AbstractObjectiveThis study aimed to describe the relationship between sex and survival in patients experiencing unintentional trauma.
MethodsThis retrospective, national population–based observational, case-control study involved a cohort of Korean trauma patients who were transferred to an emergency department by a Korean emergency medical service from January 1 to December 31, 2018. Propensity score matching was used. The primary outcome was survival until hospital discharge.
ResultsOf 25,743 patients with severe unintentional trauma, 17,771 were male and 7,972 were female. Prior to propensity score matching, there was no significant difference in survival among male and female patients (92.6% vs. 93.1%, P=0.105). After using propensity score matching to adjust for confounders, there was still no sex difference in survival (male, 93.6% vs. female, 93.1%; P=0.270).
INTRODUCTIONTrauma is a major cause of death worldwide. More than five million people die every year due to trauma [1]. Therefore, many researchers have attempted to develop treatment guidelines for trauma patients. Several investigators have recently focused on the effect of the patient’s sex on survival after trauma; however, these efforts have produced conflicting results. Some researchers have argued that estrogen is associated with more favorable outcomes in terms of survival due to its protective effect [2,3]. Studies in rodents have indicated estrogen has beneficial effects in multiple tissues after trauma: estrogen reduces cerebral edema and neuronal degeneration in the central nervous system [4], alters the expression of heat shock proteins in the cardiovascular system [5], reduces the pulmonary inflammatory response to severe blood loss [6], and reduces renal ischemia-perfusion injuries [7]. One study argued that female sex was associated with a lower intensive care unit (ICU) admission rate in those aged 16 to 44 years [8]. Another study reported that female trauma patients had a significantly lower risk of in-hospital mortality compared to male patients, an association that was most apparent in patients younger than 50 years of age [9]. Moreover, another study reported that women of reproductive age had better organ function after traumatic injury or hemorrhagic shock than men of corresponding age [10]. A study conducted in a regional trauma center reported that the patient’s sex was independently associated with death after major trauma [11,12].
As the potentially beneficial effect of being female by birth on survival of severely injured patients has not yet been firmly established, a nationwide Korean population–based study was performed to investigate the associations between sex and survival outcomes among severely injured patients. We hypothesized that female patients with trauma would have a lower mortality rate.
METHODSEthics statementThe study was approved by the Institutional Review Board of Kyung Hee University Hospital at Gangdong (No. 2022-05-056). The requirement for informed consent was waived due to the retrospective nature of the study.
Study design and settingThis was a retrospective study conducted in Korea, based on the 2018 Community-based Severe Trauma Survey, which was compiled and released by the Korea Disease Control and Prevention Agency (KDCA) with the approval of Statistics Korea in 2019 [13]. Data were collected from patients who experienced severe or multiple trauma and were transported by the Korean emergency medical services (EMS) to a hospital between January and December 2018. The Korean EMS is a government-provided system headed by the National Emergency Management Agency in Korea, which is responsible for providing advanced cardiovascular life support (ACLS) and basic life support (BLS) systems throughout the 17 provincial headquarters. All ambulances are equipped with automated external defibrillators (AEDs) and two or three emergency medical technicians (EMTs) who can administer intravenous fluids and undertake advanced airway management, including endotracheal intubation. Moreover, Korea has a unique trauma center system that divides medical centers by profession and severity of the disease: regional trauma, regional emergency, and local emergency centers. Also, trauma patient transfer guidelines for EMS have been developed to ensure the patient is transported to the correct level of emergency center.
Data collection and processThe Community-based Severe Trauma Survey was constructed based on the medical records of hospitals that were previously associated with the Korea National Fire Agency (NFA) and underwent a nonidentification procedure based on the Korean Personal Information Protection Act and the Statistics Act. A communitybased investigator visited the medical institutions to double-check the credibility of the medical records. The data were verified by the KDCA. The survey items included demographic and injury information, progress after initiating medical involvement, and outcomes after hospitalization [13].
