AbstractObjectiveWe aimed to identify the association between low serum total cholesterol levels and the risk of out-of-hospital cardiac arrest (OHCA).
MethodsThis case-control study was performed using datasets from the Cardiac Arrest Pursuit Trial with Unique Registration and Epidemiologic Surveillance (CAPTURES) project and the Korea National Health and Nutrition Examination Survey (KNHANES). Cases were defined as emergency medical service-treated adult patients who experienced OHCA with a presumed cardiac etiology from the CAPTURES project dataset. Four controls from the KNHANES dataset were matched to each case based on age, sex, and county. Multivariable conditional logistic regression analysis was conducted to evaluate the effect of total cholesterol levels on OHCA.
ResultsA total of 607 matched case-control pairs were analyzed. We classified total cholesterol levels into six categories (<148, 148-166.9, 167-189.9, 190-215.9, 216-237.9, and Ōēź238 mg/dL) according to the distribution of total cholesterol levels in the KNHANES dataset. Subjects with a total cholesterol level of 167-189.9 mg/dL (25th-49th percentile of the KNHANES dataset) were used as the reference group. In both the adjusted models and sensitivity analysis, a total cholesterol level of <148 mg/dL was significantly associated with OHCA (adjusted odds ratio [95% confidence interval], 6.53 [4.47-9.56]).
INTRODUCTIONDeath and disability due to out-of-hospital cardiac arrest (OHCA) are a significant public health concern [1,2]. The causes of OHCA can be primarily classified as cardiac and non-cardiac [3]. Many studies have focused on OHCA due to cardiac causes, including ischemic heart disease, because it accounts for a large proportion of cases of OHCA and is the main target of active resuscitation [4,5]. OHCA of cardiac origin is known to share clinical risk factors with coronary heart disease [6,7]. As lipid profile is a significant risk factor for atherosclerotic disease, studies have been conducted to evaluate its association with OHCA [8,9]. Most of these studies have focused on the adverse effects of total cholesterol or low-density lipoprotein (LDL) cholesterol [10-12]. However, only a few studies have demonstrated an association between an unfavorable lipid profile and the development of OHCA [13-15]. Cholesterol is an essential nutrient in the human body that plays a positive role in signal transduction and hormone synthesis [16]. The athero- and cardio-protective effects of high-density lipoprotein (HDL) cholesterol are well known [17]. There is evidence that reduced total cholesterol absorption efficiency is related to all-cause mortality [18]. In addition to the protective effects of high total cholesterol, a study has shown that systemic inflammation and malnutrition associated with lower total cholesterol levels influence mortality [19]. Additionally, several studies have shown that lower cholesterol levels are associated with higher mortality in various diseases and conditions [20-22]. However, few studies have focused on the association between low total cholesterol levels and the occurrence of OHCA; to investigate this, we conducted a case-control study comparing total cholesterol levels between patients who experienced OHCA and a healthy control population. We hypothesized that patients who experienced OHCA would have lower total cholesterol levels than control subjects.
METHODSStudy design and data sourcesThis case-control study was performed using datasets from the Cardiac Arrest Pursuit Trial with Unique Registration and Epidemiologic Surveillance (CAPTURES) project and the Korea National Health and Nutrition Examination Survey (KNHANES). Cases of OHCA were obtained from the CAPTURES project dataset and controls from the KNHANES dataset. Controls were randomly matched according to age (in 10-year intervals), sex, and county. Matching controls from the same county ensured that the controls were representative of the same source population as the patients. The ratio of controls to patients was 4:1; this ratio was used to increase the statistical power of the study, considering the rare nature of OHCA events [23].
The CAPTURES project database was created from a nationwide prospective multicenter cohort study designed to implement an emergency department (ED)-based OHCA surveillance system in South Korea. It was designed to identify organic problems and risk factors associated with the occurrence of OHCA based on pathophysiology. The CAPTURES project was conducted between February 2014 and January 2015 across 26 EDs. Data for the project were collected from emergency medical service (EMS)-treated patients experiencing OHCA that was suspected to be due to a cardiac etiology by emergency physicians in each ED. The project excluded patients with terminal illnesses, those in hospice care, pregnant patients, those living alone or homeless without a reliable information source, and those with a ŌĆśDo Not ResuscitateŌĆÖ card. Patients who experienced OHCA for whom resuscitation was not attempted in the ED; those transferred between hospitals; and those with a confirmed non-cardiac etiology including trauma, drowning, poisoning, burns, asphyxia, or hanging were also excluded.
