Change in guardians’ preference for computed tomography after explanation by emergency physicians in pediatric head injury
Article information
Abstract
Objective
Head injury in children is a common problem presenting to emergency departments, and cranial computed tomography scanning is the diagnostic standard for these patients. Several decision rules are used to determine whether computed tomography scans should be used; however, the use of computed tomography scans is often influenced by guardians’ preference toward the scans. The objective of this study was to identify changes in guardian preference for minor head injuries after receiving an explanation based on the institutional clinical practice guideline.
Methods
A survey was conducted between July 2010 and June 2012. Patients younger than 16 years with a Glasgow Coma Scale score of 15 after a head injury and their guardians were included. Pre- and post-explanation questionnaires were given to guardians to assess their preference for computed tomography scans and factors related to the degree of preference. Treating physicians explained the risks and benefits of cranial computed tomography scanning using the institutional clinical practice guideline. Guardian preference for a computed tomography scan was examined using a 100-mm visual analog scale.
Results
In total, 208 patients and their guardians were included in this survey. Guardian preference for computed tomography scans was significantly reduced after explanation (46.7 vs. 17.4, P<0.01). Pre-explanation preference and the strength of the physician recommendation to get a computed tomography were the most important factors affecting pre- and post-explanation changes in preferences.
Conclusion
Explanation of the risks and benefits of cranial computed tomography scans using the institutional clinical practice guideline may significantly reduce guardian preference for computed tomography scans.
INTRODUCTION
Head injury in children is a common problem presenting to emergency departments (EDs) [1,2]. Cranial computed tomography (CT) scans are the diagnostic standard for identifying the presence of intracranial injury in the acute phase [3]. However, the radiation risk of CT scans should be considered, particularly in children [4]. Decisions about CT scans are challenging for minor head injuries, because it is difficult to balance radiation risk and identification of intracranial injuries [1,2]. Several decision rules have been developed to help with decision-making for CT scans, but these were based on limited populations [3,5-7]. In 2009, the Pediatric Emergency Care Applied Research Network (PECARN) rule was derived and validated for children with minor head injuries using Glasgow Coma Scale (GCS) scores of 14 to 15 in a large population of children [8]. This rule was developed to identify clinically important traumatic brain injuries (CiTBI) and reduce excessive CT use [8]. We developed and applied an institutional clinical practice guideline based on published decision rules to reduce CT use [5-8]. During application of this practice guideline, CT scan use was also influenced by guardian preference. We hypothesized that an explanation based on the practice guideline could change guardian preference. Therefore, the objective of this study was to identify changes in guardian preferences after an explanation of the risks and benefits of cranial CT scans using a clinical practice guideline.
METHODS
Study design and setting
This study was a survey including pre- and post-explanation questionnaires (Appendices 1-3). The methodology was approved by the hospital institutional review board. The setting was the ED of a tertiary hospital with an annual census of 26,000 pediatric patients (younger than 16 years). Patients were treated by emergency resident physicians supervised by board-certified attending physicians.
Our institutional clinical practice guideline for pediatric minor head injury was developed by an institutional joint committee of EP and pediatric neurologists [6-8]. The committee reviewed several published decision rules including the PECARN rule [6-8], and modified these rules for our institution. The clinical practice guideline could be applied to children with blunt minor head injuries with GCS greater than 13. Cranial CT scans were used to identify any patients with a CiTBI, defined as death from head injury, neurosurgery, intubation for more than 24 hours, or hospital admission for at least two nights associated with head injuries on CT scans [8].
Survey study protocol
The clinical practice guideline was implemented beginning in July 2010. During 6 months prior to the survey, we educated emergency physicians (EP) about the new guideline and posted it for them to consult at any time. The survey was conducted between July 2010 and June 2012 from 10 am to 10 pm. The study period was limited due to the working time of clinical research nurses. Inclusion criteria were age younger than 16 years, GCS of 15, and treatment in our ED after head injuries. Patients with preexisting neurologic diseases or coagulation diseases, those with non-blunt head injuries or with injuries to other body parts, and those who were transported after head imaging studies at other hospitals were excluded from the survey. When an eligible patient arrived at the ED, the triage nurse gave the guardian the preliminary questionnaire form after describing the study. After the guardian completed the questionnaire, a board-certified EP examined the patient and explained the risks and benefits of CT scans, and symptoms and signs that required a CT scan, based on the clinical practice guideline. After hearing the explanation, the guardian filled out the post-explanation questionnaire. Informed consent of guardians was also obtained. The preliminary questionnaire asked about patient characteristics such as sex, age, presence of siblings, experience, numbers of previous CT scans, injury time, mechanism of injury, and symptoms related to the injury. The symptoms related to the injury included amnesia, loss of consciousness, seizure, irritability, headache, dizziness, vomiting, lethargy, and abnormal behavior. We also collected data about the guardian, including sex, age, relationship to the patient, education level, severity of the injury as perceived, and guardian preference toward a CT scan. It was not possible to assess whether patients younger than 3 years had amnesia, headache, or dizziness. The post-explanation questionnaire asked about previous knowledge about the risk of CT scans, how they learned about the risk, the degree to which the physician recommended CT, and guardian preference toward a CT scan. The severity of the injury as perceived by guardians, the degree to which the physician recommended CT, and guardian preference toward a CT scan were assessed in the pre- and post-explanation questionnaires using a 100-mm visual analog scale. A value of “0” indicated that the guardian did not want the use of CT scans.
