Usability testing of a blind intubation device for intubation novices: a randomized crossover simulation study
Article information
Abstract
Objective
A new blind intubation device (BID) has been developed for endotracheal intubation. This study aimed to test the usability of the BID in comparison to direct laryngoscopy (DL) and video laryngoscopy (VL) with inexperienced healthcare providers for endotracheal intubation.
Methods
This was a randomized crossover simulation study. Participants who had conducted fewer than five live intubation sessions were included in the study. The manikin simulation was conducted using a Laerdal trainer airway manikin. Participants performed intubation using all three devices, DL, VL, and BID. The primary outcome was intubation success rate in the first pass the secondary outcome was intubation time to first ventilation, and the tertiary outcome was dental injury.
Results
A total of 45 healthcare workers who were novices in intubation participated in this study, including 13 physicians (interns), 14 emergency medical technicians, and 18 nurses. The intubation success rates in the first pass with BID, DL, and VL were 93.3%, 91.1%, and 97.8%, respectively (P=0.53). The intubation times to first ventilation with BID, DL, and VL were 13.15±6.16, 19.07±7.71, and 17.31±6.57 seconds, respectively (P<0.01). The proportions of dental injuries associated with BID, DL, and VL were 0% for physicians; 28.6%, 14.3%, and 0%, respectively for emergency medical technicians; and 27.8%, 11.1%, and 16.7%, respectively for nurses.
Conclusion
We performed a pilot study to test the usability of the new BID. There was no significant difference in intubation success rate in the first pass among BID, DL, and VL. The intubation time to first ventilation was shorter with the BID compared to DL and VL.
INTRODUCTION
Endotracheal intubation (ETI) is life-saving procedure for securing the airway [1]. Critically ill patients require ETI in various situations such as operating rooms (ORs), in-hospital general wards, intensive care units (ICUs), and emergency departments (EDs) [2]. Advancements in prehospital treatment have led to the implementation of ETI in out-of-hospital settings [3].
kill of prehospital healthcare providers are important for successful intubation [4]. To maintain certain success rates, more than 30 live ETI sessions are required for professionals to be skilled in the procedure [5]. However, it is difficult for prehospital healthcare providers to gain experience with live ETI, and the use of alternative supraglottic airway (SGA) devices like the laryngeal mask airway, Combitube (Tyco Healthcare Nellcor), and i-gel (Intersurgical) has increased [6]. The benefit of using SGAs instead of ETI has been questioned, and there are no definite guidelines for airway device selection in prehospital settings [7–9]. However, considering the human airway anatomy, ETI remains the gold standard for managing secretions and securing and facilitating optimal oxygenation and ventilation when conducted correctly [10].
Video laryngoscopy (VL), which is indirectly used to visualize the glottis and vocal cords, is a relatively recent and advanced intubation technology that has been widely used in the ICU and OR [11]. However, the success rate of VL is dependent on operator competency and the intubation environment, and its expense is high. Guyette et al. [12] reported that the use of VL by prehospital transport agencies did not reduce the number of intubation attempts or success rate associated with direct laryngoscopy (DL) performed by highly trained medical personnel. In another study, Nouruzi-Sedeh et al. [13] reported that VL success rate was greater than 90% compared with 51% for DL in the elective intubation of patients in the OR administered by untrained medical personnel. In hospital general ward settings, VL is reported to have a higher first-attempt success rate than DL, but the results were not significant in ICU or prehospital settings [11,12,14,15]. Even though VL has demonstrated better performance, it has a high cost, which has limited its widespread use, especially for prehospital ambulance services with a limited budget [15].
Because of the difficulty in learning and performing intubation and the high cost of VL for prehospital healthcare providers who are likely to encounter emergent airway cases, we developed a simple intubation device. The new blind intubation device (BID) was designed for blind intubation without the need to visualize the vocal cords. The purpose of this study was to test the usability of the newly developed BID compared with traditional DL and VL.
METHODS
Ethical statements
The study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (No. B-2007/622- 305). The participants provided written informed consent for the study using the Seoul National Bundang Hospital research consent form.