The CAPTURES registry includes data on sociodemographic variables, health behaviors, medical history, physical and emotional stress, EMS and ED information presented using the Utstein template, laboratory test results, and cardiac examination results. Emergency physicians at each study site ED collected the information using structured survey papers during a face-to-face interview with patientsŌĆÖ caregivers. Study coordinators at each study site ED collected the results of laboratory tests and cardiac examinations via medical record review. The collected data were inputted and transferred to the central data server at the Korea Disease Control and Prevention Agency (KDCA). The project quality management committee (QMC), which consisted of emergency physicians, cardiologists, and statisticians, reviewed the quality of data via monthly meetings. The QMC trained study coordinators before the project began and guided surveys to ensure that precise information was collected. When the study coordinators were unable to define a coding element, they consulted the emergency physicians in the QMC for clarification.
Community-based controls were selected based on data from the KNHANES collected between 2008 and 2016. The KNHANES is an ongoing national surveillance system based on the National Health Promotion Act that has been conducted annually since 1998 to assess the health and nutritional status of Koreans. This nationally representative cross-sectional survey conducted by the KCDC collects survey sample data from approximately 10,000 individuals each year regarding socioeconomic status, health-related behaviors, quality of life, healthcare utilization, anthropometric measures, biochemical and clinical profiles for non-communicable diseases, and dietary intakes; there are three components to the survey: health interview, health examination, and nutrition survey [24].
Study settingThe Korean EMS is a multi-tier system that offers a basic to intermediate level of life support ambulance services based in fire stations run by the fire department and provided for by the government. Prehospital providers are classified into level 1 and 2 emergency medical technicians (EMTs), comparable to EMT-intermediate and EMT-basic in the United States, respectively. Even if instructed by medical practitioners, EMTs cannot legally perform blood tests in the field, except for blood sugar tests, and point-of-care testing equipment is not available in the Korean EMS. The government designates EDs as levels 1ŌĆō3 depending on the capability and capacity of the facility. In 2014, there were 18 level 1 and 122 level 2 EDs in South Korea; 9 level 1 and 17 level 2 EDs participated in the CAPTURES project. In Korea, blood samples are typically drawn within 5 minutes of arrival at the ED during the early cardiopulmonary resuscitation (CPR) phase [25]. Therefore, several blood test values such as total cholesterol measured in this study were obtained at the hospital stage. Detailed information about the EMS characteristics, OHCA protocols, and ED characteristics has been previously reported [26,27].
Study participantsCases were defined as adult (age Ōēź18 years) EMS-treated patients who had experienced OHCA with a presumed cardiac etiology and were transported to participating EDs between February 2014 and January 2015. OHCA cases with unknown total cholesterol levels, no information on the presence or absence of dyslipidemia, and those taking lipid-lowering medications were excluded. Controls were enrolled from the KNHANES database. Community controls with unknown total cholesterol levels, individuals who underwent blood sampling without fasting for more than 8 hours, those with no information on the presence or absence of dyslipidemia, and those taking lipid-lowering medications were excluded.
MeasurementsThe primary outcome was the total cholesterol level (mg/dL). We classified total cholesterol levels into six categories (<148, 148-166.9, 167-189.9, 190-215.9, 216ŌĆō237.9, and Ōēź238 mg/dL) according to the total cholesterol distribution of the KNHANES group (<10th, 10thŌĆō24th, 25thŌĆō49th, 50thŌĆō74th, 75thŌĆō89th, and Ōēź90th percentiles) [28].
The CAPTURES registry contains information on age, sex, county, date of cardiac arrest, initial electrocardiogram results (ventricular fibrillation, pulseless ventricular tachycardia, pulseless electrical activity, or asystole), response time interval, scene time interval, transport time interval, EMS defibrillation attempt, medical history (hypertension, diabetes mellitus, and/or dyslipidemia), and health behaviors including smoking (current smoker, ex-smoker, never-smoker, or unknown), alcohol use (frequent alcohol consumption [more than twice per week], occasional alcohol consumption [once or twice per week], no alcohol consumption, and unknown), number of hours spent sleeping per night (0ŌĆō6 hours, 6ŌĆō8 hours, over 8 hours, and unknown), and body mass index (BMI [kg/m2]; 10.5ŌĆō18.4, 18.5ŌĆō24.9, over 25.0, and unknown) for patients that have experienced OHCA.
When patients who experienced OHCA attended EDs, arterial blood gas analysis and routine laboratory examinations, including total cholesterol measurements, were performed as soon as possible. In addition to total cholesterol, LDL cholesterol, HDL cholesterol, and triglyceride levels were measured if possible. Blood samples were usually collected by nurses at the ED and transported to a central laboratory room where the blood was examined using commercially available laboratory machines. All laboratories involved in this study participate in qualification programs such as the College of American Pathologists survey.
