AbstractObjectiveThis study aimed to evaluate the association between prehospital recognition of acute myocardial infarction (AMI) and length of stay (LOS) in the emergency department (ED) of emergency medical service (EMS)-transported AMI patients.
MethodsA multicenter retrospective observational study was conducted using prehospital and hospital data from three tertiary emergency departments. Patients diagnosed with AMI between January 2015 and December 2018 were enrolled. Study groups were categorized according to prehospital recognition and prehospital 12-lead electrocardiography (ECG) into three groups based on an EMS cardiovascular registry: group A, no prehospital recognition (reference group); group B, prehospital recognition without 12-lead ECG; and group C, prehospital recognition with 12-lead ECG. The primary outcome was an ED LOS of less than 4 hours.
ResultsAmong 1,237 study participants, 722 (58.4%) were in group A, 325 (26.3%) were in group B, and 190 (15.4%) were in group C. Multivariable logistic regression showed that groups B and C had a higher likelihood of a short ED LOS (adjusted odds ratio [95% confidence interval]: group B, 1.64 [1.21–2.22] and group C, 1.88 [1.30–2.71]) than group A. There was no significant difference in ED LOS according to whether prehospital 12-lead ECG was conducted.
INTRODUCTIONAcute myocardial infarction (AMI), including both ST elevation myocardial infarction (STEMI) and non-STEMI, is a common cardiac emergency condition and is associated with a high risk of serious morbidities and mortality [1]. Although the incidence of AMI has decreased significantly in recent decades [2], AMI is still a major global health burden, with AMI associated with an increased number of years with disability [3]. In Korea, AMI is the second leading cause of death, with 60 deaths due to AMI among every 100,000 people [4]. AMI has also been demonstrated to have a high economic cost [5].
Shortening the time delay in diagnosis and treatment of AMI is crucial for achieving optimal clinical outcomes [6,7]. The American College of Cardiology and American Heart Association proposed an ideal time window for intervention in STEMI patients [8], and recommended that suspected AMI patients receive emergency medical service (EMS) to shorten the time delay [9]. The length of stay (LOS) in the emergency department (ED), as an index of time delay, was found to be associated with clinical outcomes in time-sensitive conditions, including AMI [10,11]. ED routine issues, including diagnostic difficulties, have been demonstrated to contribute to in-hospital delays [12].
EMS management of AMI is important because early assessment, treatment, and expedited communication with the receiving hospital are associated with improved patient outcomes [13]. The ED bypass program based on early recognition of AMI by EMS was demonstrated to have a significant association with survival outcome in a STEMI cohort [14]. Additionally, Bright et al. [15] reported high accuracy among EMS personnel in the prehospital diagnosis of AMI. Prehospital 12-lead electrocardiography (ECG) by EMS personnel is strongly recommended and implemented worldwide [16]. Hutchison et al. [17] reported that the time to intervention was greatly decreased with clinical pathway activation based on prehospital 12-lead ECG findings. Prehospital 12-lead ECG was also found to help the ED achieve the ideal time window for intervention and was therefore associated with a lower mortality rate in AMI patients [18].
The effect of prehospital recognition on the ED process has not been well evaluated for patients with AMI. We hypothesized that prehospital recognition of AMI would reduce the ED LOS and that prehospital 12-lead ECG would strengthen this association. The purpose of this study was therefore to evaluate the association between prehospital recognition with or without 12-lead ECG and ED LOS in EMS-transported AMI patients.
METHODSEthical statementsThis study complies with the Declaration of Helsinki, and its protocol was approved by the Institutional Review Board of Seoul National University Hospital (No. 2006-004-1128). The Institutional Review Board waived the requirement for informed consent due to the retrospective nature of the study.
Study design and data sourceThis study was a cross-sectional, retrospective, observational study based on an integrated database including data from three academic tertiary emergency departments from January 2015 to December 2018. Data were obtained from three sources: EMS ambulance run-sheets, EMS cardiovascular registry, and hospital administrative databases. EMS time variables, chief complaints, and vital signs measured at the scene are collected by EMS personnel on an EMS run-sheet for all EMS-transported patients. The EMS cardiovascular registry contains information about past medical history, prehospital sublingual nitroglycerine administration, 12-lead ECG at the scene, prenotification of the receiving hospital, and presumed acute cardiovascular disease for highly suspicious cases. Hospital administrative databases contain information about the clinical course, including the time of visit, physiologic status at triage, diagnosis at the ED or hospital discharge, time of admission or discharge, and status at discharge. We integrated data from the three sources using a common deidentified key to produce a comprehensive clinical dataset.
