INTRODUCTION
Musculoskeletal and vascular ultrasound are core components of emergency medicine point of care ultrasound (POCUS) [1]. POCUS improves diagnosis of pathology in the superficial vascular and soft tissue structures, which are well-visualized at the bedside using modern ultrasound systems [2,3]. Musculoskeletal and vascular ultrasound is also crucial for procedures including vascular access, abscess drainage, and foreign body detection and removal [1]. These applications have uses in all areas of the body, with the knee and ankle being common musculoskeletal sites evaluated with POCUS [4].
The use of POCUS to diagnose soft tissue infection is a particularly relevant application in the emergency department (ED), where it is extremely important to differentiate between pathology such as cellulitis from rapidly progressive, life-threatening infections such as necrotizing fasciitis [2]. Abscess identification and drainage and diagnosis of infectious tenosynovitis are other applications of musculoskeletal POCUS, and each of these pathologies has a distinct ultrasound appearance [5-8]. POCUS is also a useful technology for finding collections of blood and can be used to identify vascular injury or hematoma [3,9-13]. Penetrating trauma is a mechanism that could lead to vascular injury from vessel puncture or infection through introduction of bacteria by the penetrating object [13]. Rapid diagnosis is crucial in this setting as they are both limb-threatening and have distinct treatment pathways.
This report describes a use of POCUS that demonstrates the importance of using ultrasound image characteristics to distinguish between soft tissue infections and vascular injury.
CASE REPORT
A 65-year-old female patient presented to the ED for evaluation of a hand injury. She was scratched on the dorsum of her right hand by her cat 90 minutes before presenting to the ED. Her past medical history was significant for non-ST elevation myocardial infarction and hypertension. Her only medication was aspirin. She complained of rapid onset of pain, swelling, and cyanosis of the hand as well as decreased range of motion. There were no fevers, chills, or loss of sensation.
On physical examination, the temperature was 36.6°C, pulse 113 beats/min, respiratory rate 20 breaths/min, and blood pressure 227/131 mmHg. She was in distress due to pain. Her right hand was markedly swollen, firm, and tender, with a small puncture wound on dorsum of hand (Fig. 1). She had decreased active and passive range of motion about the wrist and digits, and digits showed significant discoloration (Fig. 1). Her sensation to light touch was intact, and she had a strong radial pulse. Physical examination was otherwise unremarkable.
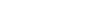
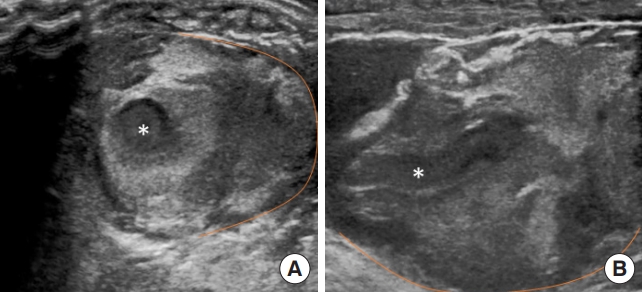
The treating physician performed point-of-care ultrasound to evaluate for evidence of vascular injury or a rapidly progressive soft-tissue infection. Using a 10-5 MHz linear transducer (Sonosite, Bothell, WA, USA), transverse and longitudinal images of the hand were obtained (Fig. 2). These images demonstrated a pulsatile vessel immediately deep to the wound (Figs. 2, 3 and Supplementary Videos 1, 2). The vessel contained hyperechoic material compatible with thrombus (Fig. 2 and Supplementary Video 1). The location was consistent with an injury to the first dorsal metacarpal artery. No definite damage to the arterial wall was visible. There was complex, hyperechoic material surrounding the vessel consistent with a hematoma or pseudoaneurysm (Fig. 2 and Supplementary Video 1). There was no evidence of shadowing air suggestive of gas-forming soft tissue infection, or well-defined collection of pus consistent with an abscess (Fig. 2 and Supplementary Video 1) [6,7]. Laboratory studies showed an international normalized ratio of 1.0, hemoglobin 16.9 g/dL, platelets 189 103/μL.
Given the clinical history and POCUS findings, a diagnosis of arterial injury was made. Hand surgery was consulted; observation and nonoperative management were recommended. There was discussion with hand surgery about the need for definitive diagnosis of arterial injury with computed tomography angiography. The consultant was satisfied with the ultrasound images and felt in this case the injury could be safely observed without advanced imaging. This management has been previously described as satisfactory when no hard signs of limb-threatening vascular injury are present [14].
The patient was given tetanus prophylaxis and ampicillin-sulbactam for infection prophylaxis. She was given ondansetron, hydromorphone, and acetaminophen to control symptoms. The hand injury was managed conservatively with a compression dressing, wrist splint, and elevation of the extremity. She was observed overnight in the ED and discharged the following morning on amoxicillin-clavulanate for infection prophylaxis with instructions to follow-up with hand surgery in the outpatient setting in 2 to 3 days for further evaluation. The patient was contacted at 1 week for follow-up and reported swelling and pain were continuing to resolve. The patient was contacted multiple months following the injury and reported regaining full range of motion and use of the hand with no additional surgical intervention.
DISCUSSION
The ultrasound findings in this case rapidly established the diagnosis of vascular injury. These findings also helped exclude an alternative, life-threatening diagnosis of a rapidly progressive infection or another actionable diagnosis such as abscess. The images demonstrate a large fluid collection with internal pulsations consistent with injury to the first dorsal metacarpal artery [3,13]. The images helped refine the differential diagnosis. The lack of shadowing air helped the clinician rule-out necrotizing fasciitis [6,7]. The sonographic appearance of an abscess could overlap with a hematoma, but given the clinical history, the location of the collection adjacent to an artery, and the pulsatile flow within the complex fluid, a diagnosis of vascular injury was more likely. Finally, there was no evidence of cobblestoning that would suggest a simple cellulitis [8]. These are all sonographic patterns that should be familiar to POCUS users, and that trainees in emergency medicine are expected to recognize by the conclusion of residency [1]. Although these competencies are often taught as distinct applications of POCUS, this case illustrates how knowledge of image characteristics for different pathologies can be combined and applied to the same clinical scenario to rapidly establish the differential diagnosis.
In summary, this application of POCUS combined clinical reasoning and ultrasound image characteristics to accurately diagnose vascular injury and rule out rapidly progressive infection. This report shows the importance of using POCUS to further diagnosis of soft tissue and vascular pathology in the setting of penetrating feline trauma. Potential limitations of these applications include experience of the sonographer, as the physician in this case was a ultrasound fellowship-trained emergency physician. A less-experienced provider may not be able to confidently distinguish between the different possible images. However, these POCUS skills are core competencies of contemporary emergency medicine programs. This case highlights the need for an integrative approach to teaching ultrasonography of superficial musculoskeletal and vascular structures.