A survey-based study on the protocols for therapeutic hypothermia in cardiac arrest patients in Korea: focusing on the differences between level 1 and 2 centers
Article information
Abstract
Objective
We aimed to summarize the therapeutic hypothermia (TH) protocols used in emergency departments (EDs) in Korea and to investigate the differences between level 1 and 2 centers.
Methods
The chief residents from 56 EDs were given a structured survey containing questions on the indications for TH, methods for TH induction, maintaining, and finalizing TH treatments. The participants were divided into 2 groups based on their work place (level 1 vs. level 2 centers).
Results
We received 36 responses to the survey. The majority of the participants (94.4%) reported that they routinely used TH. An average of 5.9 (standard deviation, 3.4) and 3.3 (standard deviation, 2.9) TH procedures were performed monthly in level 1 and 2 centers, respectively (P=0.01). The majority of level 1 and 2 centers (80.0% and 73.1%, respectively) had written TH protocols. Rectal (50.0%) and esophageal probes (38.9%) were most commonly used to monitor the patients’ body temperatures. Midazolam (80.6%) and remifentanyl (47.2%) were the most commonly used sedatives. For TH induction, external cooling devices (77.8%) and cold saline infusion (66.1%) were predominant. Between level 1 and 2 centers, only the number of TH, the usage of remifentanyl, and application of external cooling device showed significant differences (P<0.05).
Conclusion
Our study summarizes the TH protocols used in 36 EDs. The majority of study participants performed TH using a written protocol. We observed small number of differences in TH induction and maintenance methods between level 1 and 2 centers.
INTRODUCTION
Therapeutic hypothermia (TH) is one of the most potent treatments to increase the survival and improve the neurologic outcomes of survivors of cardiac arrest [1]. Although the application of TH has been advised by guidelines of the American Heart Association and the European Resuscitation Council, details such as the indication for TH, duration, methods, or target temperature have not been established yet [1-4]. Several tests such as brain MRI and electroencephalogram (EEG) to predict patient survival and neurologic outcomes have been suggested. However, the overall value of these tests is still controversial in their efficiency and effectiveness [5-8].
Investigations about the current status of TH utilization have gained interest in many countries. Several studies have investigated the criteria of, the indications for, and the methods used for TH [9-12]. In Korea, a report published by the Korean Hypothermia Network Registry recently described the clinical characteristics of TH patients of 24 participating hospitals [13].
However, previous studies did not focus on TH protocols. An indepth investigation of TH protocols and a comparison between well- and less-established hospitals is required to implement an effective TH protocol. The objective of this study was to provide an overview of the currently utilized TH protocols in Korea and to investigate the differences between level 1 and 2 centers.
METHODS
Study setting
In Korea, approximately 20.9% of patients experiencing emergency medical service (EMS)-assessed out-of-hospital cardiac arrests (OHCAs) are not provided cardiopulmonary resuscitation by EMS providers, and only 1.0% gain prehospital return of spontaneous circulation.
All emergency departments (EDs) in Korea are designated level 1, 2, or 3 by government authorities. Currently, 20 level 1, 122 level 2, and about 275 level 3 EDs serve as destination hospitals for OHCA victims [14,15]. Among these, 56 EDs have an emergency medicine residency program.
Study population
The chief residents of 56 EDs were asked to fill out surveys during a national emergency medicine meeting. The purpose of the study was explained to the residents, and their written informed consent was received.
Survey questions
The survey questions were structured based on previous studies from the USA, Canada, and European countries [10-12]. They were grouped into 5 clusters and included items on: 1) the presence of a written TH protocol as well as the indications and contraindications for TH; 2) the methods used for TH induction; 3) the methods used for maintaining TH; 4) those used for finalizing the TH process; and 5) the prognostication of patients undergoing TH (Appendix 1).
Statistical analysis
The study participants were divided into 2 groups based on their work place—those working at level 1 and those at level 2 centers. Level 2 emergency centers have a full capacity of clinical services from major surgery to minor care such as plastic surgery. Level 1 centers have same the clinical capability as level 2 centers, and in addition, they provide training and education for the region, including disaster preparedness. Though quality of care exist among different regions, the common essentials of the emergency medical system such as EMS and insurance are shared nationwide and each level of centers [16-18].
We used descriptive statistics to depict the study participants’ responses to survey. Continuous variables are presented as means and standard deviations. Statistical analysis was performed with STATA ver. 13 (StataCorp., College Station, TX, USA).
RESULTS
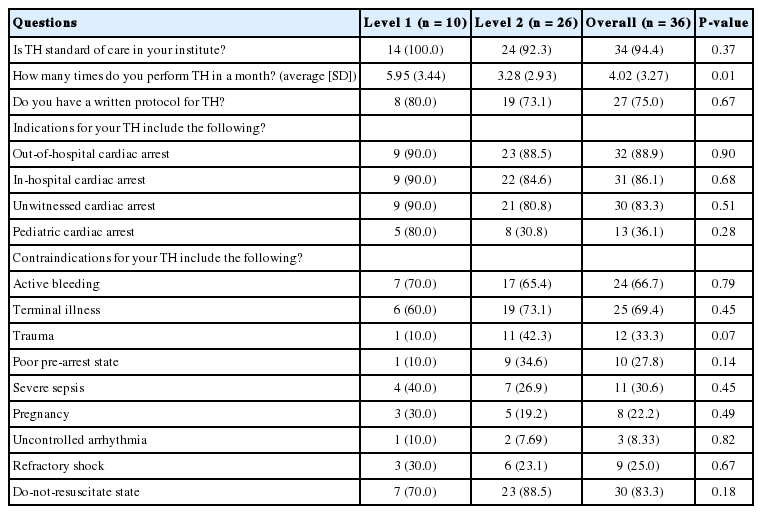
A total of 36 (57.1%) responses were received from 63 subjects (27.8% from residents of level 1 centers). Overall, 34 chief residents (94.4%) reported that they routinely applied TH in cardiac arrest patients, and that an average of 4.0 (standard deviation, 3.3) TH procedures were performed per month. Whereas the majority of OHCA and in-hospital cardiac arrest patients underwent TH (88.9%), only the minority of pediatric cardiac arrests patients did (36.1%). The majority of the study participants answered that active bleeding, terminal illness, and do-not-resuscitate orders were seen as contraindications for TH (Table 1). Regarding the existence of a written protocol, no statistically significant difference between level 1 and level 2 centers was observed (80.0% vs. 76.1%, P=0.67). The geographical distribution of EDs is shown in Fig. 1.

