Frequency of posttrauma complications during hospital admission and their association with Injury Severity Score
Article information
Abstract
Objective
Multiple trauma is associated with a remarkable risk of in-hospital complications, which harm healthcare services and patients. This study aimed to assess the incidence of posttrauma complications, their relationship with poor outcomes, and the effect of the Injury Severity Score (ISS) on their occurrence.
Methods
This retrospective cohort study was conducted at a pair of trauma centers, between January 2020 and December 2022. All hospitalized adult patients with multiple trauma were included in this study. Multivariable logistic regression was used to identify factors related to posttrauma complications.
Results
Among 727 multiple trauma patients, 90 (12.4%) developed in-hospital complications. The most frequent complications were pneumonia (4.8%), atelectasis (3.7%), and superficial surgical site infection (2.5%). According to multivariable logistic regression, ISS, the length of stay in the intensive care unit (ICU), the length of stay in the hospital, and mortality were significantly associated with complications. The complication rate increased by 17% with every single-unit increase in ISS (adjusted odds ratio [OR], 1.17; 95% confidence interval [CI], 1.00–1.38). Per every 1-day increase in the ICU or hospital stay, the complication rate increased by 65% (adjusted OR, 1.65; 95% CI, 1.00–2.73) and 20% (adjusted OR, 1.20; 95% CI, 1.03–1.41), respectively. Posttrauma complications were also significantly more common in patients with mortality (adjusted OR, 163.30; 95% CI, 3.04–8,779.32). In multiple trauma patients with a higher ISS, the frequency, severity, and number of complications were significantly increased.
Conclusion
In-hospital complications in multiple trauma patients are frequent and associated with poor outcomes and mortality. ISS is an important factor associated with posttrauma complications.
INTRODUCTION
Trauma is a serious public health issue ranked as the first cause of disability-adjusted life-years for people of productive age, according to the latest Global Burden of Disease report [1]. Trauma is recognized as blunt or penetrating injuries, mostly from motor vehicle collisions, falls, interpersonal violence, or self-harm. Trauma accounts for approximately one out of three emergency department visits in the United States annually [2]. Undoubtedly, these numbers are likely higher in developing countries due to the lack of infrastructure [3].
During the last decades, the improvement in diagnostic strategies and patient management has led to a remarkable decline in the mortality rate of patients with trauma injuries. Numerous studies have affirmed the improvement in trauma survival rates among patients from different regions [4–7]. However, it is important to note that keeping trauma patients with major injuries alive makes them susceptible to trauma-related complications [8]. Patients with trauma can experience a wide range of in-hospital complications, including infections, coagulopathy, thromboembolic events, and organ failure.
Trauma-related complications bear undesirable consequences for patients and trauma centers. Patients with posttrauma complications have an increased risk of death [9–11]. Moreover, studies have concluded that these individuals experience a more extended hospital stay length and a higher cost of care [12,13]. Such complications can also negatively affect patients’ quality of life and lifelong functionality [14]. Therefore, more attention should be given to reduce the numbers of these unwanted complications.
The majority of trauma-related complications can be prevented. Applying suitable antimicrobial prophylaxis, adhering to venous thromboembolism-prevention guidelines, and practicing early rehabilitation could be practical and effective steps to decrease posttrauma complications. Nevertheless, it should be noted that complications are not similarly distributed among trauma patients. Based on the existing evidence, there is no way to accurately predict when, how, or what kind of complications a patient with trauma might experience. Conducting more research on the epidemiology of posttrauma complications using records from different trauma centers could help to identify patients at a higher risk.
Therefore, the aims of the present study were the following: (1) assess the overall incidence and types of complications in hospitalized adult patients with multiple trauma; (2) describe the clinical features and outcome of the patients with posttrauma complications; and (3) examine the effect of injury severity on the occurrence of complications in multiple trauma patients.
METHODS
Ethics statement
The study protocol was reviewed and approved by the Institutional Review Board of Shahid Beheshti University of Medical Sciences (No. IR.SBMU.MSP.REC.1400.814). The requirement for informed consent from individual patients was waived due to the retrospective nature of the study. The study adheres to the principles outlined in the Declaration of Helsinki.