The KNHANES registry contains variables related to participantsŌĆÖ demographics, medical history, health behaviors, and laboratory test components, including total cholesterol, LDL cholesterol, HDL cholesterol, triglyceride level, white blood cell count, hemoglobin level, platelet count, aspartate transaminase level, alanine aminotransferase level, blood urea nitrogen level, and creatinine level. According to standardized protocols, all health examination procedures were performed by trained medical personnel, and all equipment was calibrated periodically. Blood samples were collected from participants aged Ōēź10 years who had fasted for Ōēź8 hours. When LDL cholesterol samples were not obtained using direct assay and total cholesterol, HDL cholesterol, and triglyceride level measurements were obtained, LDL levels were calculated according to the Friedewald equation [29]. When the individualŌĆÖs triglyceride concentration was >400 mg/dL, LDL cholesterol values were treated as missing data because the LDL cholesterol value estimated from the above formula was less accurate. The laboratory data quality control program monitors laboratory performance to ensure that all analytical values meet acceptable standards of precision and accuracy [21]. The lipid panel was categorized and presented based on the KNHANES value. Total cholesterol was categorized according to the 10th, 25th, 50th, 75th, and 90th percentiles, whereas HDL cholesterol, LDL cholesterol, and triglyceride were categorized based on the 25th and 75th percentiles.
Statistical analysisDemographics of the OHCA patient and community control groups were evaluated. Categorical variables were analyzed using the chi-square test, and continuous variables were analyzed using the t-test when they followed a normal distribution. For missing data on medical history, health behaviors, and laboratory parameters, multiple imputations with multivariable proportional logistic regression models were conducted. In case of HDL cholesterol, LDL cholesterol, and triglyceride levels, multiple imputations were not performed because there were many missing values, and categories were divided according to the distribution of the KNHANES values (the 25th and 75th percentiles). For the matched case-control dataset, multivariable conditional logistic regression analysis was conducted to estimate the effect of the total cholesterol level on the risk of OHCA and to calculate the adjusted odds ratios (AORs) and 95% confidence intervals after controlling for potential confounders identified in directed acyclic graph models. Sensitivity analyses were performed in the cardiac arrest group with a shockable rhythm, the group with a relatively normal pH and potassium levels after cardiac arrest, and the relatively young group without hypertension and diabetes. Statistical significance was defined as a P-value <0.05. All statistical analyses were performed using the SAS ver. 9.4 (SAS Institute Inc., Cary, NC, USA).
RESULTSA total of 607 matched case-control pairs were included in our analysis (Fig. 1). Characteristics of the OHCA and community control groups are shown in Table 1. Patients who had experienced OHCA were more likely to have diabetes mellitus and hypertension. The OHCA group had more never-smokers and non-drinkers and had fewer people who rarely exercised, slept less than 8 hours per night, and were obese.
Laboratory findings for patients who experienced OHCA and community controls are shown in Table 2. Patients in the OHCA group were more likely to have lower hemoglobin levels and platelet counts as well as higher white blood cell counts and aspartate transaminase, alanine aminotransferase, blood urea nitrogen, and creatinine levels than the community controls. The OHCA group had lower overall levels of total cholesterol, HDL cholesterol, LDL cholesterol, and triglycerides than the control group. Fig. 2 shows the lipid panel histograms for the OHCA and control groups.
Results of the multivariable conditional logistic regression models, including the AORs (95% confidence intervals), are shown in Table 3. Subjects with a total cholesterol level of 167ŌĆō190 mg/dL (25thŌĆō49th percentile in the KNHANES dataset) were used as the reference group for analysis of the association between total cholesterol levels and each outcome. In both the unadjusted and adjusted models, total cholesterol levels of <148 mg/dL and 148ŌĆō167 mg/dL were significantly associated with the occurrence of OHCA. Potential confounders included BMI, past medical history (diabetes mellitus or hypertension), health behaviors (smoking, alcohol consumption, hours spent sleeping per night, and exercise), and laboratory data (hemoglobin and creatinine levels). BMI, past medical history, health behaviors, and laboratory data used as potential confounders also had significant AOR values (Supplementary Table 1).
Table 4 shows results of the subgroup analysis for patients who experienced OHCA and community controls. We created subgroups for patients with witnessed OHCA and a shockable rhythm, relatively normal values for serum potassium and pH, and those of a relatively young age and no history of diabetes or hypertension. Analysis of the subgroups showed similar results: the lowest total cholesterol group showed a significantly higher AOR.