Ninety days after discharge, a follow-up telephone call was made to identify symptoms and management in other hospitals due to head injuries [8]. We assessed changes in guardian preference between pre- and post-explanation questionnaires (pre-and post-explanation preference) and factors related to changes in preferences.
Outcomes
The primary outcomes were changes in guardian preferences after receiving an explanation according to the new clinical practice guideline. The secondary outcomes were the related factors affecting changes in guardian preferences.
Data analysis
Statistical analysis was performed using the IBM SPSS Statistics ver. 19.0 (Armonk, NY, IBM Corp., USA). In the analysis of the survey study, pre- and post-explanation guardian preference was compared using the paired t-test. Factors affecting these changes were identified using univariate linear regression, and factors with P-values less than 0.1 were included in multivariate linear regression. Correlations between knowledge of the risk of CT scans, experience with previous CT scans, highest education level, and pre-explanation preference were identified using the χ2 test and Student’s t-test. A P-value less than 0.05 was considered statistically significant.
RESULTS
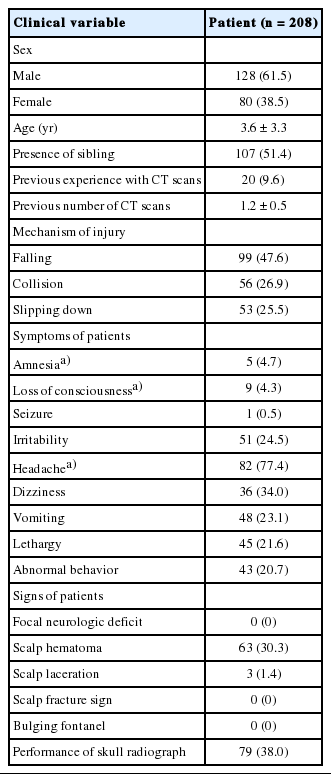
A total of 208 patients were surveyed during the study period. Male patients accounted for 61.5% (128 patients) and the mean age was 3.6 (standard deviation 3.3) years (range, 2 months to 15 years). Twenty patients (9.6%) had undergone CT scans previously. The most common cause of injury was a fall. Headache was the most common symptom, and scalp hematoma was the most common sign. No patients had a focal neurologic deficit, sign of a scalp fracture, or bulging fontanel. Although skull radiographs were performed in 78 patients, no fractures were detected (Table 1).
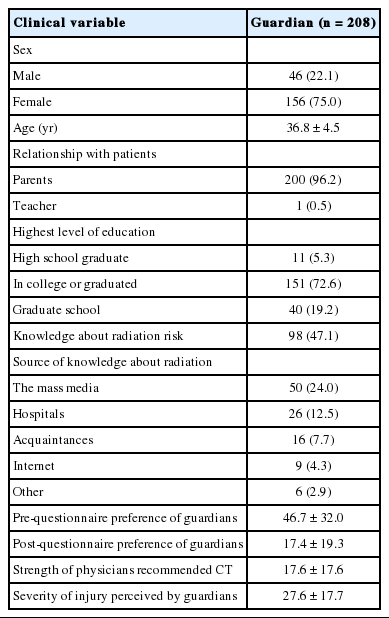
Female guardians accounted for 75.0%, and most guardians were parents. About half of the guardians knew about the radiation risk of CT scans, and half had obtained this information from the mass media (Table 2). Knowledge about the radiation risk of CT scans was not associated with previous experience with CT, highest level of education, or pre-explanation preference.
Guardian preference for CT scans was significantly reduced after receiving an explanation (46.7 vs. 17.4; P<0.01; 95% confidence interval, 25.1 to 33.5). Change in preference before and after explanation, as measured using the VAS, was significantly affected by pre-explanation preference and the strength of the physician recommended CT. However, change in preference was not significantly associated with age, presence of siblings, previous experiences with CT scans, mechanism of injury, symptoms, signs, or performance of skull radiography. Variables related to guardians, such as sex, age, relationship to the patient, highest education level, knowledge about radiation risk, source of knowledge about radiation, and severity of the injury as perceived by guardians, were not significantly related to change in preferences (Table 3). Multivariate analysis revealed that the most important factors affecting changes in preference were pre-explanation preference and the strength of the physicians recommendation for a CT (Table 4).