The Revised Trauma Score (RTS) and Injury Severity Score (ISS) were used to quantify the severity of trauma. RTS is considered a convenient tool for trauma triage, especially in prehospital settings. This score is based on the patients’ Glasgow Coma Scale (GCS), systolic blood pressure, and respiratory rate. The RTS results ranged from 0 to 12, with a score of 12 recorded for patients with normal vital signs [14]. In the prehospital phase, the EMTs evaluated and collected patient information. If the collected data included any of systolic blood pressure less than 90 mmHg, respiration rate less than 10 or more than 29 breaths/min, or abnormal consciousness, the RTS score was automatically less than 12. After gathering information relating to the RTS score, the EMS provider determined the severity of trauma based on the collected data.
The ISS is another widely used scale suitable for use during the hospital phase to evaluate patients with trauma [15]. The ISS is based on the Abbreviated Injury Scale (AIS), which divides the body into six parts (head, face, chest, abdomen, limb, and external), and each part is assigned a severity score ranging from 0 (no damage) to 5 (severe damage). The sum of the three highest scores among the six parts was used to calculate the ISS score [16].
An ISS score greater than or equal to 16 was generally considered to represent severe trauma. Patients who initially had abnormal RTS values and ISS scores greater than 16, as analyzed by the healthcare providers in the hospital following their arrival, were considered for inclusion in our study analyses.
Data regarding injuries and outcome parameters among male and female patients were collected from the trauma registry. Injury was categorized by severity, ISS, and mechanism of injury (transportation incidents, falls, other, or unknown).
Other covariables were age, elapsed time from call to patient transfers to the site by the EMS, hospital class (regional trauma center, regional emergency center, local emergency center; later simplified to trauma center and nontrauma center), and interventions performed. The Korean government designed a national trauma system in 2012, under which national trauma centers were created to efficiently provide medical care for patients with major trauma.
The study data were divided into three categories: (1) initial disposition plan in an emergency department (such as survival to discharge, survival to transfer, survival to admission, and death after CPR); (2) final outcome after hospitalization (survival or death); and (3) final outcome after emergency department (ED) visit (survival or death). We analyzed the data for patients who transferred to a second hospital in a similar manner.
Statistical analysisThe median and interquartile range were calculated for continuous variables, and numbers and percentages were calculated for categorical variables. The patients were divided into two groups (male and female at birth). To compare the two groups, the MannWhitney test was used for continuous variables, and the chi-square test was used for categorical variables. Since patient age, ISS, and the elapsed time between the emergency line (119) call to site arrival variables did not follow a normal distribution, a nonparametric test was used. To eliminate the effect of confounding variables that may influence outcome variables, when analyzing basic characteristics, a propensity score matching (PSM) method was used to collect data for both groups. Exact matching was used to match male patients 1:1 with female patients according to propensity score. Using matched data, differences between male and female variables were reanalyzed.
All statistical analyses were performed using R ver. 4.2.3 (R Foundation for Statistical Computing). P-values were based on a two-sided significance level of 0.05.
RESULTSA total of 52,262 patients were transported to EDs by EMS in Korea in 2018. A total of 6,018 patients with unknown RTSs (such as dead on arrival or out-of-hospital cardiac arrest [OHCA]), 10,235 patients with RTS of 12 or who had missing data, and 10,266 patients with intentional injury were excluded. Finally, 25,743 patients, comprising 17,771 men and 7,972 women, were considered to have experienced an unintentional traumatic injury. Patient matching was achieved for 61.9% (15,944 of 25,743), comprising 44.9% of men (7,972 of 17,771) and 100% of women (7,972 of 7,972) (Fig. 1).
The male patients were significantly younger than the female patients (52 years [range, 33−64 years] vs. 58 years [range, 36−74 years], P<0.001). The median ISS was higher in male patients than in female patients (5 [range, 1−13] vs. 4 [range, 1−10], P<0.001). A greater percentage of male trauma patients tended to be admitted to regional trauma centers or regional emergency centers than of female patients. The elapsed time between the 119-emergency call and EMS arrival at the hospital was shorter for male patients than for female patients (27 minutes [range, 19−40 minutes] vs. 26 minutes [range, 19–38 minutes], P<0.001). The mechanisms of injury differed between sexes as well. Transportation incidents and falls were the second most frequent causes of trauma in both sexes; however, transportation accidents were more frequent in men than in women (46.7% vs. 42.8%, P<0.001) (Table 1).
