although the time required for surgery or TAE in TCs was shorter, the difference in survival rates was not statistically significant.
We performed resampling using PSM for a controlled comparison of factors affecting the survival rate. After postmatching analysis, the difference of ISS score of TC patients and non-TC patients was not statistically significant. Through PSM, no statistical difference in the ratio of patients with severe trauma was observed. After adjusting for related factors, the survival rate of the TC patient group was significantly higher.
This study and its analysis process have several limitations. First, it was not known whether the transferred patients went to a TC or non-TC as the follow-up hospital. In this study, it was possible to compare the results of interfacility transferred patients according to the type of hospital of initial arrival. It is necessary to collect and supplement patient records from the follow-up hospital in future studies.
Second, we were unable to capture deaths that occurred shortly after discharge as a result of trauma injuries, even though Mullins et al. [27] demonstrated that many trauma deaths occur within 30 days of hospital discharge. Ideally, these deaths should have been included in the analysis [28].
Third, the data used in this study were from a single year and offer the advantage of representing Korea’s EMS at the national level. If data are accumulated over several years and follow-up studies are conducted, more meaningful and constructive results can be derived in the future.
Finally, even in the PSM analysis, we were unable to exclude numerous unknown confounding factors that may have affected the difference in TC status from outcomes after patient transportation. Other limitations are common to epidemiological studies, including ascertainment bias and lack of data integrity.
In this study, using data from the Korean EMS, we demonstrated that the direct transport of patients with severe trauma to TCs might lead to better survival benefits than transport to non-TCs.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization: DJL, SHK, HZC; Data curation: DJL, SHK, HZC; Formal analysis: DJL, JK, HZC; Investigation: DJL, HZC; Methodology: DJL, SHK, HZC; Project administration: DJL, MCK, HZC; Resources: DJL, HZC; Software: DJL, JK, HZC; Supervision: MCK, HZC; Validation: DJL, JK, HZC; Visualization: DJL, JK, HZC; Writing–original draft: DJL; Writing–review & editing: DJL, SHK, MCK, HZC. All authors read and approved the final manuscript.
Acknowledgements
The authors would like to thank the Korea Disease Control and Prevention Agency (KDCA) for their cooperation in establishing the database. The data supporting the findings of this study are available from KDCA (http://kdca.go.kr) upon application request.
References
Article information Continued
Notes
Capsule Summary
What is already known
Treatment of patients with severe trauma is resource-intensive and requires many human resources; thus, patients who need a higher level of care must be transported to an appropriate trauma center (TC). In the Korean emergency medical system, there is currently no distinction between regional TCs and nonTCs regarding transporting and treating major trauma patients.
What is new in the current study
The direct transport of patients with severe trauma to TCs was associated with better survival benefits than non-TCs. The time for surgery or transcatheter arterial embolization at TCs was shorter.