INTRODUCTION
Chronic pain due to cervical radiculopathy is a common condition. Drug treatment is primarily used for treating this condition, and epidural injections are known to be effective in relieving the pain [1]. However, epidural injections may cause various unexpected complications such as epidural hematomas (EHs) [2]. If an EH leads to severe neurologic symptoms or progresses rapidly, surgical decompression may be required [3]. Additionally, Brown-Sequard syndrome (BSS) may occur due to an EH [4]. However, BSS is generally known to occur due to a penetrating spinal cord injury, and the number of non-traumatic BSS cases is significantly less [5]. In this case report, we describe a rare EH case with BSS, presented to the emergency department (ED).
CASE REPORT
A 55-year-old man presented to the ED with a gait disturbance and right-sided weakness. His risk factors for acute stroke included hypertension, smoking, and cardiovascular problems. He was taking aspirin and clopidogrel for a cardiovascular disease. On arrival at the ED, his vital signs were as follows: blood pressure, 165/95 mmHg; respiratory rate, 16 breaths/min; heart rate, 78/min; body temperature, 36.7°C; and oxygen saturation with room air, 98%. His mental status was alert without any disorientation or speech disturbance, and his Glasgow Coma Scale was 15. Neurological examination revealed normal cranial nerve functions, but motor weakness (Grade 4) was confirmed in the right arm and leg. Symptoms developed within 3 hours, and we consulted the in-hospital stroke team.
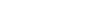
Brain computed tomography, angiography, and magnetic resonance imaging were performed sequentially to rule out vascular and brain lesions, but no specific findings were observed. After the neuroimaging, at the time of preparing thrombolytic therapy, a full neurological examination was performed. Left hemibody pain and temperature sensation below T5 was slightly impaired (90% of normal sensation). There was no hyperreflexia or clonus, and the anal sphincter tone was normal. The patient was given a C4-C5 transforaminal cervical epidural injection 30 minutes before the onset of neurological symptoms at a local pain clinic by a physician specialized in rehabilitation medicine with radiological assistance (C-arm fluoroscopy). Considering the possibility of spinal cord complications due to the epidural injection by neurological examination, no thrombolytic therapy was given. Subsequently, cervical spine magnetic resonance imaging was performed. Mild ossification of the posterior longitudinal ligament was seen at the C4-5-6 level (Fig. 1), and a hematoma at the C4- 5-6 level was also confirmed (Fig. 2). Because the right-sided weakness was not severe at the time of admission, surgical intervention was not pursued as a result of ED consultation from the neurosurgeon. The patient was admitted to the general ward and closely monitored. The patient gradually improved with conservative care. Gait was regained four days after admission, and weakness improved six days later. The sensory loss was almost completely recovered (95% of normal sensation) when he was discharged eight days after admission. The 2-month follow-up imaging study showed complete resorption of EH (Fig. 3).
DISCUSSION
Various complications may develop following a cervical epidural injection [2]. In general, the majority are self-limited minor complications such as a vasovagal reaction or procedure-related pain. However, an improper needle position can cause serious problems such as a direct spinal cord injury by the needle, epidural abscess, and EH. Embolic infarction and brain stem herniation due to an intra-arterial injection may also occur [6]. Spinal EH is treated by conservative treatment if the initial condition is good. However, if neurological symptoms progress rapidly or severe paralysis such as para or quadriparesis is present, urgent surgical decompression may be necessary [3]. Therefore, in patients with progressive complications caused by cervical lesions, treatment must be performed urgently with caution.
BSS is usually caused by penetrating spinal cord injuries such as gunshot and stab wounds. Symptoms are characterized by ipsilateral weakness and contralateral loss of pain and temperature two levels below the lesion due to lateral spinothalamic tract damage. Tumor, disc herniation, infection, autoimmune disease, and non-penetrating trauma resulting in an EH may also cause BSS. EH incidence after epidural injections is 1 in 150,000, but EH with BSS is more unusual [6,7].
There are many difficulties in ensuring early diagnosis of cervical spine lesions in patients visiting the ED. It takes a substantial amount of time to perform a full neurologic examination in a patient visiting the ED. This can be very restrictive when imaging should be performed immediately to distinguish brain lesions. Because stroke treatment is time sensitive, the ED should reduce inhospital time delays, such as those associated with door-to-imaging and door-to-needle times through a critical pathway. Due to the required tests and procedures, there is limited time to perform a full neurological examination on a patient. Nevertheless, we learned with this case that emergency physicians should be cautious to exam a patient who complains neurological symptoms.
The epidural injection is useful for treating spinal radiculopathy [8]. This case illustrates that BSS caused by an EH is possible after an epidural injection. In patients presenting with stroke symptoms and epidural injection history, it may be desirable to carry out a focused neurological examination at the beginning with the possibility of spinal cord lesions.