The locations of the emergency departments that were enrolled or excluded from this study are depicted. The existence (or absence) of a written therapeutic hypothermia (TH) protocol is also demonstrated.
Table 2 shows the processes used for TH induction. The majority of the study participants reported using esophageal and rectal probes to monitor the patients’ body temperatures. The most common agents for sedation were midazolam (80.6%) and remifentanyl (47.2%). About 66.7% of the residents answered that they used neuromuscular blockers as part of routine care, while only 13.9% reported using preventive anticonvulsants. The average TH target temperature was reported to be 33.4°C (standard deviation, 0.80). External cooling with a mechanical device was the most common method (77.8%) to achieve this, whereas the infusion of a cold fluid was the second most common method (66.1%).
The most common target value for mean arterial pressure was ≥65 mmHg (88.9%). All study participants answered that they used a TH duration of 24 hours. The rewarming rate varied among the subjects, and some reported not controlling the rewarming rate (11.1%) (Table 3).
Table 4 summarizes the measures used for predicting the patients’ prognoses. Among several methods that were being used, the most common included EEG (63.9%), brain computed tomography (58.3%), and neuron-specific enolase (36.1%). We only observed a difference in the use of S-100 between level 1 and 2 centers (50.0% vs. 7.7% in level 1 and 2 centers, respectively; P=0.01).
DISCUSSION
In this survey-based study, we reviewed the TH protocols used in a variety of EDs in Korea. Although only a small number of sites could be recruited, we were able to reveal significant data on the TH protocols utilized in these EDs.
The rate of centers who reported using written TH protocols was 75.0%; this is higher than the rate reported in a previous Canadian study (58.9%) [8]. The proportion of EDs performing TH was 94.4%, which is also higher than that reported in studies in Italy (55.1%) and Germany (86%) [9,10]. However, the location of treatment (intensive care unit vs. ED), and the interval since the publication of the guideline might have contributed to these differences, making a direct comparison difficult. However, supporting data could not be demonstrated throughout this study.
The indications and contraindications for TH were similar albeit not identical between level 1 and level 2 centers. This might be due to the implementation of the American Heart Association and European Resuscitation Council guidelines in academic hospitals [1].
The methods used for monitoring the patients’ body temperatures are different from those used in other countries. For example, only 16.7% of the residents in this study reported using the bladder to measure body temperature, whereas 56.1% of respondents reported doing so in a previous study [11]. TH induction was similar to previous studies, in that external cooling devices were used most commonly.
In our study, EEG was the most commonly used method to evaluate the patients’ neurologic prognoses (63.9%), followed by brain computed tomography (58.3%), and brain magnetic resonance imaging (58.3%). This is not consistent with a previous study that showed that neurologic examination (92.0%) and median nerve somatosensory evoked potentials (94.0%) were primarily used for prognostication [19].
We only observed a few statistically significant differences between the two groups. A higher numbers of TH procedures were performed and more measures of cooling methods were used in level 1 than level 2 centers. Among these methods, the rates of using bladder irrigation and a mechanical external cooling device showed statistically significant differences.
This study has several limitations. First, the number of study participants was smaller than intended. In the national perspective, the included participants only accounted for less than 30% of overall EDs. We observed wide differences in several factors between the two groups; however, these differences were not statistically significant. A future investigation with better coverage will likely yield significant outcomes.
Second, the survey questions might have been subjective to the investigators. Even though comprehensive data were collected from previous studies and the questions were based on these data, we might have not covered other elements of TH treatment in our survey [8-10].
Third, this study did not include data on institution and community characteristics. The socioeconomic status of the neighborhood, urbanization level, and the case volume of cardiac arrest are known institutional and regional characteristics that might explain differences among study subjects [17,20,21].
Last, we only studied TH protocols used in hospitals. There could be gaps between these protocols and actual clinical practice due to practical reasons. Therefore, studies conducted in patients level should be referred in one needs to understand present practice [13]. Although this study compared the TH protocols used in level 1 vs. level 2 centers, we did not have data on the quality of care, which limits implication to real practice.
In conclusion, we described the TH protocols used in 36 EDs. The majority of the chief residents working in these hospitals performed TH using written protocols. We observed a small number of differences in the TH induction methods between level 1 and the level 2 centers.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This work was supported by a research grant from Samsung Medical Center (OTX0001731).
References
Appendices
Article information Continued
Notes
Capsule Summary
What is already known
Therapeutic hypothermia contributes to the outcome of cardiac arrest patients. There are emergency departments using therapeutic hypothermia.
What is new in the current study
We have investigated protocols of 36 academic emergency departments throughout the country. There were differences among study sites, though very small difference between level 1 and level 2 centers.