Design and function of the blind intubation device
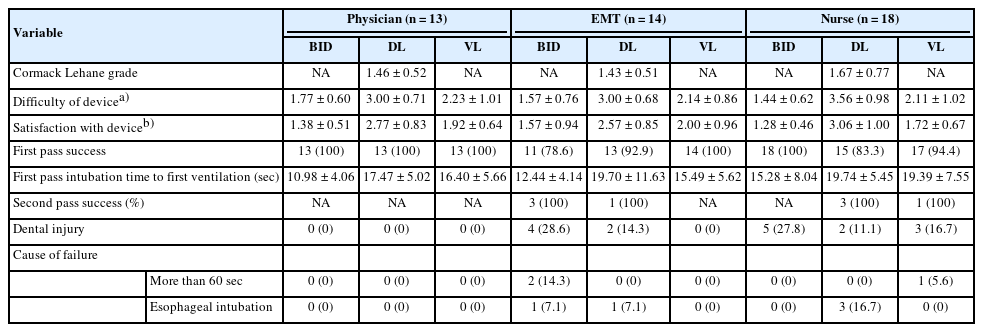
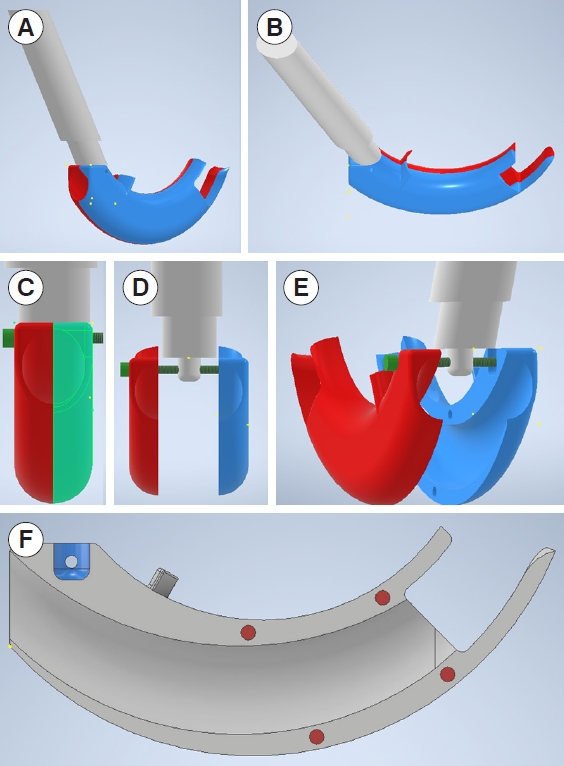
The BID (Fig. 1) was designed using the three-dimensional (3D) design program, Inventor 2020 (Autodesk). The BID consists of a handle and a body that are connected via a bolt at the end of the handle tip. There is an endotracheal tube (E-tube) insertion hole allowing the E-tube to pass through an epiglottis plate located above the glottis, an esophageal plate that prevents esophageal insertion, and an E-tube exit hole located in front of the vocal cords if placed correctly. Each body part has magnets to attach them into one device. The dental plate indicates the body insertion depth. Insertion of the BID body should stop when the dental plate touches the patient’s lower incisors. The design was printed using a 3D printer (Cubicon) and is constructed of polylactic acid (Fig. 2).
The design of the blind intubation device using Inventor 2020 (Autodesk). (A) Lateral view. (B) Superior view. (C) Posterior view. (D) Separated form. (E) Lateral view of separated form. (F) Cross-sectional view.
The components of the blind intubation device. The name of components viewed (A) from the side and (B) from the separated form. E-tube, endotracheal tube.
For ETI, the BID must be placed in the manikin airway (Fig. 3A). When the dental plate touches the lower incisor of the patient, the handle needs to be pulled back to avoid injuring the teeth (Fig. 3B). Intraoral status when the BID is placed correctly is illustrated in Fig. 3C. To insert the E-tube, the handle needs to be pushed along the direction of the red arrow to elevate the epiglottis and expose the vocal cords (Fig. 3D). The intraoral status when the handle is elevated along the direction of the red arrow is described in Fig. 3E. Compared to image in Fig. 3C, the epiglottis is elevated, the vocal cords are exposed, and the esophageal insertion prevention plate blocks the esophageal entrance (Fig. 3E). The E-tube is inserted into the BID E-tube insertion hole. The E-tube exit hole is located in front of the vocal cords, and advancement of the E-tube naturally results in ETI (Fig. 3F, G). After successful intubation is confirmed by end-tidal carbon dioxide (EtCO2) monitoring or lung auscultation, the handle and the body of the BID can be disassembled (Fig. 3H). The E-tube remains in the trachea after removal of the BID from the patient’s mouth (Fig. 3I).
