Acute subclavian artery occlusion mimicking cerebral infarction
Article information
A 92-year-old female patient presented to the emergency department with sudden onset of left-arm weakness. Initial neurological examination revealed grade II motor weakness in the left upper extremity. Brain computed tomography showed no hemorrhage, and diffusion-weighted image showed no definite acute infarction (Fig. 1A). However, magnetic resonance angiography revealed a left subclavian artery occlusion (Fig. 1B). On physical reexamination, we found that her left arm was pale and cold, the brachial pulse was very weak, and the radial pulse was not palpable. Additional upper extremity computed tomography angiography was performed. Computed tomography angiography showed an abrupt contrast filling defect of the left subclavian, axillary, and forearm arteries, and we could partially visualize the axillary artery from the middle of the humerus to the elbow level (Fig. 1C, D). The patient’s symptom of left arm weakness was suspected to be due to subclavian artery occlusion. The patient was transferred to a vascular surgeon and underwent an emergency arterial thrombectomy (Fig. 2). After the surgery, the patient’s arm weakness and sensation improved, and she was discharged without complications.
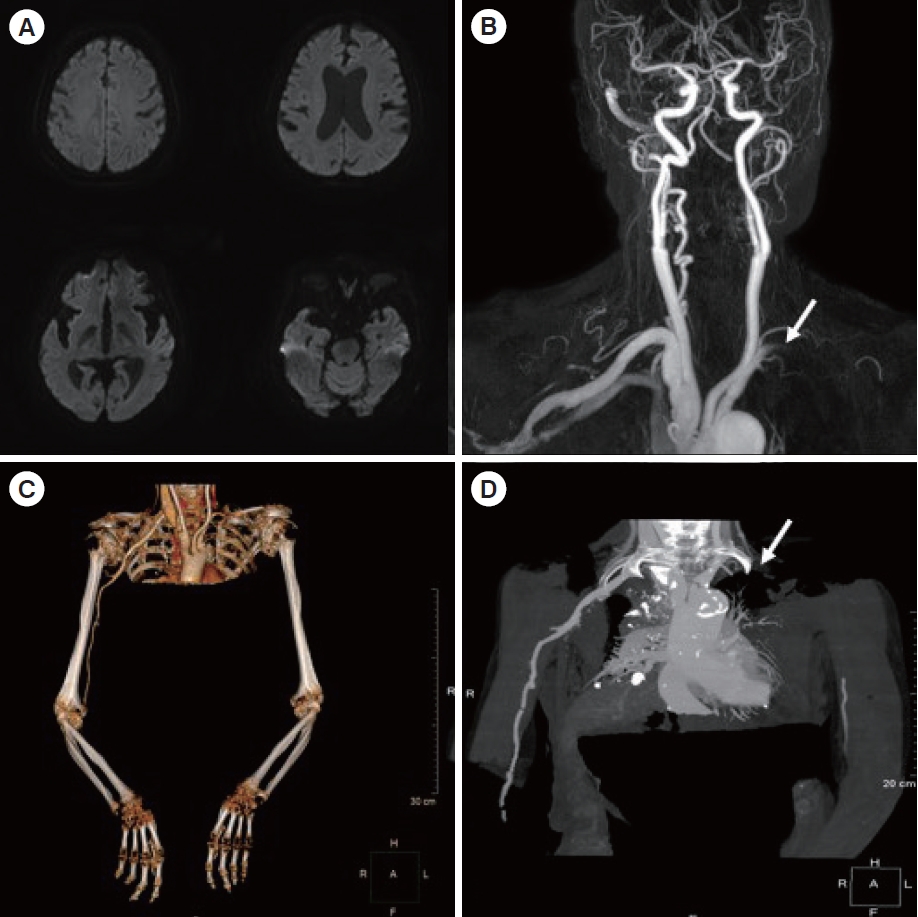
Magnetic resonance imaging and computed tomography angiography of the patient. (A) Diffusion-weighted image shows no definite cerebral infarction. (B) Magnetic resonance angiography shows left subclavian arterial occlusion (arrow). (C, D) Computed tomography angiography shows an abrupt contrast filling defect of left subclavian, axillary, and forearm arteries. Partially visualized axillary artery from the middle of the humerus to elbow level (arrow).
Common conditions that mimic stroke include seizures, toxins, hypoglycemia, syncope, psychiatric disorders, brain tumors, and spinal cord lesions [1,2]. This report presents an unusual case of a patient with acute subclavian arterial occlusion that presented as a stroke mimic. We recommend that patients suspected of having a stroke with acute hemiparesis be examined thoroughly for cold skin, pulselessness, weak pulse, pale skin color, and paresthesia to evaluate arterial occlusive disease. Informed consent for publication of the research details and clinical images was obtained from the patient.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization: SKO; Data curation: SKO; Formal analysis: SUC; Investigation: SUC; Methodology: SKO; Project administration: SKO; Resources: SUC; Software: SUC; Supervision: SKO; Validation: SUC; Visualization: all authors; Writing–original draft: all authors; Writing–review & editing: all authors. All authors read and approved the final manuscript.
References
Article information Continued
Notes
Capsule Summary
What is already known
Several clinical conditions can mimic ischemic stroke.
What is new in the current study
Upper limb weakness can be caused by subclavian artery occlusion. Patients with acute hemiparesis have to be evaluated for arterial occlusive disease.