No differences in survival after admission were found between the two groups of patients; however, the clinical plans implemented in the emergency departments differed for male and female patients. A greater percentage of male patients underwent operations or interventions (23.7% vs. 19.6%, P<0.001) and were admitted to the ICU (57.0% vs. 44.5%, P<0.001). Moreover, male patients tended to be admitted (44.1% vs. 40.9%, P<0.001) or transferred to other hospitals (14.3% vs. 11.5%, P<0.001) more frequently than female patients, while a greater percentage of female patients tended to be discharged from hospital (46.3% vs. 39.8%, P<0.001). As a result, female patients who were treated only at the initial hospital more frequently survived their traumatic injury than male patients (82.9% vs. 79.3%, P<0.001), while male patients were more frequently transferred to other institutions (14.3% vs. 11.5%). Of 17,771 male patients, 7,067 (39.8%) survived to discharge from the ED, while 7,841 (44.1%) were admitted to the hospital. Among the 7,841 male patients who were admitted, 7,027 (89.6%) survived after hospital admission. Of 7,972 female patients, 3,688 (46.3%) survived to discharge from the ED, while 3,264 (40.9%) were admitted. Among the 3,264 female patients who were admitted, 2,924 (89.6%) survived to hospital discharge. In total, 14,094 of 17,771 male patients (79.3%) and 6,612 of 7,972 female patients (82.9%) survived after arrival at the ED (P<0.001) (Table 2).
With regard to transfers, 2,545 male and 919 female patients were transferred to another hospital after the initial evaluation, but data from 752 male and 261 female transferred patients were missing. Based on the data of 2,545 male and 919 female transferred patients, there was no sex differences in overall admissions and ICU admissions after transfer to a second hospital. Of 1,793 male patients transferred to another hospital for whom data were available, 96 survived to discharge from the ED and 1,597 (89.1%) were admitted. Among the 1,597 male patients admitted to hospital, 1,432 (89.7%) survived to discharge. In contrast, of the 658 female patients transferred to another hospital for whom data were available, 34 (5.2%) survived to discharge from the ED and 573 (87.1%) were admitted. Among the 573 female patients admitted to hospital, 500 (87.3%) survived to discharge. As a result, a significantly greater percentage of men (1,528 of 1,793, 85.2%) than women (534 of 658, 81.2%) survived (P=0.047) (Table 3).
Total survival comprised patients who survived in the initial hospital and those who survived in a transfer hospital. In summary, 14,094 male patients (79.3%) and 6,612 female patients (82.9%) who were treated only at the initial hospital survived, and 1,528 male patients (85.2%) and 534 female patients (81.2%) who were transferred to another hospital survived. Overall, 15,622 of 16,879 male patients (92.6%) and 7,146 of 7,673 female patients (93.1%) survived (P=0.105). No sex difference was observed in survival of trauma patients, including the results after transfer to a second hospital (Table 3 and Figs. 2, 3).
To control for factors other than patient sex that might have influenced their survival after traumatic injury, PSM was conducted. No differences between male and female patients were found with respect to age, ISS, elapsed time from the 119-emergency call to site to patient transport to the hospital by the EMS, level of care at transfer hospital, and injury mechanism (Table 4).
No differences in intervention rate or survival after admission were found between groups with matched data. However, the clinical plans implemented in the emergency departments were different for male and female patients. A greater percentage of male than female patients was admitted to the ICU (20.1% vs. 18.2%, P=0.003). Moreover, a greater percentage of female patients was treated at the primary hospital and either discharged from the ED (46.3% vs. 45.5%, P<0.001) or admitted (40.9% vs. 38.9%, P<0.001), while male patients were more frequently transferred to other hospitals (13.9% vs. 11.5%, P<0.001). At the initial hospital, female patients survived more frequently than male patients (82.9% vs. 80.6%, P<0.001) (Table 5).