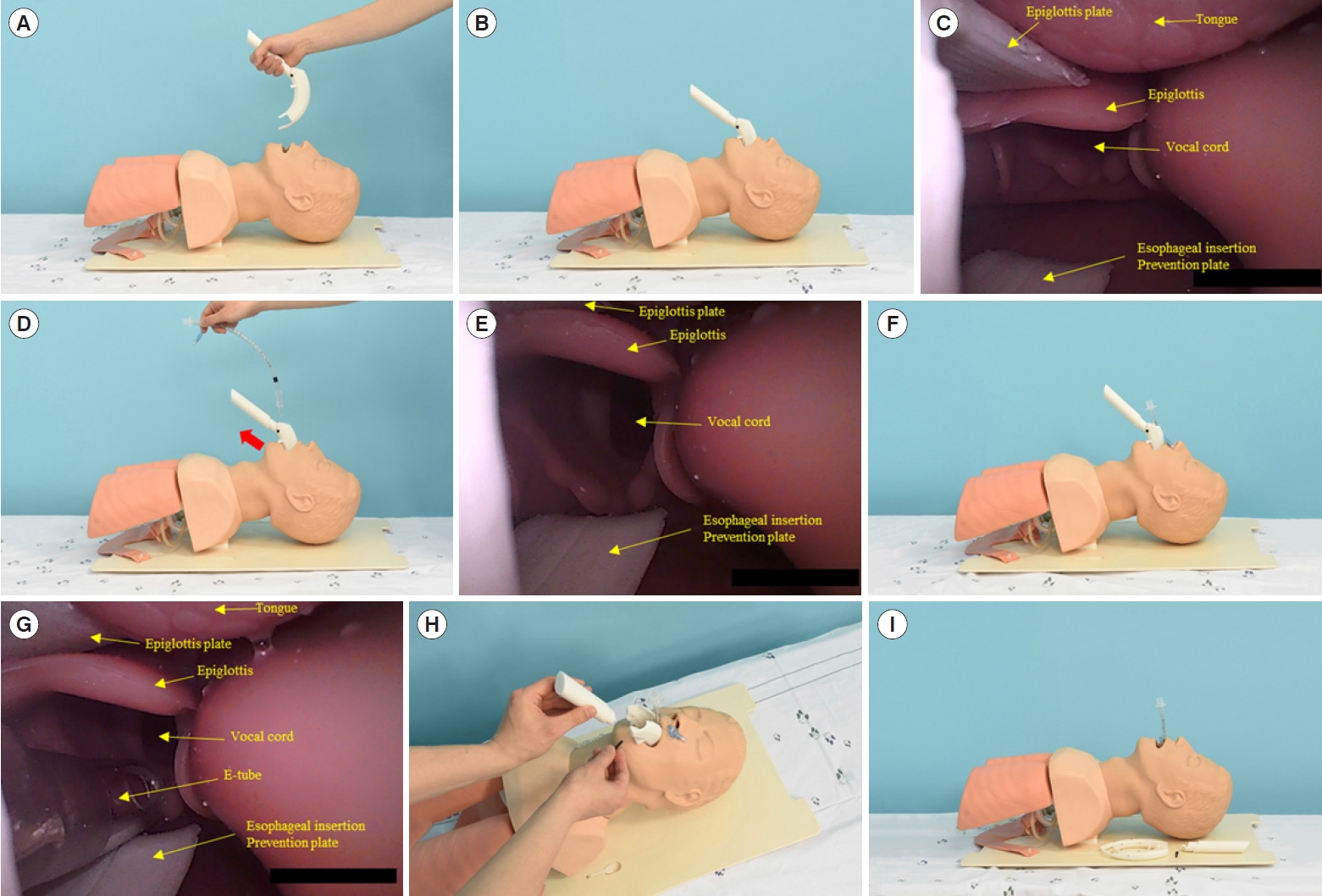
The way to perform endotracheal intubation using the blind intubation device (BID). (A) Initial placement of the BID. (B) Proper placement of the BID. (C) Intraoral status when the BID is properly placed. (D) Elevation of the epiglottis before inserting the endotracheal tube (E-tube). (E) Intraoral status when the epiglottis is elevated. (F) Proper placement of the E-tube through the BID. (G) Intraoral status when the E-tube passes the BID. (H) Removal of the BID after successful endotracheal intubation. (I) Lateral view after successful endotracheal intubation.