DISCUSSIONIn this case-control study, individuals with low total cholesterol levels were found to have a higher risk of developing OHCA. The results of the analyses indicate that the risk of OHCA increases significantly when the total cholesterol level is less than the national populationŌĆÖs lower 10th percentile.
Recently, several studies on OHCA survivors have reported that the initial serum total cholesterol level is associated with good neurological outcomes [30-32]. One of these studies reported that HDL cholesterol was associated with outcomes following OHCA, whereas LDL cholesterol and triglycerides were not [31]. It has been postulated that cholesterol might influence prognosis following OHCA due to the anti-inflammatory and antioxidant effects of HDL cholesterol [33]. In our study, the lower 25th percentile lipid panel group (HDL cholesterol, LDL cholesterol, and triglyceride level) was associated with a significantly higher risk of OHCA in the multivariable logistic regression analysis (Supplementary Table 2). Therefore, not only low HDL cholesterol but also low LDL cholesterol or triglyceride level may be a risk factor for the development of cardiac arrest [18,19]. Previous studies have reported that low lipoprotein levels are associated with high mortality [34-38]. Our study has shown an association between low cholesterol and an increased occurrence of OHCA, suggesting that low lipid levels may be a risk factor for the development of OHCA.
The calculated total cholesterol cut-off values used in previous studies were 148 mg/dL and 169.5 mg/dL [30,31]. These studies used the Youden index to determine the optimal total cholesterol cut-off value. Our study identified a cut-off value from the distribution of total cholesterol levels across the national population to evaluate the risk of OHCA in the population. The cut-off values calculated in previous studies to determine a good neurological outcome in survivors of OHCA were similar to those obtained in this study when calculating the odds of occurrence of OHCA in the general population. Therefore, total cholesterol may affect the prognosis of OHCA and its occurrence through a similar mechanism.
High cholesterol levels increase the risk of cardiovascular diseases such as atherosclerosis and acute coronary syndrome [39]. Many studies have been conducted based on the hypothesis that unfavorably high cholesterol levels are a risk factor for the development of OHCA, but no clear conclusion has been reached so far [10-15]. Some studies focused on the hypothesis that low cholesterol can cause more cardiac arrests because of the belief that ŌĆśthe lower, the betterŌĆÖ. Our study found that in the general population, those with total cholesterol levels below the lower 10th percentile were at an increased risk of developing OHCA. Consistent results were also obtained when we only analyzed total cholesterol levels in the subgroup analysis. Individuals with low total cholesterol levels may have other chronic diseases or unhealthy conditions that could lead to cardiac arrest, and they may be more likely to develop cardiac arrest for this reason than the total cholesterol level itself. To overcome this bias, we selected a subgroup of patients who experienced OHCA with a relatively ŌĆśsuddenŌĆÖ onset rather than due to slower deterioration associated with a chronic disease.
Hosadurg et al. [8] conducted a case-control study on the effects on sudden cardiac death, with lipid profile as the main variable. They hypothesized that patients with sudden cardiac death would have a less favorable lipid profile than control subjects. However, the OHCA group had more favorable total, LDL, and non-HDL cholesterol levels. This suggested that there is probably no link between traditional lipid cardiovascular risk factors and sudden unexpected death. We believe that these hypotheses and explanations do not clearly distinguish between dyslipidemia and lipid levels. In our study, a relatively higher total cholesterol level was associated with a lower risk of developing OHCA. Patients that experience OHCA do not have a ŌĆśfavorableŌĆÖ lipid profile but are likely to have a dangerously low lipid profile.
In general, LDL cholesterol and triglyceride level are recognized as risk factors for the development of cardio- and cerebrovascular disease. However, the ŌĆślipid paradoxŌĆÖ concept that describes how an individualŌĆÖs prognosis is relatively poor in the presence of a low lipid profile has been proposed in studies of the elderly [40,41] as well as in studies of patients with acute myocardial infarction [42-44], heart failure [45,46], and ischemic stroke [47,48]. In one study, Lopez et al. [49] reported low total cholesterol levels to be associated with a high incidence of atrial fibrillation in the community that they studied. Based on the results of these studies, the total cholesterol level may be related to the development of cardiac arrest.