Among the matched patients, 1,112 men and 919 women were transferred to a secondary hospital, but the data for 334 of these men and 261 of these women were missing; data for 778 men and 658 women who were transferred to other hospitals were collected. Among transferred patients with matched data, there were no differences between men and women with respect to the percentages admitted to hospital or to the ICU or survival after admission. By summing the survival result after disposition in the initial hospital or in the transfer hospital, no survival difference was observed between sexes (male, 93.6% vs. female, 93.1%; P=0.270) (Table 6).
DISCUSSIONSex-dependent survival of severely injured patients is an emerging medical issue. Laboratory and clinical data related to this issue have been collected in many different countries; however, to date, most studies of the effect of sex on mortality have been conducted in European countries [2,3,8,11,12,15,17–22]. In a singlecenter study in China, female patients with severe blunt trauma had significantly lower mortality rates than male patients [23]. Our study is the first nationwide retrospective study in Korea to study the relationship between sex and survival in trauma patients. Our study included data for a large study population that was obtained without restrictions due to the size of the hospital or region.
In this study, no statistically significant survival advantage was evident for either sex. Overall, a significantly lower percentage of women underwent general admission, ICU admission, or surgical or angiographic interventions. However, these findings may have been due to confounders, including trauma severity and age. The female patients had significantly lower ISS values and were older than the male patients; the risks associated with surgical or angiographic interventions might be expected to be greater among the female patients and medical professionals may be hesitant to provide such interventions. Nonetheless, physicians consider many factors other than age and severity of trauma when making treatment decisions. Since the data did not include the thoughts of doctors making certain medical decisions, we only could infer those factors may impact the treatment plans.
After controlling for potential confounders (age, severity of trauma, elapsed time from 119-emergency call to site arrival, level of care at transfer hospital) through PSM, there was no statistically significant difference in the survival of male and female trauma patients in our study. However, male sex was associated with transfer to another institution, and female sex was associated with final medical decision of admittance or discharge in the primary hospital.
In our study, the mean age of the female patients was 53.2 years, and most were postmenopausal. The absence of sex-dependent differences in survival of trauma patients in this study may have been due to the decline in estrogen production in post-menopausal women, as was postulated in many previous studies, but the results of those studies have been equivocal. In one study investigating the relationship between trauma patient sex and mortality, logistic regression failed to identify any such association [17]. However, a study conducted in the Netherlands found that male sex was associated with ICU admission in those aged 16 to 44 years, but this association was not identified in the overall study population [8]. In addition, another study concluded that improvement in multiple organ dysfunction after trauma occurred more frequently in women aged 16 to 44 years than in men of the same age group [10]. Previous studies showed that lower ICU admission rate and higher organ function improvement in women of reproductive age than men, but the result of our studies (women with median age of 58 years showed no difference in mortality after trauma compared to men) did not show a significant protective effect of estrogen against stressful conditions, such as trauma.
Another possible theory is that the protective effect of estrogen existed only in the premenopausal group. In a rodent study, young female mice (6–8 weeks old) had a more favorable immune response to sepsis, such as increased release of proinflammatory cytokines, than male mice of the same age; however, the opposite relationship between mouse sex and immune response was observed in aged mice (2 years old) with reduced sex hormone levels. Since proinflammatory cytokines are released in trauma, the difference of release level between sexes could cause differences in survival of trauma patients. Similar results have been noted in clinical settings. McLauchlan et al. [18] reviewed patients with a mean age of 66 years who were admitted to the ICU because of abdominal sepsis. They concluded that age and female sex were independent risk factors for higher mortality. Further investigation is needed to subdivide our patient groups by age to assess potential protective effects of estrogen. In our study, such analysis could not be performed due to the skewed population of our data: the premenopausal population was too small to categorize.