Study design
This randomized crossover simulation study used manikins to evaluate DL, VL, and BID performance. It was conducted between September and October 2020 at a tertiary teaching hospital with an annual ED volume of approximately 80,000 patients and 600 ETI cases in Gyeonggi Province, Korea.
Participants
The expected sample size was at least 12 participants for each group based on a previous study [16]. We finally determined a size of 40 participants based on a dropout rate of 10%. The participants were recruited from the ED using an intrahospital announcement bulletin board, and all provided written informed consent for the study. The participants included physicians, nurses, and emergency medical technicians (EMTs) aged between 18 and 60 years who had performed fewer than five live intubations. Participants were excluded if they did not consent to the study; had cardiac, neurological, or musculoskeletal disease; or were pregnant.
Study protocol
The researcher lectured all participants on DL, VL, and BID for approximately 30 minutes before simulation. The participants had 30 minutes of practice on a manikin with each device for familiarization with the ETI procedure. During the actual test, the participants were allowed two attempts using the manikin for each device. Macintosh DL was used with a fiber optic curved Mac 4 blade (Heine Optotechnik). The Glidescope GVL (Verathon Medical) was used for VL. A GlideRite stylet (Verathon Medical) was used for both DL and VL intubations. A cuffed polyvinyl chloride E-tube with an internal diameter of 7.5 mm was used for all intubation sessions. A Laerdal airway management trainer (Laerdal) was used as the intubation manikin, which was maintained in the supine position, and the sniffing position was allowed if the operator could not find the vocal cords.
The participants were randomly allocated to six groups based on the order of the intubation technique (Fig. 1): group 1 (DL-VL-BL), group 2 (DL-BL-VL), group 3 (VL-DL-BL), group 4 (VL-BL-DL), group 5 (BL-DL-VL), and group 6 (BL-VL-DL). Randomization was achieved by drawing lots using eight identical papers for each of the six groups.
After allocation, the participants conducted ETI using each device in sequential order. A single unblinded researcher (DKK) used a stopwatch to record the intubation time. The participants were blinded to the measurements. Intubation was defined as successful when the lungs of the manikin inflated well. Intubation was considered a failure if it took more than 60 seconds or esophageal intubation was confirmed. For the participants who failed during the first attempt, a second attempt was allowed. The participants had a 1-minute break after each intubation procedure. A dental injury was recorded if a click sound was generated from the upper incisors of the manikin. All intubation processes were performed in a normal stretcher car with a height of 90 cm.
All participants completed a brief questionnaire that was used to collect the following data: demographic data (age, sex, profession, working experience as healthcare provider), Cormack Lehane grade of the manikin, difficulty with ETI manipulation, and general satisfaction with each device [17]. The difficulty (range, 1 [very easy] to 5 [very difficult]) and general satisfaction (range, 1 [excellent] to 5 [very poor]) associated with each device were expressed on a 5-point Likert scale.
Exposure and outcome variables
The primary outcome was the success rate of intubation during the first attempt. The secondary outcome was intubation time to first ventilation in the first attempt. Intubation time to first ventilation was defined as the duration from the time the laryngoscopy blade of the DL or VL or the body of the BID passed the incisors of the manikin to the first ventilation with a bag-valve mask. The third outcome was dental injury rate.