There are some limitations to this study. First, the possibility of measurement bias should be considered. In the CAPTURES group, the total cholesterol levels were not measured after standardized fasting durations and were measured in different laboratories of each hospital; thus, there is a possibility that they are not uniform and accurate. Total cholesterol levels may have decreased after cardiac arrest. In a canine CPR model, significant changes were noted in total cholesterol values obtained during CPR and at baseline (-16.4┬▒23.6 mg/dL) [37]. In our study, blood was collected immediately after arrival at the ED; thus, the time interval between cardiac arrest and blood sampling was not large. In general, hyperkalemia and metabolic acidosis occur during cardiac arrest [50]. In our studyŌĆÖs sensitivity analysis, the direction of the results did not change even when analyzing the subgroup with relatively normal potassium and pH levels. Unfortunately, the timing of blood collection for the measurement of total cholesterol was not recorded in this study. The CAPTURES project measured the time of serum troponin collection. Serum troponin and total cholesterol were likely collected simultaneously from patients in the OHCA group. The time to collect serum troponin from the estimated time of cardiac arrest was calculated for 482 patients; the average time was 84 minutes, and the median was 57.5 minutes. There was no statistical difference when comparing the distribution of total cholesterol by dividing it into two groups based on a cut-off of 60 minutes (Supplementary Table 3). In addition, there were no clear differences between the total cholesterol distributions of the short prehospital time group (<30 minutes before hospital admission) and the long prehospital time group (Supplementary Table 4). In this study, multiple imputations were applied to the missing values of all variables except the lipid panel. Further analysis was conducted to evaluate the possibility that the estimated missing values had influenced the results. When analyzing the data without imputation, the main results did not change (Supplementary Table 5). The height and weight measurements in the KNHANES registry were performed by nurses belonging to KCDC and underwent quality control. Each hospital conducts height and weight measurements independently in the CAPTURES registry; as this has not been subjected to standard quality control, the accuracy may be relatively low. Second, the possibility of selection bias should be considered. Patients who were not included in the final analysis because of missing cholesterol data were likely to have a different distribution of cholesterol levels. On comparing patients in the OHCA group whose cholesterol levels were measured to those whose cholesterol levels were not measured, no clear differences were noted in any variable (Supplementary Table 6). Third, some diseases that decrease the total cholesterol levels may have acted as confounding variables. Patients who experienced OHCA, were younger than 65 years, and did not have hypertension or diabetes could be assumed to have a relatively good physical functional status; interestingly, the results were the same when a sensitivity analysis was performed in this group. Fourth, data on underlying diseases such as coronary artery disease, which are closely related to OHCA, could not be obtained. If these data were available, these could have been used as a potential confounding variable or as a sensitivity analysis subgroup. Finally, issues related to dyslipidemia should be considered. To control the effects of dyslipidemia treatment, patients taking lipid-lowering medication were excluded from the analysis. Therefore, our study results could not address the risk of OHCA in the population that are treated for dyslipidemia. However, patients with dyslipidemia are likely to have higher total cholesterol levels than the average individual in the general population.
In conclusion, this case-control study demonstrated that having a very-low total cholesterol level was associated with the risk of OHCA. The clinical implication of this study is that low cholesterol levels should be considered important, not only in estimating the prognosis of OHCA survivors but also in predicting the development of OHCA.
ACKNOWLEDGMENTSThis study was supported and funded by the Korea Disease Control and Prevention Agency (2013-2014) (Grant No. 2013E3300500/2014E3300100).
SUPPLEMENTARY MATERIALSupplementary Tables are available from: https://doi.org/10.15441/ceem.20.114.
Supplementary┬ĀTable┬Ā1.Multivariable logistic regression analysis of total cholesterol for OHCA (with potential confounder variables) Supplementary┬ĀTable┬Ā2.Multivariable logistic regression analysis of lipid profiles for OHCA Supplementary┬ĀTable┬Ā3.Distribution of total cholesterol levels in the short sample time and long sample time groups Supplementary┬ĀTable┬Ā4.Distribution of total cholesterol levels in the short prehospital time and long prehospital time groups Supplementary┬ĀTable┬Ā5.Multivariable logistic regression analysis of total cholesterol for OHCA (without imputation data) Supplementalry┬ĀTable┬Ā6.Demographics and distribution of laboratory findings of known cholesterol cases and unknown cholesterol cases. REFERENCES1. Taniguchi D, Baernstein A, Nichol G. Cardiac arrest: a public health perspective. Emerg Med Clin North Am 2012; 30:1-12.
2. In: Committee on the Treatment of Cardiac Arrest: Current Status and Future Directions, Board on Health Sciences Policy, Institute of Medicine, Graham R, McCoy MA, Schultz AM, editors. Strategies to improve cardiac arrest survival: a time to act. Washington, DC: National Academies Press; 2015.