It is also possible that estrogen provides protective effects in severe trauma, but this effect likely is minimal. This hypothesis is compatible with that of a meta-analysis conducted in 2015, in which Liu et al. [9] compared the risk of death in women with minor-to-moderate injuries or severe injury. The effects of estrogen may not have been prominent in our study since our outcome of interest was survival, not duration of hospital admission or rate of complications after trauma. Moreover, a rodent study argued that proestrus females had greater survival after trauma, as their circulating blood volumes were greater than those of male rodents during and after trauma-hemorrhage [19]. This difference could be eliminated simply in the hospital setting by proactive transfusion of trauma patients, which is standard therapy in major trauma, especially in the regional trauma center setting.
Another possibility is that the protective effect of estrogen is present for only a brief period after a stressful event. Choi et al. [24] assessed differences in survival among male and female patients after OHCA and concluded that women in the reproductive age group had a better chance of survival than men. Their conclusion is consistent with the findings of Deitch et al. [20] and McKinley et al. [21], who speculated that the initial protective effect of elevated estrogen decreased with time from the initial injury. Therefore, the protective effect may exist only in a brief period that may have ended prior to hospital arrival.
The major difference between animal studies and clinical settings is that humans can verbally explain their symptoms. The decision to admit is determined by a doctor based not only on objective findings, but also on subjective findings. If one sex subjectively expresses more symptoms than the other, it may influence the doctor’s decision to admit. In one study that analyzed the outcomes after mild traumatic brain injury in male and female patients, poor coping style was associated with increased postconcussive symptoms, and this was more prevalent in women than in men [22]. As we collected data addressing survival after ED arrival, the reasons for admission were not available. If one sex was admitted more frequently due to subjective symptoms rather than based on severity of trauma, our data could be misinterpreted.
Since the data we collected represent only one year, this study has some limitations. Among the patients with severe trauma, there were too few of reproductive age to analyze as a separate group. To better evaluate the effect of estrogen on severe trauma, further research should be performed after collecting data for several years. Second, there were missing and excluded data as the study was based on a retrospective analysis. Initially, we excluded 10,266 cases categorized as intentional injury, accidental self-harm, or suicide (Fig. 1). These 10,266 cases accounted for almost 20% of the total data collected; however, given that intentional injury and self-harm may have different traumatic mechanisms than those responsible for nonintentional trauma and were beyond the scope of our interest, we excluded the data.
Moreover, significant data were missing from the records of many transferred patients (Table 3), notably the reasons for transfer. Patients may have been transferred from higher-grade hospitals (i.e., tertiary hospitals) to general hospitals due to a shortage of beds or from a low-grade hospital to a tertiary hospital due to severity of trauma; however, because our collected data did not include this information, the analyzed data may have been biased. These missing data were crucial for interpreting the information presented in Table 5. Men were more frequently transferred from the initial hospital to other institutions, but we could not interpret this finding further due to the lack of information. Last, since some data, such as the RTS and ISS, were provided by the EMTs and medical providers, bias could have occurred.
In conclusion, the survival of severely injured female patients admitted to emergency departments in Korea was not significantly different from that of male trauma patients. Future research should focus on the relationships between the sex of the patient and their estrogen concentrations on survival among trauma patients of reproductive age and on the reasons why trauma patients are transferred to other institutions after arriving at the ED or being admitted.
NOTESETHICS STATEMENTS
The study was approved by the Institutional Review Board of Kyung Hee University Hospital at Gangdong (No. 2022-05-056). The requirement for informed consent was waived due to the retrospective nature of the study.
AUTHOR CONTRIBUTIONS
Conceptualization: SJM, HZC; Data curation: HZC, JK; Formal analysis: SJM, HZC, JK; Investigation: SJM, HZC; Methodology: HZC; Project administration: MCK, HZC; Supervision: MCK; Visualization: SJM; Writing–original draft: SJM; Writing–review & editing: all authors. All authors read and approved the final manuscript.
ACKNOWLEDGMENTSThe authors thank the Korea Disease Control and Prevention Agency (KDCA) for their cooperation in establishing the database.
REFERENCES1. World Health Organization (WHO). Injuries and violence: the facts 2014. WHO; 2014.