Study setting and design
This was a retrospective cohort study evaluating the occurrence of complications in patients with multiple trauma. The study was conducted at a pair of trauma centers (Shohadaye Tajrish Hospital, Tehran, Iran; Valiasr Hospital, Tehran, Iran). Multiple trauma patients were identified from the electronic databases of the centers between January 2020 and December 2022, using the International Classification of Diseases, 10th Revision (ICD-10) code T07. Patients were required to have injuries in two or more areas of the body to be classified as multiple trauma patients [15]. The confidentiality of data was maintained throughout the study, and the results were reported anonymously.
Participants
All patients with multiple trauma aged ≥18 years and hospitalized in the centers mentioned above were included in this study. Patients were excluded if they met the following criteria: (1) admitted as a secondary admission from another center; (2) discharged or transported from the study center before completing the assessment and management; (3) admitted multiple times for one episode of trauma; or (4) died in the emergency department due to the impact of fatal trauma.
Data collection
We collected data from patients’ records, including general demographics (sex, age, comorbidities, and medication history), trauma characteristics (type, mechanism, and Injury Severity Score [ISS]), arrival vital signs (blood pressure, heart rate, respiratory rate, temperature, oxygen saturation, and Glasgow Coma Scale Score [GCS]), management approaches (hemorrhagic shock and transfusion of blood products), hospital admission information (department of admission, mechanical ventilation, length of hospital stay, and intensive care unit [ICU] admission and length of stay), in-hospital complications, and mortality.
To weigh the comorbid conditions and underlying disease, we used the Charlson Comorbidity Index score [16]. The ISS score was measured as the sum of squares of the highest Abbreviated Injury Scale from three different body regions [17]. Posttrauma complications were defined as medical and surgical complications related to trauma that occurred during hospital admission, including infections, thromboembolic events, and circulation disturbance, and were confirmed by two experts and written in the medical records. We classified the complications that were potentially life-threatening or resulted in permanent disability, including cerebral vascular accident, acute coronary syndrome, arrhythmia, abdominal compartment syndrome, pulmonary embolism, acute respiratory distress syndrome, gastrointestinal bleeding, peritonitis, compartment syndrome, deep vein thrombosis, deep surgical site infection, sepsis, and multiorgan failure, as major complications. A general practitioner was responsible for data collection under the direct supervision of an emergency physician specialist.
Statistical analysis
Assuming the frequency of 5% for posttrauma complications based on a previous report [18], for a desired precision of 2%, a minimum sample size of 450 was necessary to estimate complications in our study centers. Therefore, we decided to collect data on patients with multiple trauma during 2 subsequent years. Results of the descriptive analysis are presented as counts with percentages (qualitative variables) or median with interquartile range values (quantitative variables) according to the non-normal distribution of the data. The chi-squared test was used for proportions and the MannWhitney U-test was used for continuous variables to compare the demographic and clinical characteristics between the cohort of patients with and without complications, respectively. Any variable with a significant univariable test was inserted into the multivariable logistic regression to find factors related to posttrauma complications. Adjusted odds ratios (ORs) for these factors were presented with 95% confidence intervals (CIs). To further evaluate the association between ISS and the occurrence of posttrauma complications, we used ISS as a categorical variable divided as ≤8 (minor), 9 to 15 (moderate), 16 to 24 (severe), and ≥25 (very severe) [19]. The impact of ISS on frequency, severity, and the number of complications was assessed using the chi-squared test. All hypothesis tests performed were two-sided. P<0.05 was considered to be statistically significant. All statistical analyses were conducted using IBM SPSS ver. 24 (IBM Corp).
RESULTS
Characteristics of the study population
Of the 1,336 patients recorded as having multiple trauma in the database between January 2020 and December 2022, there were 890 hospitalized patients (the remaining 446 were managed as outpatients). Among them, 727 patients met the study inclusion criteria (Fig. 1). Patients were admitted to different units of the hospitals, including the emergency department (62.5%), surgery department (19.9%), neurosurgery department (4.5%), and orthopedic surgery department (3.9%), or directly to the ICU (4.4%).