3. Myat A, Song KJ, Rea T. Out-of-hospital cardiac arrest: current concepts. Lancet 2018; 391:970-9.
4. Engdahl J, Holmberg M, Karlson BW, Luepker R, Herlitz J. The epidemiology of out-of-hospital ŌĆśsuddenŌĆÖ cardiac arrest. Resuscitation 2002; 52:235-45.
5. Porzer M, Mrazkova E, Homza M, Janout V. Out-of-hospital cardiac arrest. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 2017; 161:348-53.
6. Adabag AS, Luepker RV, Roger VL, Gersh BJ. Sudden cardiac death: epidemiology and risk factors. Nat Rev Cardiol 2010; 7:216-25.
7. Hess PL, Al-Khalidi HR, Friedman DJ, et al. The metabolic syndrome and risk of sudden cardiac death: the Atherosclerosis Risk in Communities Study. J Am Heart Assoc 2017; 6:e006103.
8. Hosadurg N, Bogle BM, Joodi G, et al. Lipid profiles in out-of-hospital sudden unexpected death. Mayo Clin Proc Innov Qual Outcomes 2018; 2:257-66.
9. Albert CM, Ma J, Rifai N, Stampfer MJ, Ridker PM. Prospective study of C-reactive protein, homocysteine, and plasma lipid levels as predictors of sudden cardiac death. Circulation 2002; 105:2595-9.
10. Wannamethee G, Shaper AG, Macfarlane PW, Walker M. Risk factors for sudden cardiac death in middle-aged British men. Circulation 1995; 91:1749-56.
11. Kagan A, Yano K, Reed DM, MacLean CJ. Predictors of sudden cardiac death among Hawaiian-Japanese men. Am J Epidemiol 1989; 130:268-77.
12. Jouven X, Desnos M, Guerot C, Ducimetiere P. Predicting sudden death in the population: the Paris Prospective Study I. Circulation 1999; 99:1978-83.
13. Doyle JT, Kannel WB, McNamara PM, Quickenton P, Gordon T. Factors related to suddenness of death from coronary disease: combined Albany-Framingham studies. Am J Cardiol 1976; 37:1073-8.
14. Kannel WB, Thomas HE Jr. Sudden coronary death: the Framingham Study. Ann N Y Acad Sci 1982; 382:3-21.
15. Kurl S, Laaksonen DE, Jae SY, et al. Metabolic syndrome and the risk of sudden cardiac death in middle-aged men. Int J Cardiol 2016; 203:792-7.
16. Incardona JP, Eaton S. Cholesterol in signal transduction. Curr Opin Cell Biol 2000; 12:193-203.
17. Soppert J, Lehrke M, Marx N, Jankowski J, Noels H. Lipoproteins and lipids in cardiovascular disease: from mechanistic insights to therapeutic targeting. Adv Drug Deliv Rev 2020; 159:4-33.
18. Sittiwet C, Simonen P, Gylling H, Strandberg TE. Mortality and cholesterol metabolism in subjects aged 75years and older: the Helsinki Businessmen Study. J Am Geriatr Soc 2020; 68:281-7.
19. Liu Y, Coresh J, Eustace JA, et al. Association between cholesterol level and mortality in dialysis patients: role of inflammation and malnutrition. JAMA 2004; 291:451-9.
20. Bae JM, Yang YJ, Li ZM, Ahn YO. Low cholesterol is associated with mortality from cardiovascular diseases: a dynamic cohort study in Korean adults. J Korean Med Sci 2012; 27:58-63.
21. Yamano S, Shimizu K, Ogura H, et al. Low total cholesterol and high total bilirubin are associated with prognosis in patients with prolonged sepsis. J Crit Care 2016; 31:36-40.
22. Nago N, Ishikawa S, Goto T, Kayaba K. Low cholesterol is associated with mortality from stroke, heart disease, and cancer: the Jichi Medical School Cohort Study. J Epidemiol 2011; 21:67-74.
23. Ro YS, Shin SD, Song KJ, et al. Risk of diabetes mellitus on incidence of out-of-hospital cardiac arrests: a case-control study. PLoS One 2016; 11:e0154245.
24. Kweon S, Kim Y, Jang MJ, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol 2014; 43:69-77.
25. Shin J, Lim YS, Kim K, et al. Initial blood pH during cardiopulmonary resuscitation in out-of-hospital cardiac arrest patients: a multicenter observational registry-based study. Crit Care 2017; 21:322.