2. Angele MK, Frantz MC, Chaudry IH. Gender and sex hormones influence the response to trauma and sepsis: potential therapeutic approaches. Clinics (Sao Paulo) 2006; 61:479-88.
3. Choudhry MA, Bland KI, Chaudry IH. Trauma and immune response: effect of gender differences. Injury 2007; 38:1382-91.
4. Kim H, Cam-Etoz B, Zhai G, Hubbard WJ, Zinn KR, Chaudry IH. Salutary effects of estrogen sulfate for traumatic brain injury. J Neurotrauma 2015; 32:1210-6.
5. Dhamad AE, Zhou Z, Zhou J, Du Y. Systematic proteomic identification of the heat shock proteins (Hsp) that interact with estrogen receptor alpha (ERa) and biochemical characterization of the ERa-Hsp70 interaction. PLoS One 2016; 11:e0160312.
6. Yu HP, Yang S, Hsieh YC, Choudhry MA, Bland KI, Chaudry IH. Maintenance of lung myeloperoxidase activity in proestrus females after trauma-hemorrhage: upregulation of heme oxygenase-1. Am J Physiol Lung Cell Mol Physiol 2006; 291:L400-6.
7. Rusai K, Prokai A, Szebeni B, et al. Gender differences in serum and glucocorticoid regulated kinase-1 (SGK-1) expression during renal ischemia/reperfusion injury. Cell Physiol Biochem 2011; 27:727-38.
8. Pape M, Giannakopoulos GF, Zuidema WP, et al. Is there an association between female gender and outcome in severe trauma? A multi-center analysis in the Netherlands. Scand J Trauma Resusc Emerg Med 2019; 27:16.
9. Liu T, Xie J, Yang F, et al. The influence of sex on outcomes in trauma patients: a meta-analysis. Am J Surg 2015; 210:911-21.
10. Trentzsch H, Nienaber U, Behnke M, Lefering R, Piltz S. Female sex protects from organ failure and sepsis after major trauma haemorrhage. Injury 2014; 45 Suppl 3:S20-8.
11. Magnotti LJ, Fischer PE, Zarzaur BL, Fabian TC, Croce MA. Impact of gender on outcomes after blunt injury: a definitive analysis of more than 36,000 trauma patients. J Am Coll Surg 2008; 206:984-92.
12. Napolitano LM, Greco ME, Rodriguez A, Kufera JA, West RS, Scalea TM. Gender differences in adverse outcomes after blunt trauma. J Trauma 2001; 50:274-80.
13. Korea Disease Control and Prevention Agency (KDCA). Community-based severe trauma survey. KDCA; 2019.
14. Jeong JH, Park YJ, Kim DH, et al. The new trauma score (NTS): a modification of the revised trauma score for better trauma mortality prediction. BMC Surg 2017; 17:77.
15. Butcher NE, D’Este C, Balogh ZJ. The quest for a universal definition of polytrauma: a trauma registry-based validation study. J Trauma Acute Care Surg 2014; 77:620-3.
16. Greenspan L, McLellan BA, Greig H. Abbreviated Injury Scale and Injury Severity Score: a scoring chart. J Trauma 1985; 25:60-4.
17. Croce MA, Fabian TC, Malhotra AK, Bee TK, Miller PR. Does gender difference influence outcome? J Trauma 2002; 53:889-94.
18. McLauchlan GJ, Anderson ID, Grant IS, Fearon KC. Outcome of patients with abdominal sepsis treated in an intensive care unit. Br J Surg 1995; 82:524-9.
19. Kuebler JF, Toth B, Rue LW 3rd, Wang P, Bland KI, Chaudry IH. Differential fluid regulation during and after soft tissue trauma and hemorrhagic shock in males and proestrus females. Shock 2003; 20:144-8.
20. Deitch EA, Livingston DH, Lavery RF, Monaghan SF, Bongu A, Machiedo GW. Hormonally active women tolerate shock-trauma better than do men: a prospective study of over 4000 trauma patients. Ann Surg 2007; 246:447-55.
21. McKinley BA, Kozar RA, Cocanour CS, et al. Standardized trauma resuscitation: female hearts respond better. Arch Surg 2002; 137:578-84.