The median age of patients was 33 years (interquartile range [IQR], 24–45 years), and 79.1% of patients were male. Among the total study population, 15.7% had at least one comorbid condition, and the median Charlson Comorbidity Index score of these patients was 2 (IQR, 0–3). The trauma type in most patients was blunt (97.2%). The most common causes of trauma were motorcycle accident (28.5%), car accident (27.2%), fall (18.3%), pedestrian accident (17.9%), and assault (6.2%). The median ISS score of all patients was 3 (IQR, 0–9). The overall mortality rate of the whole cohort was 5.8%.
Incidence of complications
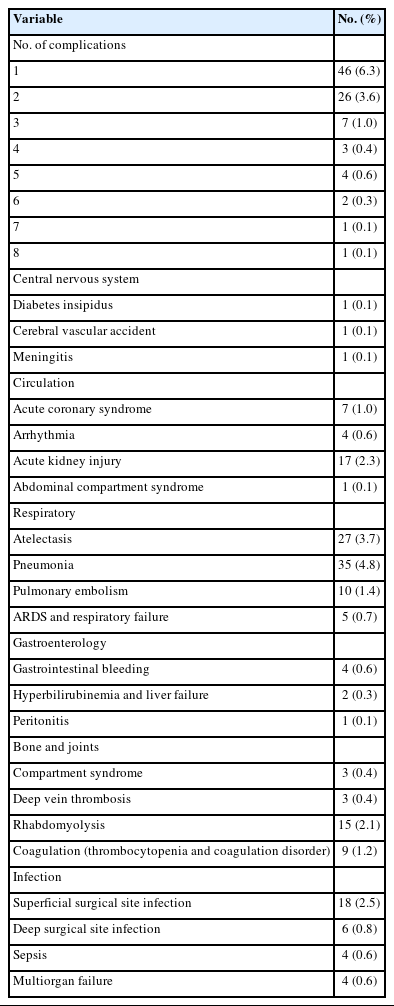
A total of 90 patients (12.4%) experienced in-hospital complications during the course of this study, including 35 (38.9%) who suffered from major complications. Most of the patients developed only one complication. The most frequent complications were pneumonia (4.8%), atelectasis (3.7%), and superficial surgical site infection (2.5%). The mortality rate in multiple trauma patients with complications was 33.3%, and a rise in complication numbers (OR, 34.54; 95% CI, 15.77–75.67) and major complications (OR, 4.63; 95% CI, 3.21–6.69) increased the mortality rate. The characteristics of complications observed in this study are demonstrated in Table 1.
The comparison between patients with and without complications revealed a significant difference in age between the two groups (39.5 [IQR, 28.7–51.0] years vs. 32.0 [IQR, 24.0–45.0] years, P=0.005). Patients with complications had higher Charlson Comorbidity Index scores (0 [IQR, 0–1] vs. 0 [IQR, 0–0], P=0.006). The ISS was greater in patients with complications than in those without them (22 [IQR, 14–34] vs. 1 [IQR, 0–6], P<0.001). The presence of complications in multiple trauma patients was associated with ICU admission (54.4% vs. 6.3%, P<0.001), a longer length of ICU stay (3 days [IQR, 2–8 days] vs. 2 days [IQR, 1–3 days], P<0.001) and longer length of hospital stay (5 days [IQR, 2–13 days] vs. 1 day [IQR, 1–1 days], P<0.001), and mortality (33.3% vs. 1.9%, P<0.001). Features of the multiple trauma patients with and without complication are presented in greater detail in Table 2.

Comparing the demographic and clinical characteristics of patients with and without in-hospital complications
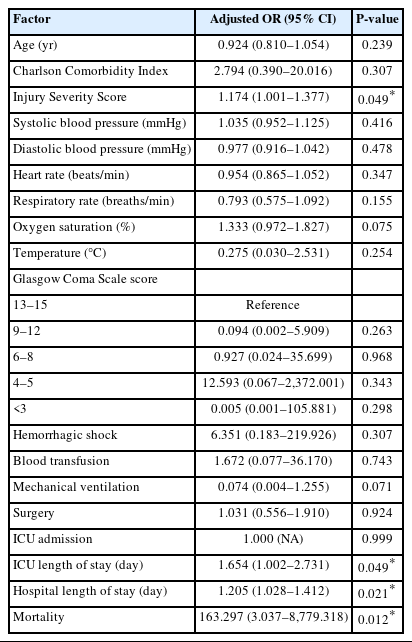
A multivariable logistic regression analysis was performed to identify factors associated with complications in patients with multiple trauma (Table 3). Accordingly, ISS, ICU length of stay, hospital length of stay, and mortality were significantly associated with complications. Per every 1-point increase in ISS, the complication rate in multiple trauma patients increased by 17%. Also, with every 1-day increase in the ICU and hospital stay lengths, the complication rate increased by 65% and 20%, respectively. Posttrauma complications were also 163 times more common in patients with mortality.