Statistical analysis
Categorical variables are presented as counts and proportions and were compared using Fisher exact test. Continuous variables are presented as the median and interquartile range (IQR) or mean±standard deviation and were compared using the analysis of variance test. All analyses were performed using SAS ver. 9.4 (SAS Institute Inc). Statistical significance was set at P<0.05.
RESULTS
A total of 45 participants was recruited for the study. No participants were excluded. Participants were allocated to six groups, and a total of 135 intubations were performed, with 45 cases for each intubation device (Fig. 4).
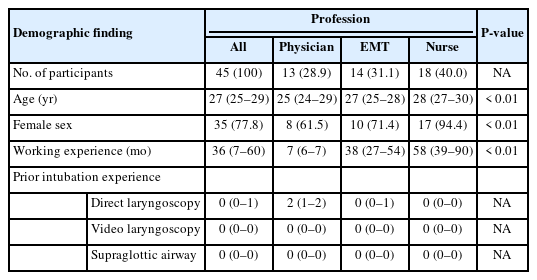
The median age of the participants was 27 years (IQR, 25–29 years). The number of female participants was 35 (77.8%). The numbers of physicians, EMTs, and nurses were 13 (28.9%), 14 (31.1%), and 18 (40.0%), respectively. The median working experience for the healthcare providers was 36 months (IQR, 7–60 months). The median number of previous intubation experiences was zero for DL, VL, and SGA, but the IQR was 0 to 1 for the DL group (Table 1).
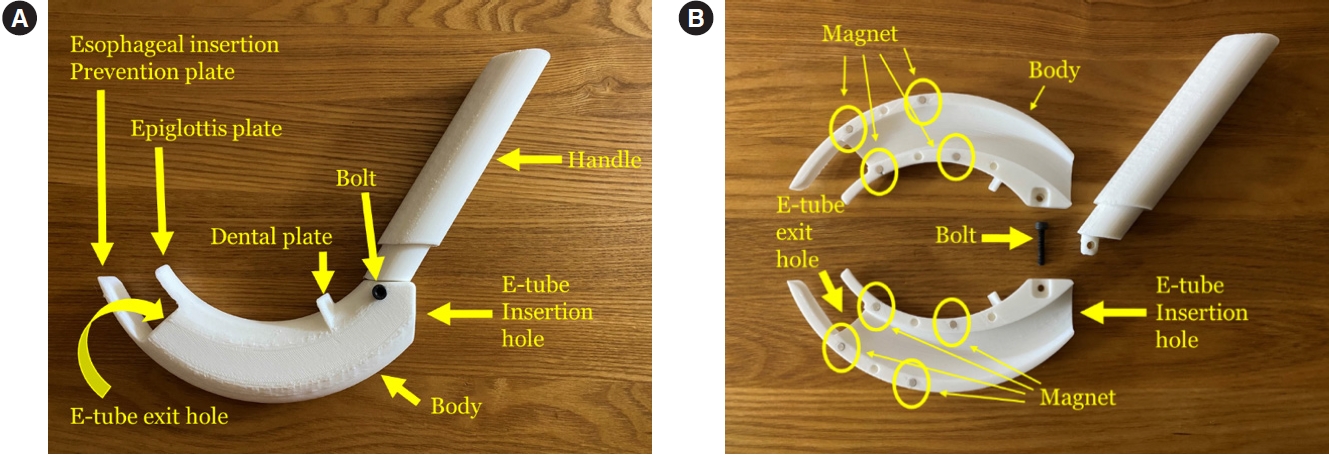
The mean Cormack Lehane grade of the intubation manikin rated by participants was 1.53±0.63. Intubation success rate for the first attempt in the BID, DL, and VL groups was 93.3%, 91.1%, and 97.8%, respectively (P=0.53). The mean intubation time to first ventilation in the first attempt was 13.15±6.16, 19.07±7.71, and 17.31±6.57 seconds for the BID, DL, and VL groups, respectively (P<0.01). The proportions of dental injuries in BID, DL, and VL were 20.0%, 8.9%, and 6.7%, respectively (P=0.17) (Table 2 and Fig. 5). For participants who failed in the first attempt, the intubation success rate for the second attempt was 100% for all groups. The number of intubation failures due to need for more than 60 seconds was two (4.4%) for BID, zero for DL, and one (2.2%) for VL. The number of esophageal intubations was one (2.2%) for BID, four (8.9%) for DL, and zero for VL. The mean difficulty associated with using each intubation device expressed on a 5-point Likert scale was 1.58±0.66 for BID, 3.22±0.85 for DL, and 2.16±0.95 for VL. The mean satisfaction for each intubation device expressed on a 5-point Likert scale was 1.40±0.65 for BID, 2.82±0.91 for DL, and 1.87±0.76 for VL (Table 2).