22. Bazarian JJ, Blyth B, Mookerjee S, He H, McDermott MP. Sex differences in outcome after mild traumatic brain injury. J Neurotrauma 2010; 27:527-39.
Fig. 1.Inclusion and exclusion flowchart. ED, emergency department; OHCA, out-of-hospital cardiac arrest; DOA, dead on arrival; RTS, Revised Trauma Score. 
Fig. 2.Flowchart for male trauma patients. ED, emergency department; CPR, cardiopulmonary resuscitation. 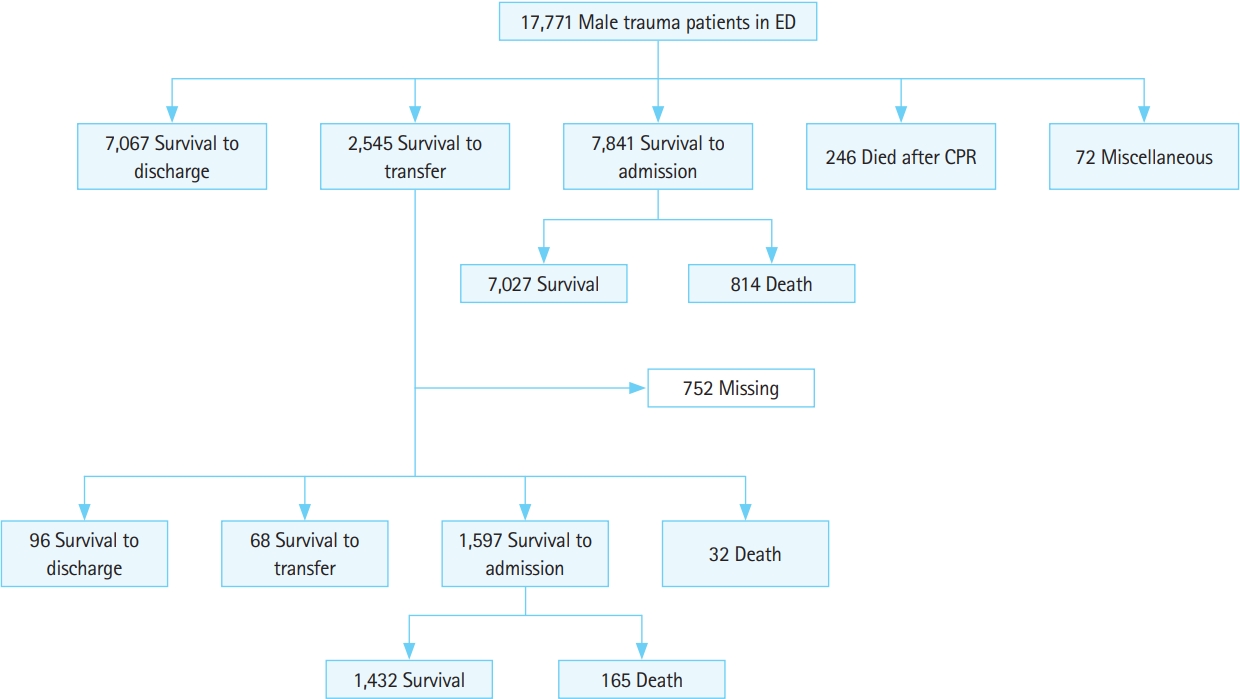
Fig. 3.Flowchart for female trauma patients. ED, emergency department; CPR, cardiopulmonary resuscitation. 
Table 1.Basic characteristics of trauma patients at emergency departments (n=25,743) Table 2.Comparison of trauma patient outcomes (n=25,743)
Table 3.Comparisons of survival rate after admission and after transfer to other hospitals among traumatic patients
Table 4.Basic characteristics of trauma patients at emergency departments after propensity score matching (n=15,944) Table 5.Comparison of trauma patient outcomes after propensity score matching (n=15,944)
Table 6.Comparison of trauma patient outcome after transfer after propensity score matching
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||