Study settingThe Korean EMS, which is a public health service, is operated by the National Fire Agency and includes 17 provincial headquarters with approximately 200 fire stations, 1,000 EMS agencies, and 8,400 EMS personnel. Ambulances assigned to regional EMS agencies are dispatched for emergency calls. Korean EMS personnel have certification levels ranging from basic to intermediate, including intravenous fluid administration and advanced airway management under direct medical oversight by doctors. A 6-month curriculum is provided to all EMS providers at the Fire Service Academy, with a minimum of 1 month of first aid practice including 12-lead ECG interpretation in the field. Act 119 regarding the rescue and EMS mandates that patient information be input into structured sheets (EMS run-sheets) by EMS personnel immediately after transportation [19]. An additional cardiovascular registry needs to be filled out if a patient complains of chest pain, respiratory difficulty, or syncope, or if acute cardiovascular disease is suspected by EMS personnel. EMS personnel are instructed to perform 12-lead ECG if an ECG device is available, and the patient is suspected of having acute cardiovascular disease and to transport the patient to the nearest at least level 2 ED. Sublingual nitroglycerin can be attempted at most three times per 5-minute intervals under direct medical oversight if no contraindications are present.
In Korea, EDs are categorized into three levels by the Ministry of Health and Welfare: level 1 EDs (n=36), where 24/7 emergency care for critically ill emergency patients is provided by emergency physicians; level 2 EDs (n=119), where emergency physicians provide high-acuity emergency care for emergency patients; and level 3 EDs (n=261), where general physicians provide lowacuity emergency care for patients. All EDs in Korea undergo an annual nationwide functional performance evaluation by the Ministry of Health and Welfare. Level 1 and 2 EDs have a cardiology intervention team, which is headed by an emergency physician, and general acute cardiac care is performed following international standard guidelines. Emergency physicians are responsible for making critical decisions for patient care [20,21].
After EMS personnel deliver on-scene clinical information to the triage nurse at the entrance of the ED, all patients are assessed and categorized into one of five levels according to the urgency of emergency medical care. Patients suspected of AMI undergo urgent ECG, and the emergency physician can directly notify the on-call intervention team regarding suspected STEMI (STEMI critical pathway). Otherwise, after full evaluation, including cardiac biomarker tests, an assigned emergency physician will consult an on-duty cardiologist regarding hospitalization. Since ED care performance for AMI patients is evaluated by the government, reducing the ED LOS is strongly recommended.
Study populationEMS-assessed and transported adult nontraumatic AMI patients seen from January 2015 to December 2018 who were admitted following their ED visit were enrolled. We excluded patients transported between hospitals, patients with cardiac arrest, discharged patients, and patients with missing outcomes. Patients were identified according to International Statistical Classification of Diseases 10th Revision (ICD-10) diagnostic codes of I-210 and I-219, which indicate AMI. The ED administrative database has two types of primary diagnostic codes: the final diagnostic codes at ED discharge and at hospital discharge. A patient was considered positive for AMI if a confirmative diagnostic code was found at any point in the discharge record. Coronary angiography reports were not taken into consideration to confirm diagnosis, as the goal of this study was to evaluate the association between prehospital recognition of AMI and ED LOS.
Outcome measuresThe primary outcome was the ED LOS, defined as the time interval from ED arrival to ED departure due to admission to the floor; this was collected from the hospital administrative database. Four hours was defined as a short ED LOS as this time interval has been used as the target in previous studies [22,23]. Inpatient (IP) LOS, which is a clinical outcome indicator [24], was used as the secondary outcome, and the median value was selected for reference. Survival to discharge, which was evaluated at the point of hospital discharge and collected from the administrative database, was additionally used as the tertiary outcome.
Variables and measurementsThe main exposures were prehospital recognition of acute cardiovascular disease by EMS personnel (prehospital recognition) and prehospital 12-lead ECG. Prehospital recognition was defined as positive if EMS personnel entered the patient with presumed acute cardiovascular disease into the cardiovascular registry. Whether 12-lead ECG was conducted at the scene was assessed in the same way. The study population was categorized into three groups: group A, no prehospital recognition (reference group); group B, prehospital recognition without 12-lead ECG; and group C, prehospital recognition with prehospital 12-lead ECG.