Comparison of outcomes of the intubation devices. Values on the bar represent means. (A) First pass intubation success rate. (B) Intubation time to first ventilation in first attempt. (C) Dental injury. BID, blind intubation device; DL, direct laryngoscopy; VL, video laryngoscopy.
Table 3 shows the subgroup comparisons by profession. The intubation success rates for BID, DL, and VL were all 100% for physicians; 78.6%, 92.9%, and 100%, respectively, for EMTs; and 100%, 83.3%, and 94.4%, respectively, for nurses. The mean intubation time to first ventilation in the first attempt for BID, DL, and VL was 10.98±4.06, 17.47±5.02, and 16.40±5.66 seconds, respectively, for physicians; 12.44±4.14, 19.70±11.63, and 15.49±5.62 seconds, respectively, for EMTs; and 15.28±8.04, 19.74±5.45, and 19.39±7.55 seconds, respectively, for nurses (Table 3). The proportions of dental injuries associated with BID, DL, and VL were all 0% for physicians; 28.6%, 14.3%, and 0%, respectively, for EMTs; and 27.8%, 11.1%, and 16.7%, respectively, for nurses (Table 3 and Fig. 6).
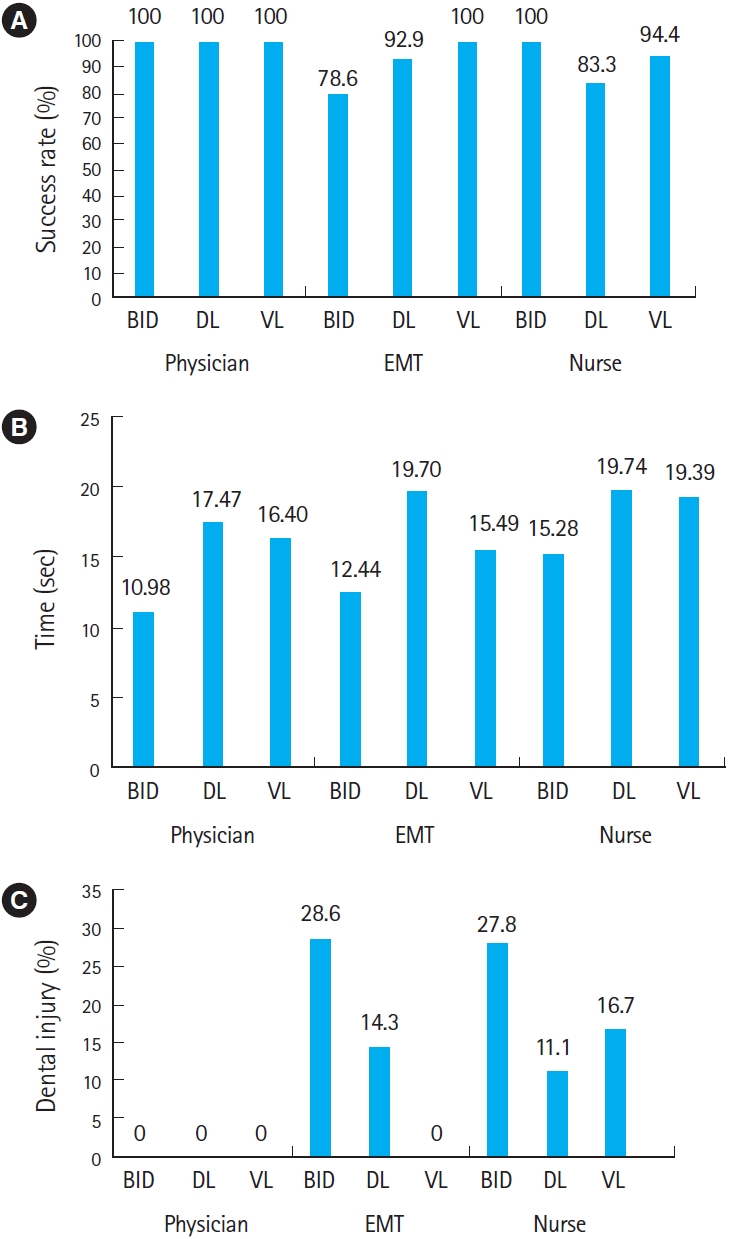
Subgroup comparison of the outcomes by profession: 13 physicians, 14 emergency medical technicians (EMTs), and 18 nurses. Values on the bar represent means. (A) First pass intubation success rate. (B) Intubation time to first ventilation in first trial. (C) Dental injury. BID, blind intubation device; DL, direct laryngoscopy; VL, video laryngoscopy.