26. Lee SY, Song KJ, Shin SD, Hong KJ. Epidemiology and outcome of emergency medical service witnessed out-of-hospital-cardiac arrest by prodromal symptom: nationwide observational study. Resuscitation 2020; 150:50-9.
27. Park JH, Lee SC, Shin SD, Song KJ, Hong KJ, Ro YS. Interhospital transfer in low-volume and high-volume emergency departments and survival outcomes after out-of-hospital cardiac arrest: a nationwide observational study and propensity score-matched analysis. Resuscitation 2019; 139:41-8.
28. Korean Society of Lipid and Atherosclerosis. Dyslipidemia fact sheets in Korea, 2018. Seoul: Korean Society of Lipid and Atherosclerosis; 2018.
29. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972; 18:499-502.
30. Chae MK, Lee SE, Min YG, Park EJ. Initial serum cholesterol level as a potential marker for post cardiac arrest patient outcomes. Resuscitation 2020; 146:50-5.
31. Lee HY, Lee DH, Lee BK, et al. The association between lipid profiles and the neurologic outcome in patients with out-of-hospital cardiac arrest. Resuscitation 2019; 145:26-31.
32. Kim JH, Wi DH, Lee JH, et al. Effects of cholesterol levels on outcomes of out-of-hospital cardiac arrest: a cross-sectional study. Clin Exp Emerg Med 2019; 6:242-9.
33. Son YS, Kim KS, Suh GJ, et al. Admission levels of high-density lipoprotein and apolipoprotein A-1 are associated with the neurologic outcome in patients with out-of-hospital cardiac arrest. Clin Exp Emerg Med 2017; 4:232-7.
34. Tikhonoff V, Casiglia E, Mazza A, et al. Low-density lipoprotein cholesterol and mortality in older people. J Am Geriatr Soc 2005; 53:2159-64.
35. Schupf N, Costa R, Luchsinger J, Tang MX, Lee JH, Mayeux R. Relationship between plasma lipids and all-cause mortality in nondemented elderly. J Am Geriatr Soc 2005; 53:219-26.
36. Lv YB, Yin ZX, Chei CL, et al. Low-density lipoprotein cholesterol was inversely associated with 3-year all-cause mortality among Chinese oldest old: data from the Chinese Longitudinal Healthy Longevity Survey. Atherosclerosis 2015; 239:137-42.
37. Bathum L, Depont Christensen R, Engers Pedersen L, et al. Association of lipoprotein levels with mortality in subjects aged 50 + without previous diabetes or cardiovascular disease: a population-based register study. Scand J Prim Health Care 2013; 31:172-80.
38. Ravnskov U, Diamond DM, Hama R, et al. Lack of an association or an inverse association between low-density-lipoprotein cholesterol and mortality in the elderly: a systematic review. BMJ Open 2016; 6:e010401.
39. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol 2019; 73:e285-350.
40. Schatz IJ, Masaki K, Yano K, Chen R, Rodriguez BL, Curb JD. Cholesterol and all-cause mortality in elderly people from the Honolulu Heart Program: a cohort study. Lancet 2001; 358:351-5.
41. Liang Y, Vetrano DL, Qiu C. Serum total cholesterol and risk of cardiovascular and non-cardiovascular mortality in old age: a population-based study. BMC Geriatr 2017; 17:294.
42. Cheng KH, Chu CS, Lin TH, Lee KT, Sheu SH, Lai WT. Lipid paradox in acute myocardial infarction-the association with 30- day in-hospital mortality. Crit Care Med 2015; 43:1255-64.
43. Reddy VS, Bui QT, Jacobs JR, et al. Relationship between serum low-density lipoprotein cholesterol and in-hospital mortality following acute myocardial infarction (the lipid paradox). Am J Cardiol 2015; 115:557-62.
44. Sia CH, Zheng H, Ho AF, et al. The Lipid Paradox is present in ST-elevation but not in non-ST-elevation myocardial infarction patients: insights from the Singapore Myocardial Infarction Registry. Sci Rep 2020; 10:6799.
45. Guder G, Frantz S, Bauersachs J, et al. Reverse epidemiology in systolic and nonsystolic heart failure: cumulative prognostic benefit of classical cardiovascular risk factors. Circ Heart Fail 2009; 2:563-71.
46. Rauchhaus M, Clark AL, Doehner W, et al. The relationship between cholesterol and survival in patients with chronic heart failure. J Am Coll Cardiol 2003; 42:1933-40.
47. Markaki I, Nilsson U, Kostulas K, Sjostrand C. High cholesterol levels are associated with improved long-term survival after acute ischemic stroke. J Stroke Cerebrovasc Dis 2014; 23:e47-53.