Effects of injury severity
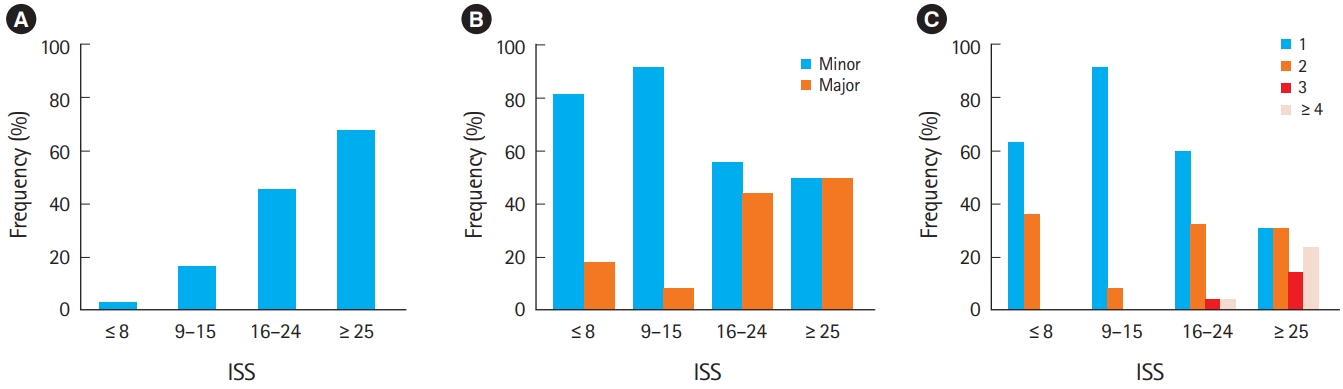
We further investigated the effects of ISS on in-hospital complications in multiple trauma patients. Accordingly, the frequency of complications was significantly increased in higher ISS categories (P<0.001); more specifically, the occurrence rate was 2.0% when ≤8, 16.4% when 9 to 15, 45.5% when 16 to 24, and 67.7% when ≥25 (Fig. 2A). With a higher ISS, there were more major complications that occurred in a statistically significant fashion (P=0.027). In order from the lowest to the highest ISS category, the occurrence rates of major complications were 18.2%, 8.3%, 44.0%, and 50.0%, respectively (Fig. 2B). In addition, the number of complications significantly increased in association with a higher ISS (P=0.005). In the group where ISS≥25, 38.1% of patients with complications experienced four or more complications, while this rate was just 4.0% when ISS was 16 to 24 and 0% when ISS≤8 or 9 to 15 (Fig. 2C).
DISCUSSION
In-hospital complications in patients with multiple trauma are common and associated with a significant burden on both patients and trauma centers. Tracing these complications is crucial to establish the best practices for their reduction. The present study explored the characteristics and outcomes of patients with multiple trauma to add to the growing knowledge of posttrauma complications. We found that almost 10% of hospitalized adult patients with multiple trauma experienced at least one complication; in-hospital complications were also associated with poor outcomes, and ISS was identified as an important factor associated with complications.
The 12.4% posttrauma complication rate among multiple trauma patients in the current study is consistent with previous reports [20,21]. According to other studies, this incidence rate could rise to as high as 30% in ICU-admitted patients [11,12]. Pulmonary-related complications were the most frequent posttrauma complications, while thromboembolic events were associated with the highest mortality rate [11,20,22]. Notably, patients with more complications and/or with major complications were at greater risk for death.
According to our data, in-hospital complications in multiple trauma patients are associated with increased lengths of hospital stay and ICU stay, which is consistent with previous reports [10,12,23]. These observations could be attributed to the fact that salvage of severely injured patients with multiple trauma necessitates more extended hospitalization and ICU care, increasing complications and vice versa. We also observed a strong association between mortality and posttrauma complications; in other words, multiple trauma patients with complications are at increased risk of death. Although the cost of care was not evaluated in the current study, the increase in both hospital length of stay and mortality undoubtedly enhances resource utilization. A previous study focused on the cost associated with traumatic injury showed that patients with complications are likely to have three to five times higher costs than those without complications [13].
