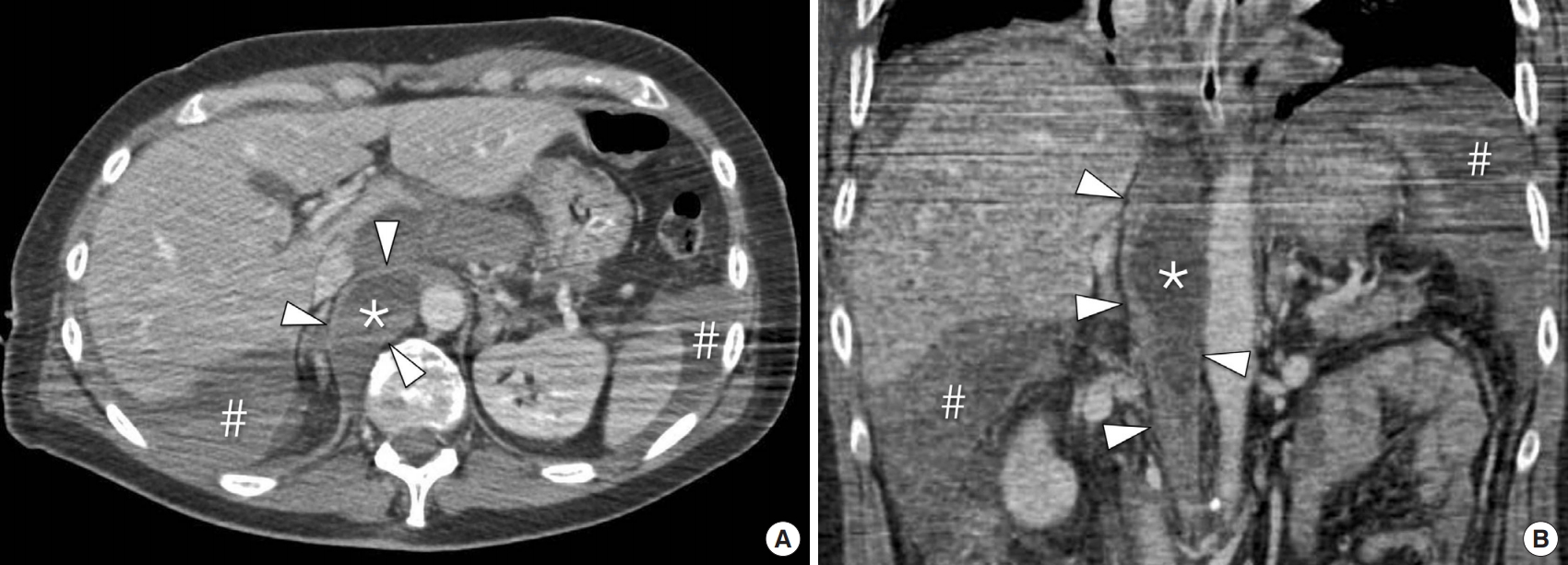
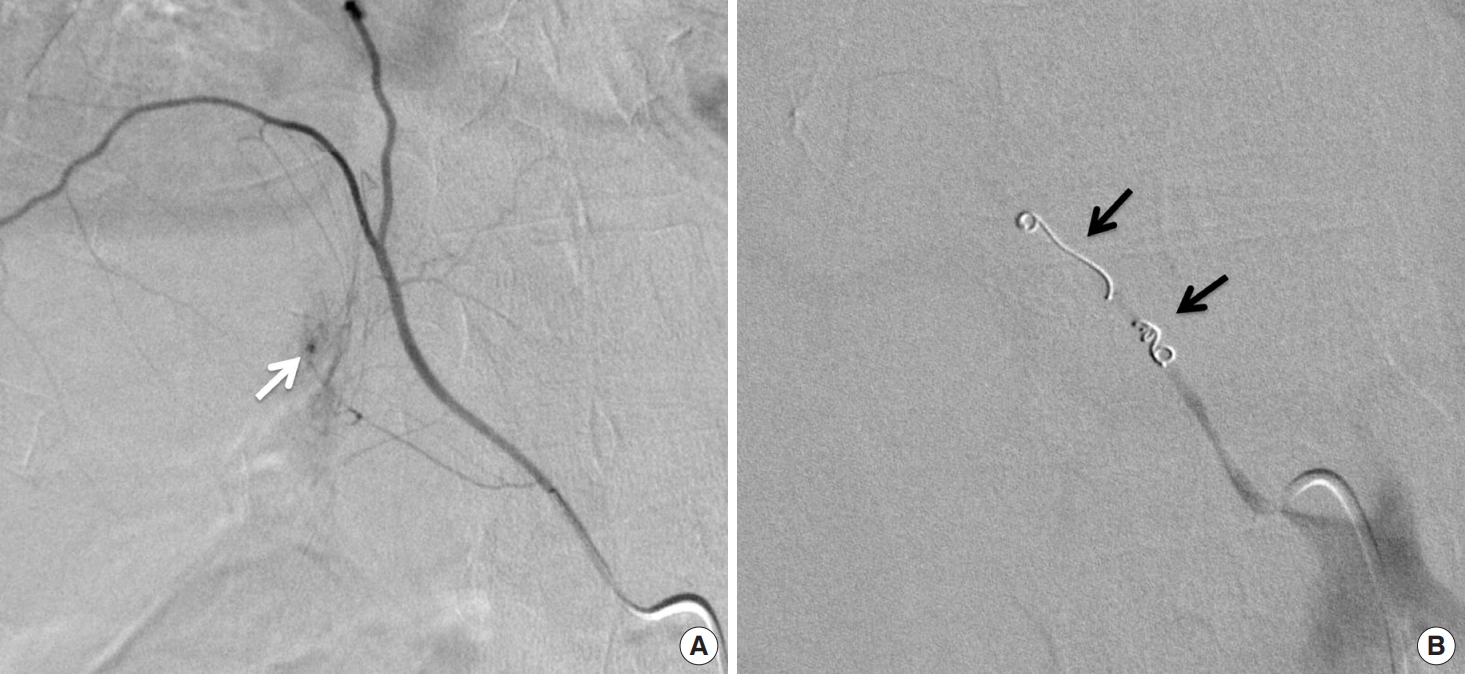
A 76-year-old hospitalized man developed acute ventricular fibrillation. The cardiology staff started cardiopulmonary resuscitation (CPR) with 30 chest compressions and two artificial ventilations, combined with automated external defibrillator use. The time to restore cardiac output was 25 minutes. Twelve hours later, he was extubated and started complaining of upper abdominal and back pain. Over this time, his hemoglobin level decreased from 13.4 to 8.7 mg/dL. Multidetector computed tomography revealed a lesion in the right crus of the diaphragm and hemoperitoneum (Fig. 1A, B). Selective lower thoracic and upper abdominal digital subtraction angiography showed active bleeding from a branch vessel of the right inferior phrenic artery (Fig. 2A). Active bleeding was stopped by coaxial superselective catheterization of the right inferior phrenic artery (Fig. 2B). The postoperative course was uneventful; he was discharged on day 10. Follow-up performed 24 months after embolization demonstrated no complications.
Diaphragmatic lesions (varying from tearing of a muscle bundle to full-strength breakage) with inferior phrenic artery bleeding due to blunt trauma is a rare emergency event [1-3]. Diaphragmatic rupture caused by CPR is even rarer [3]. To our knowledge, this is the first case involving a diaphragmatic lesion and inferior phrenic artery rupture caused by CPR, leading to hemoperitoneum. This is a potentially life-threatening condition requiring prompt diagnosis and treatment [1,2,4]. In selected cases involving active traumatic bleeding in thoraco-abdominal organs, transcatheter embolization techniques have been successfully used as the first-line treatment [5-7]. In conclusion, the possibility of injury to abdominal organs, such as the diaphragm, must be considered while performing vigorous CPR.