DISCUSSION
A new intubation device was developed, and its usability was tested in this pilot study. The BID showed no significant difference in intubation success rate in the first attempt compared to DL or VL. The intubation time to first ventilation was shorter in the BID compared to DL or VL.
In existing SGAs, though the insertion process is easy, misplacement or esophageal insertion is frequent, resulting in inefficient ventilation. The BID mechanically prevented esophageal insertion by attaching an esophageal insertion prevention plate to the end of the body. Furthermore, for convenience of inexperienced operators, the insertion depth was marked with a dental plate to ensure an appropriate insertion depth and location inside the mouth. The epiglottic plate is designed to be placed under the glottis to elevate the epiglottis as in DL. The BID was designed to preoccupy the intraoral space where the E-tube is supposed to be inserted successfully, such that the operator can advance the E-tube according to the preoccupied intraoral space through the BID, resulting in endotracheal placement. In addition, the BID is disposable, reducing infection, and is operable without a battery.
The performance varied by intubation device. The intubation success rate was highest for VL and lowest for DL, although the difference was not statistically significant. Previous studies have reported different intubation outcomes stratified by profession and previous experience with airway management [12,13,18–20]. Although there was no statistical analysis for profession comparison, physicians showed the highest intubation success rate regardless of device. This result is consistent with those of previous studies showing that physicians had higher intubation success rates than nonphysicians [20]. Inexperienced doctors showed the highest success rate with the least working experience compared with other professions. In addition, physicians had more previous intubation experience than other professions. This may have been caused by differences in the education systems for the various professions. In contrast, nurses had the longest working experience with no previous intubation experience. The BID showed the lowest success rate in the EMT group and the highest success rate in the nurse group. The difference in BID outcomes stratified by profession implies that further research is required to determine the effect of previous education on the use of the device.
VL is a well-known intubation device with advanced technology [14]. However, considering the high cost of VL products, they can only be used in certain hospital settings, such as the OR, ICU, and ED, which limits their usefulness outside the hospital. The cost of VL and DL varies according to country and manufacturer, ranging from €1,120 to €5,600 for VL and $100 to $300 for DL, while the BID costs less than $100 [21]. For BID, the intubation time to first ventilation was shortest because it does not require a stylet for E-tube insertion. Although there was no statistical difference in dental injury, the BID showed the highest rate because the airway manikin did not have enough intraoral space due to the absent mandibular joint function. Further usability testing on an airway manikin with a mandible joint and prior education on BID handling are required to reduce the dental injury rate.
The difficulty and satisfaction associated with usage were highest for BID, because the BID could be used in the blind state and allowed faster intubation than DL and VL. For the failed cases of the DL and VL, the operators did not locate the vocal cords because the blade was inserted too deeply. One case of esophageal intubation was observed in the BID group. During the practice trial before the actual test, some participants could not find the vocal cords using the VL. Similar cases were observed with DL in practice trials. Despite the BID design to prevent esophageal intubation when performed correctly, esophageal intubation with the BID was problematic. Likewise for DL, the BID needs to be elevated against gravity to expose the vocal cords. Esophageal intubation with the BID may have occurred because of insufficient elevation of the glottis and inappropriate positioning of the device inside the mouth. Education on correct usage of the BID is required before use in further studies.