The following demographic and clinical data were collected and categorized: age (under 49, 50–59, 60–69, 70–79, and over 80 years old), sex, ED visit time (morning, evening, or night), weekend presentation, season of the ED visit, chief complaint (chest pain, atypical coronary symptoms, including dyspnea, syncope, palpitation, epigastric pain, and chest burning), past heart disease history, prehospital shock status (systolic blood pressure under 90 mmHg), prehospital abnormal heart rate (heart rate over 100 beats/min and under 60 beats/min), prehospital alertness, ST-segment abnormality in prehospital 12-lead ECG, prehospital sublingual nitroglycerin administration, receiving hospital notification before ED arrival, shock status at ED triage, abnormal heart rate at ED triage, direct transport to the angiography room with confirmation of ST-segment elevation in the initial ECG examination (STEMI critical pathway), and intensive care unit (ICU) admission (including coronary unit). Median imputation was conducted for missing values for age and vital signs, which occurred in less than 20% of the study population.
Statistical analysisA descriptive analysis was performed to analyze the distributions of the demographic and clinical data of the study population. Chi-squared tests for categorical variables and Wilcoxon rank-sum tests for continuous variables were used. To determine the associations between prehospital recognition with and without 12-lead ECG and outcomes, adjusted odds ratios (AORs) with 95% confidence intervals (CIs) were calculated using a multivariable logistic regression analysis with group A as the reference. We adjusted for age group, sex, past medical history of heart disease, chief complaint of chest pain and atypical coronary symptoms, prehospital shock, prehospital alertness, and time, weekend, and season of the ED visit. To determine the effectiveness of 12-lead ECG on prehospital recognition, AORs and 95% CIs were recalculated with the aforementioned regression model with group B as a reference.
To evaluate changes in effect size according to the characteristics of the patients, sensitivity analyses were performed. Since one of the main variables affecting ED LOS is severity, the subgroup of patients admitted to the ICU was extracted, and the same statistical analyses were performed. We also conducted additional subgroup analysis for non-STEMI patients considering that the STEMI critical pathway could significantly affect the results. All statistical analyses were performed using SAS ver. 9.4 (SAS Institute Inc., Cary, NC, USA).
RESULTSDemographic findingsAmong 4,988 patients diagnosed with AMI from January 2015 to December 2018, 1,237 patients were included in the final analysis. We excluded 22 injured patients, five pediatric patients, 388 patients with symptoms occurring for more than a week, 3,114 non-EMS users, 87 patients transported between hospitals, 89 patients with out-of-hospital and in-hospital cardiac arrest, and 56 patients with no outcome data at discharge (Fig. 1).
Table 1 presents demographic and clinical data according to study group. Patients in group C were more likely to be male and less likely to visit the ED at night (11 PM–7 AM) or in the summer. Patients in group A had lower proportions of typical coronary symptoms, past medical history of heart disease, prehospital alertness, prehospital sublingual nitroglycerin administration, and prenotification of the receiving hospital. Group A had a lower proportion of STEMI critical pathway patients than groups B and C: 12.0% in group A, 25.2% in group B, and 29.5% in group C. The main outcomes showed significant differences according to study group: the percentages of patients with a short ED LOS and short IP LOS were 41.7% and 40.0% in group A, 57.8% and 52.3% in group B, and 60.5% and 58.4% in group C, respectively (Table 1).
Main analysisIn multivariable logistic regression analysis, statistically significant differences in ED LOS were found for groups B and C compared to group A (ED LOS less than 4 hours, AOR [95% CI]: 1.64 [1.21–2.22] in group B and 1.88 [1.30–2.71] in group C). There was no significant difference in IP LOS or survival to discharge (IP LOS less than 4 days, AOR [95% CI]: 1.02 [0.75–1.37] in group B and 1.25 [0.87–1.79] in group C; survival to discharge, AOR [95% CI]: 1.14 (0.60–2.14) in group B and 1.20 [0.55–2.62] in group C) (Table 2). In multivariable linear regression analysis for ED LOS, the coefficient for regression of the study group (reference, group A) was calculated to be -1.782 (P<0.01).