Our findings also showed that ISS was significantly associated with in-hospital complications in multiple trauma patients. In particular, we observed that the rate of complications increased by 17% for every 1-point increase in ISS. Accordingly, in higher ISS category groups, more patients experienced complications and also more frequently suffered from major and multiple complications. A severe injury following a traumatic event can have an extreme impact on physiological mechanisms, including the immunological, endocrinological, and acute stress responses. Moreover, these patients usually undergo multiple transfusions, numerous invasive procedures, surgeries, and extended hospital care, making them vulnerable to developing complications. To date, several studies have indicated the direct effect of ISS on the occurrence of infection [24], thromboembolic events [25], and acute kidney injury [26] following the trauma. Therefore, calculating ISS as an independent predictor of posttrauma complications is crucial for the management of patients with trauma, and scores should be recorded in patients’ charts.
In addition to complications, another important metric is the mortality rate of complicated multiple trauma patients. Failure to rescue patients with complications is an evolving factor that identifies the hospital’s quality of care of patients with trauma [27]. The mortality rate of multiple trauma patients with complications in the present study was measured as 33.3%, which is higher than rates in similar previous reports [20,21]. Several factors influence mortality following complications; some are related to clinicians and care providers, while others are related to patients. A study from Japan showed that trauma patients in high-performing hospitals had lower rates of complications and failure to rescue than those in low-performing hospitals [20]. Another study indicated that clinician-attributable errors in diagnosing and managing trauma patients with complications are a major contributor to mortality [21]. Age, preexisting comorbidities, and insurance status are also patient-related factors identified to significantly affect the mortality of trauma patients with complications [28–31].
The nature of multiple trauma injuries demands a multidisciplinary approach and real-time decision-making. Improving the quality of care and minimizing errors can successfully reduce the rate of in-hospital complications and related deaths in patients with multiple trauma. A recent study from the United States assessed eight million patients with trauma and noted a significant drop in posttrauma complications over a decade [18]. Therefore, adhering to resuscitation and prophylaxis protocols, besides identifying patients at greater risk, could be a key component for reducing complications in multiple trauma patients.
There were some limitations in the current study. First, this study had a retrospective design, and the recorded complications’ correctness and completeness depended on the responsible clinicians. There might also be some patients with multiple trauma treated during the study period that were not included. Second, we could not confirm the causal relationship between events due to uncertainty about the complications’ onset date. Third, this study did not collect data on prophylaxis or treatment approaches. To reduce the posttrauma complications in multiple trauma patients, future studies could investigate interventions that might improve trauma centers’ quality of care.
Multiple trauma injuries are associated with a wide list of in-hospital complications. ISS was detected as a major factor associated with in-hospital complications, implying its importance when managing patients with trauma. Multiple trauma patients with more severe injuries should receive high-quality care and preventive services to avoid unwanted complications.
Notes
ETHICS STATEMENT
The study protocol was reviewed and approved by the Institutional Review Board of Shahid Beheshti University of Medical Sciences (No. IR.SBMU.MSP.REC.1400.814). The requirement for informed consent from individual patients was waived due to the retrospective nature of the study. The study adheres to the principles outlined in the Declaration of Helsinki.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization: MY, SS; Data curation: SD, SS; Formal analysis: SD, MY, SS; Investigation: MY, HM, SS; Methodology: MY, MFR, MF, SS; Project administration: MY, SS; Resources: MFR, MF; Software: MY; Supervision: SS; Validation: SS; Visualization: SS; Writing–original draft: SD, SS; Writing–review & editing: all authors. All authors read and approved the final manuscript.
References
Article information Continued
Notes
Capsule Summary
What is already known
Patients with multiple trauma are susceptible to experiencing in-hospital complications, including infections, coagulopathy, and thromboembolic events, which are mostly preventable.
What is new in the current study
We found that posttrauma complications were common and related to poor outcomes; moreover, the Injury Severity Score was detected as an important factor associated with complications.