We included physicians, EMTs, and nurses as inexperienced participants because they are most likely to encounter patients with airway compromise in the clinical arena, and the purpose of the BID is to assist ETI by inexperienced operators. We included nurses in the study because in some emergency medical service systems, nurses participate as prehospital emergency medical service providers [22,23]. We found that short lectures and practice on airway manikins facilitated ETI with BID without previous intubation experience. The BID can be useful when VL cannot be performed due to expense and in prehospital ambulance or inhospital ward situations. Although the satisfaction, difficulty, and outcomes associated with BID were better than those associated with DL in this pilot study, the outcomes should be confirmed by further studies using a more exact sample size calculation. In further research, the BID needs to be compared with the SGAs because they have similar esophageal insertion prevention functions and are widely used in the prehospital setting.
This study has several limitations. First, it was a pilot simulation study. Because this device is new, there is no reference information for comparison of its function. Based on the results of this study, we can design appropriate studies for analysis and protocols for comparing BID feasibility with other airway devices. Second, this study was performed on an airway manikin, not on real human patients. Because of ethical problems trying new medical devices directly on humans, further studies on this new device are required for various airway manikins. Third, there were measurement errors in determining intubation duration during simulation due to measurement by a single unblinded researcher. Fourth, this study was repeated by the same operator, and the procedure performed immediately before could have influenced the procedure performed later. Further research is needed to separate the study population groups. Last, as there are several VL products available on the market, the use of only one may have biased the results.
The BID was developed, and its feasibility was tested on airway manikins. The BID showed a similar first intubation success rate and shorter intubation time to first ventilation compared with DL or VL. Further research with an accurate sample size calculation based on this pilot study is required.
SUPPLEMENTARY MATERIAL
Supplementary material is available at https://doi.org/10.15441/ceem.22.370.
Supplementary Material 1.
Questionnaire used for the participants.
Notes
CONFLICT OF INTEREST
Dae Kon Kim has applied for a patent for the device described in this study, and the result is pending. No other potential conflict of interest relevant to this article was reported.
FUNDING
This study was supported by a research grant funded by Seoul National University Bundang Hospital (No. 02-2019-038). The design of the study, data collection, analysis, and interpretation of research data were conducted by the authors.
AUTHOR CONTRIBUTIONS
Conceptualization: YJK; Data curation: JJ; Formal analysis: DKK; Funding acquisition: JJ; Investigation: DKK, SMP; Methodology: YJK, SMP; Project administration: DKK, JJ; Resources: DKK, JJ; Software: YJK; Supervision: YH Jo; Validation: SMP, YH Joo; Visualization: YH Jo; Writing–original draft: DKK; Writing–review & editing: YJK, JJ, YH Jo, YH Joo, SMP. All authors read and approved the final manuscript.
Acknowledgements
The authors thank Professor Jung Chan Lee (Department of Biomedical Engineering, Seoul National University College of Medicine, Seoul, Korea) for providing technical support for blind intubation device development. The authors also thank Associate Professor Dong Keon Lee (Department of Emergency Medicine, Seoul National University Bundang Hospital, Seongnam, Korea) for useful discussions.
References
Article information Continued
Notes
Capsule Summary
What is already known
Endotracheal intubation is life-saving procedure for securing the airway. The development of prehospital treatment has also led to the implementation of endotracheal intubation in out-of-hospital settings. However, it is difficult for prehospital healthcare providers to get enough opportunities to undertake live endotracheal intubation, and the use of alternative supraglottic airway devices like the laryngeal mask airway, Combitube, and i-gel has increased. However, considering the human airway anatomy, endotracheal intubation is still the gold standard for managing secretions, and securing and facilitating optimal oxygenation and ventilation when conducted correctly.
What is new in the current study
We developed a simple intubation device. The new intubation device is called the “blind intubation device (BID),” and it was designed for blind intubation through the patient’s vocal cord to facilitate endotracheal intubation instead of a supraglottic airway. The first pass success rate with the BID was similar to direct laryngoscopy and video laryngoscopy, and the time to ventilation was shortest with the BID.