In sensitivity analysis for patients admitted to the ICU, similar and statistically significant associations were found (ED LOS less than 4 hours, AOR [95% CI]: 1.85 [1.15–2.97] in group B and 1.77 [1.02–3.06] in group C) (Table 3). A similar trend was demonstrated for non-STEMI patients (ED LOS less than 4 hours, AOR [95% CI]: 1.46 [1.03–2.06] in group B and 1.55 [1.02–2.37] in group C) (Table 4).
DISCUSSIONIn EMS-transported AMI patients admitted to the ED, prehospital recognition was found to be associated with a short ED LOS. There was no statistically significant difference according to prehospital 12-lead ECG. IP LOS and survival to discharge had no significant association with prehospital recognition with or without 12-lead ECG. The same trends were sustained and statistically significant in patients admitted to the ICU and in non-STEMI patients. Careful prehospital evaluation for AMI by EMS personnel should be emphasized to improve the clinical course of these patients.
Prehospital recognition of AMI is associated with a higher probability of notification of the receiving hospital. This should ideally result in activation of the AMI practice process in the hospital, which could shorten ED LOS. We found that there were more AMI patients with a short ED LOS (under 4 hours) when the hospital received notification of an AMI during the prehospital phase, even after excluding STEMI cases, then when no prenotification was received (42.1% vs 35.0%, respectively).
In the prehospital phase of AMI, patients present with more pronounced symptoms, and recognition of these symptoms can optimize patient assessment and triage [25]. With sufficient experience and focused education, EMS personnel can identify highrisk features that indicate the possibility of acute cardiovascular disease [26]. A detailed history taken at the scene can provide meaningful information to ED staff, who can use this information to direct the assessments performed, thus accelerating the clinical process. However, the delivery of misleading information may interfere with the direction of the assessments performed and thus the clinical course of the patient. Considering that communication barriers extend ED LOS, the first impression of EMS personnel can influence ED staff [27].
Additionally, the presence or absence of a sublingual nitroglycerin effect on chest pain is an important diagnostic predictor [28]. EMS personnel can evaluate this effect more clearly at the scene when chest pain has not yet subsided, as chest pain often improves spontaneously and changes to ambiguous symptoms at ED arrival. In such situations, ED LOS can be prolonged, as the application of proper diagnostic algorithms to reach the right diagnosis is limited [29]. In the prehospital recognition group, the number of sublingual nitroglycerin administrations was seven to eight times higher than in the other groups (Table 1).
In this study, prehospital recognition of AMI by EMS personnel was documented in the official registry. There is no detailed protocol about when EMS personnel should consider the patient to have suspected acute cardiovascular disease, but typical questions should be asked to complete the cardiovascular registry questions, such as the location and intensity of pain, whether the pain is radiating, and aggravating and relieving factors. The National Fire Agency provides a routine continuing education course for EMS personnel, including information on the presentations of acute critical illnesses such as AMI. EMS personnel are likely able to differentiate the possibility of AMI on the basis of complaints, past medical history, and vital signs. Sixty percent of the total patients had chest pain, but 40% of them were not recognized as having acute cardiovascular disease (Table 1), so we hypothesize that unmeasured factors affected EMS personnel assessments. Recognition of the overlooked AMI population is crucial to improve the clinical process.
ED LOS has been considered an indicator of the ED care process in previous studies [30-32]. Unlike cardiac arrest or trauma, in which prehospital resuscitation determines the status of patients at the ED entrance level, the role of EMS personnel in STEMI usually focuses on 12-lead electrocardiogram interpretation and ED bypass [8]. Considering that overcrowding and limited resources are major challenges to ED AMI diagnostic performance [33], detailed and accurate prehospital assessments are helpful from the beginning of ED care. Additionally, prenotification of receiving hospitals affects the ED care process. In the study group with prehospital recognition, a higher proportion of the patients’ hospitals were notified before ED arrival, even when no 12-lead ECG results were available.
Condition severity has been demonstrated to be associated with ED LOS [34]. Sensitivity analysis of patients admitted to the ICU was performed to correct for unmeasured biases, such as a delay in admission based on nonmedical issues. Similar trends with statistical significance were found regarding the outcomes of patients admitted to the ICU and non-STEMI patients. Therefore, we highly recommend that EMS personnel assess the probability of AMI at the scene, especially in patients with indications of high condition severity, even without evidence of STEMI.
Our results indicate that prehospital EMS assessment could be beneficial for the ED care process, but the effect of prehospital recognition on shortening ED LOS is not clear. The effects of implementation of more sensitive EMS tools to screen patients with suspected AMI and analyses of the effects of these tools on the ED care process are needed. Considering that over half of AMIs were not recognized at the prehospital level, the creation and use of advanced patient-assessment protocols at the scene could have clinical benefits.