48. Patel U, Malik P, Dave M, et al. The lipid paradox among acute ischemic stroke patients: a retrospective study of outcomes and complications. Medicina (Kaunas) 2019; 55:475.
Fig.┬Ā1.Flow diagram for inclusion of the study population. CAPTURES, Cardiac Arrest Pursuit Trial with Unique Registration and Epidemiologic Surveillance; KNHANES, Korea National Health and Nutrition Examination Survey; EMS, emergency medical services; OHCA, out-of-hospital cardiac arrest. 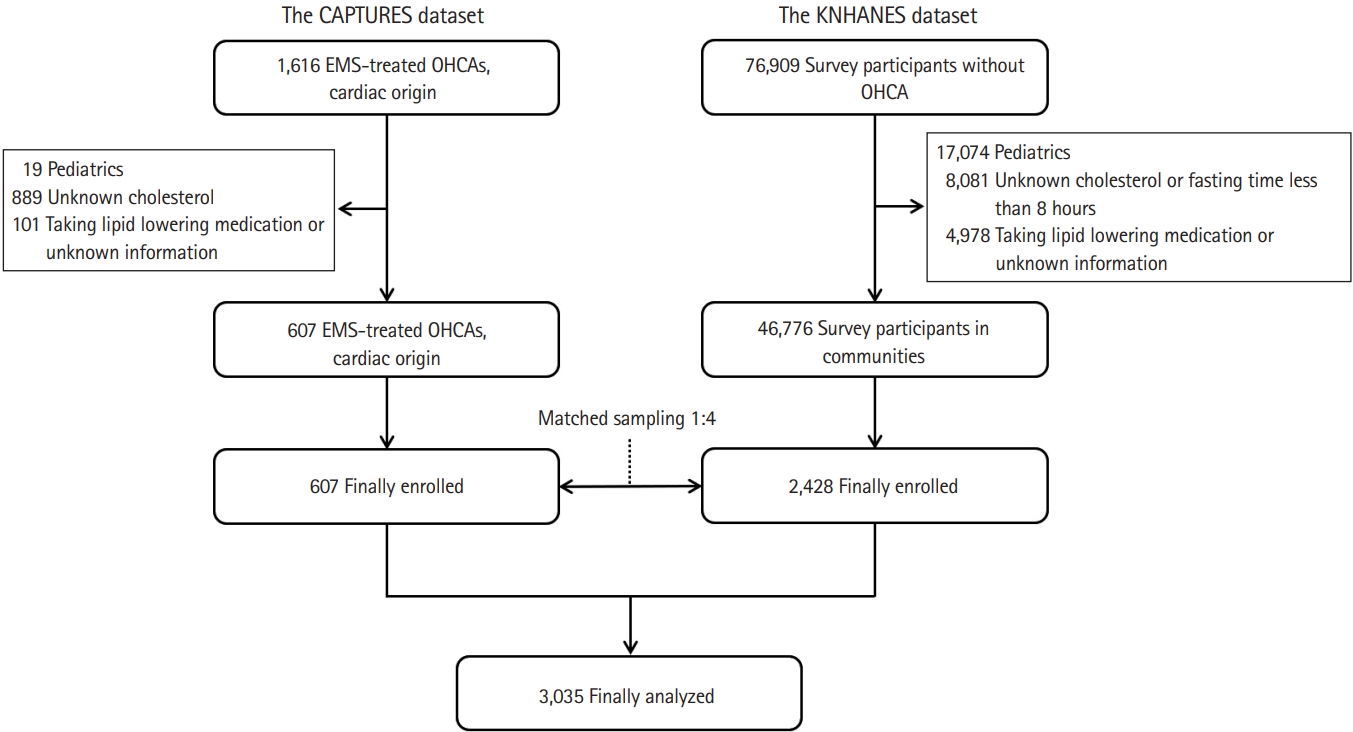
Fig.┬Ā2.Histograms of lipid profiles in both the out-of-hospital cardiac arrest and community control groups. (A) The percentage of cholesterol in each group. (B) The percentage of low-density lipoprotein (LDL) in each group. (C) The percentage of high-density lipoprotein (HDL) in each group. (D) The percentage of triglycerides in each group. 
Table┬Ā1.Demographic characteristics of OHCA patients and community controls
Table┬Ā2.Distribution of laboratory findings in OHCA patients and community controls
Table┬Ā3.Multivariable logistic regression analysis of total cholesterol levels for predicting OHCA
Table┬Ā4.Sensitivity analysis
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||