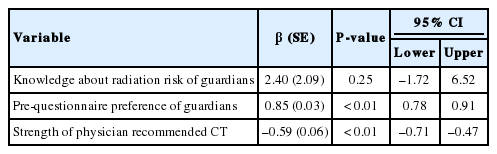
Factors affecting change in preference between pre- and post-explanation questionnaires, based on multiple linear regression analysis
At 90 days, three patients were not assessed for their symptoms. The remaining patients had recovered from their symptoms and were not being managed in other hospitals. The proportion of children who received CT scans after implementing the practice guideline was significantly reduced compared with that before the practice guideline period (7.3% vs. 13.6%, P<0.01).
DISCUSSION
This is the first study to explore changes in guardian preferences for CT scans after receiving an explanation by physicians about the risks and benefits of the clinical practice guideline. Guardian preference was significantly reduced after explanation, and this change was associated with pre-explanation preference and the strength of the physicians recommended CT.
Since the introduction of CT scans in the 1970s, their use has increased among both adults and children [4]. The use of head CT scans for minor head injuries has doubled over 10 years [2]. CT scans have a radiation risk, and children are at more risk from radiation than adults because of radiosensitive tissue and longer life duration [9]. Radiation exposure from CT scans may also increase the risk of leukemia and brain tumors in children [10]. The estimated rate of cancer in children after head CT scans is reportedly between 1 in 1,000 and 1 in 5,000 [8,11]. However, approximately half of the guardians in our survey study did not know about the radiation risk of CT scans. One previous study reported that guardian knowledge of radiation risk associated with CT scans was not affected by previous use of CT scans among their children [12]. These authors emphasized education about radiation for guardians. Our results also indicate that there is no relationship between knowledge about radiation risk and previous use of CT. This might mean that the knowledge that guardians had was abstract and unreasonable; moreover, they were unaware of when children required CT scans. Therefore, explanation of the radiation risk using the evidence-based decision rule, which clarified which cases required CT scans, could significantly reduce preferences. Two factors were significantly related to change in preference: pre-explanation preference and the strength of the physician’s recommendation for the CT.
Pre-explanation preference was not associated with knowledge about radiation risk. This suggests that greater pre-explanation preference would result in a greater change in preference, i.e., preference was significantly reduced by explanation.
Physicians have difficulty deciding whether CT scans are required for minor head injuries due to the variability in management [5,11], and should make careful decisions about the use of CT scans, considering the risks and benefits to children. EPs at our hospital have also had difficulty with this decision. An institutional clinical practice guideline may help EPs make decisions as well as help them to explain these decision to guardians more reasonably. Because the strength of the physician’s recommendation for a CT could differ (based on the degree of necessity of CT scans according to the guideline), this might affect post-explanation preference and change in preference. Among the factors identified as affecting a change in preference, the strength of the physician’s recommendation for a CT was the only adjustable factor in the ED. This might be used to reduce the number of unnecessary CT scans that are requested by guardians.
This study had several limitations. First, this was a survey study that included some, but not all, children with head injuries. Therefore, the results may reveal reduced preference among their guardians. Because we could not access the characteristics of the unenrolled patients, we identified the performance rate of CT scans after the guideline period. We assumed that the clinical practice guideline affected the use of CT scans based on the lower numbers of CT scans performed after guideline period. Second, because the survey was conducted from 10 am to 10 pm, selection bias may have been involved. The limited study time may also have had an effect in that all suspected patients were not included. However, the characteristics of guardians and patients may not have been different during other time periods. Third, as the hospital is located in a metropolitan area, the patients and guardians visiting this hospital represent a reasonably well-educated sample; thus, they may better understand the explanation of physicians. Therefore, the results may not necessarily apply to a less educated population. Fourth, this study was conducted in a single center, so the ability to generalize the results is limited.
In conclusion, explanation of the risks and benefits of cranial CT scans using the clinical practice guideline may significantly reduce guardian preference toward CT.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This study was supported by grant number 11-2010-025 from Seoul National University Bundang Hospital research fund.
References
Appendices
Article information Continued
Notes
Capsule Summary
What is already known
Cranial computed tomography scan is the diagnostic standard for intracranial injury. However, the radiation risk of computed tomography scans is problematic, particularly in children.
What is new in the current study
When physicians explain the risks and benefits of cranial computed tomography scans using the institutional clinical practice guideline, guardian preference for computed tomography scans can be reduced.