Dear Editor,
In the mid-2000s, the supraclavicular brachial plexus (SBP) block surfaced in emergency medicine literature; case reports and series demonstrated it as an effective means for managing challenging upper extremity (UE) injuries [1ŌĆō4]. Despite its appeal, the SBP block has not gained significant traction in emergency departments (EDs) and is taught rarely in academic emergency medicine curricula. We believe that, though the SBP block is underappreciated, it is extremely valuable and should be learned, taught, and utilized in emergency practice.
One of the main advantages of SBP block is that it is simple to setup. Most brachial plexus blocks involve special equipment not readily accessible in the ED, such as spinal needles, intravenous tubing, and a long linear probe for ultrasound (US). An SBP block, however, only requires a 22-gauge needle, a 20-mL syringe, and a simple short linear probe already included on most US systems.
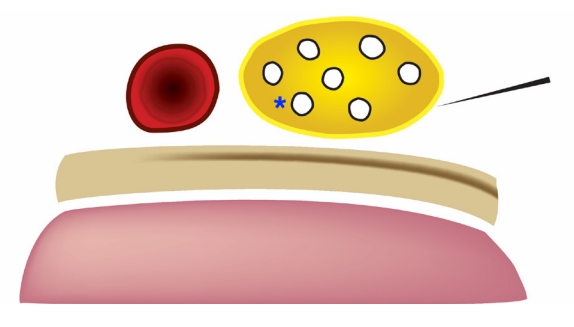
During the procedure, patients can position the UE in adduction as comfortably as possible since no special positioning is required for the procedure. In addition, the SBP block is simple to learn and perform. With the linear probe situated in the supraclavicular fossa, the SBP is visualized on US immediately lateral to the subclavian artery and superior to the first rib and pleura. The shallow position of 1 to 2 cm below the skin surface allows easy accessibility to the SBP [5]. Under US guidance, the physician directs a needle in-plane from lateral to medial toward the SBP and instills local anesthetic within or just outside the sheath (Supplementary Video 1). Injecting at the inferior ŌĆ£corner pocketŌĆØ nearest the subclavian artery within the SBP sheath guarantees dense anesthesia directly targeting the inferior trunk (Figs. 1, 2) [6,7]. The onset of anesthesia occurs within minutes of injection [6].
To complement its easy learning curve, the SBP block boasts an excellent safety profile. Though pneumothorax is a well-known complication, US guidance has significantly minimized this risk [8ŌĆō11]. Also, the first rib acts as a backstop to the needle path and may prevent pneumothorax even if the physician advances past the SBP. As with all brachial plexus blocks above the clavicle, hemidiaphragmatic paralysis may persist in up to 70% of patients after an SBP block [12]. However, Renes et al. [13] demonstrated significantly lower rates of hemidiaphragmatic paralysis using less than 20 mL of ropivacaine for a SBP block. Transient hemidiaphragmatic paralysis secondary to phrenic nerve palsy is common after brachial plexus blocks such as the interscalene nerve block, SBP block, and infraclavicular brachial plexus block [14,15]. Yet healthy patients without chronic cardiac or pulmonary disease or obesity tend not to experience respiratory compromise [14], perhaps because the minor respiratory muscles (sternocleidomastoid, scalene, and intercostals) and contralateral hemidiaphragm compensate. While vascular puncture is also a concern, the subclavian artery lies on the opposite side of the approach, and there are no major arteries in the needle trajectory. Additionally, neuropraxia is a worrisome but relatively infrequent outcome [16]. In a retrospective review performed by Liu et al. [17], 17% of perioperative US-guided SBP blocks involved inadvertent intraneural injection, but no patients suffered brachial plexus injury. Other complications include Horner syndrome and, as with any nerve block, local anesthetic systemic toxicity (LAST). Similar to hemidiaphragmatic paralysis, the risk of LAST can be minimized with lower doses of anesthetic [18].
The SBP block is a safe and powerful technique that enables physicians to anesthetize the entire upper limb including the shoulder in the frequent UE injuries presenting to the ED [5]. There is no equivalent nerve block for the chest, back, or lower extremities. In our ED, for example, we have employed the SBP block for anterior shoulder dislocations; wrist, elbow, and humerus fractures; complicated lacerations; and postoperative compressive neuropathy. Published reports have used it for UE abscesses, fractures, and joint dislocations [1ŌĆō4]. While other brachial plexus blocks are useful for UE anesthesia, each has its own imperfections. The interscalene block, for example, only anesthetizes the sensory distribution of C5ŌĆōC7 and excludes the inferior trunk (C8ŌĆōT1) of the brachial plexus, limiting its use for injuries distal to the elbow. The infraclavicular brachial plexus block, on the other hand, involves a daunting needle trajectory aimed toward the pleura and may also require multiple needle passes. The blind needle path of the retroclavicular approach to the infraclavicular region under the clavicle is followed by a narrow lane between the pleura and the axillary artery, hindering novice users. The axillary nerve block also involves multiple needle passes and requires that the patient abduct the arm, making its impractical for particular injuries.
Musculoskeletal pain is the most common complaint in the ED, and there is no one-size-fits-all technique for management. While the SBP block is not superior to all other brachial plexus blocks, it is undervalued and underutilized in emergency medicine. Considering the ease, safety, and potency of the SBP block, emergency physicians should include the SBP block in the multimodal approach to acute pain.