This study had several limitations. First, prehospital recognition was dependent on individual experience or competency. There was no standardized EMS protocol to evaluate patients with suspected AMI based on the patient’s history, which is a significant limitation. Second, we could not confirm whether prehospital information was actually delivered to ED physicians. Although ED triage nurses write a triage note containing information provided by EMS personnel, it is entirely up to the physician as to whether they refer to this note or not. Next, information on the time of diagnosis, time to first 12-lead ECG at the ED, or time to consult cardiologist would provide more accurate information on the effect of prehospital recognition, but this information was not available in the databases. As ED LOS is a surrogate marker, we adjusted for factors affecting the ED LOS as much as possible. However, there were also unadjusted confounders such as administrative delays and preparation time in the ward or ICU. We included time and season of ED visit in the main analysis to adjust for variation, but variation remains a significant limitation of the study. However, when further sensitivity analysis excluding extremely delayed cases (10, 12, and 15 hours) was conducted, we observed the same trends (Supplementary Table 1.). Fourth, even though chief complaints and vital signs were adjusted for, detailed condition severity or characteristics were not analyzed. Generally, the ED LOS of patients with minor AMI or late presenters is prolonged due to ambiguous histories. Furthermore, we could not evaluate this association in the STEMI cohort as the majority of these patients stayed in the ED for less than 4 hours. We hypothesized that shortening of ED LOS would affect the treatment outcomes of AMI, which would shorten IP LOS and increase survival. There was no significant association between prehospital recognition and IP LOS and survival, suggesting that a delay in the ED might be tolerated in non-severe patients. Fifth, individual variations in practice could affect the results, such as physicians who always check for cardiovascular disease, cardiologists who respond quickly, and physicians who tend to skip performing laboratory tests in patients without certain needs. Compliance with hospitalization may also have affected our findings. Since the design of this study was observational, unmeasured biases may have been present. Last, the results of this study cannot be generalized because this study was conducted using data from three academic tertiary emergency departments and a basic-to-intermediate service level EMS system.
In summary, prehospital recognition of AMI by EMS personnel was found to be associated with a short ED LOS in EMS-transported AMI patients. Focused assessment at the scene can improve the clinical outcomes of AMI patients by decreasing their ED LOS.
SUPPLEMENTARY MATERIALSupplementary Table 1.Multivariable logistic regression by prehospital recognition with or without 12-lead electrocardiography excluding the extremely delayed cases Supplementary materials are available at http://doi.org/10.15441/ceem.22.330.
NOTESAUTHOR CONTRIBUTIONS
Conceptualization: SRS, KHK; Data curation: KJS, SDS; Formal analysis: SRS, KHK; Investigation: SRS, KHK; Methodology: JHP, KHK; Project administration: KJS, SDS; Resources: KJS, SDS; Software: SRS, KHK; Supervision: JHP; Validation: JHP; Visualization: SRS, KHK; Writing–original draft: SRS, KHK; Writing–review & editing: all authors. All authors read and approved the final manuscript.
REFERENCES2. Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med 2010; 362:2155-65.
3. Moran AE, Forouzanfar MH, Roth GA, et al. The global burden of ischemic heart disease in 1990 and 2010: the global burden of disease 2010 study. Circulation 2014; 129:1493-501.
4. Stiell IG, Wells GA, Field BJ, et al. Improved out-of-hospital cardiac arrest survival through the inexpensive optimization of an existing defibrillation program: OPALS study phase II. JAMA 1999; 281:1175-81.
5. Weintraub WS, Daniels SR, Burke LE, et al. Value of primordial and primary prevention for cardiovascular disease: a policy statement from the American Heart Association. Circulation 2011; 124:967-90.
6. Canto JG, Zalenski RJ, Ornato JP, et al. Use of emergency medical services in acute myocardial infarction and subsequent quality of care: observations from the national registry of myocardial infarction 2. Circulation 2002; 106:3018-23.
7. Hata N, Kobayashi N, Imaizumi T, et al. Use of an air ambulance system improves time to treatment of patients with acute myocardial infarction. Intern Med 2006; 45:45-50.
8. Fosbol EL, Granger CB, Jollis JG, et al. The impact of a statewide pre-hospital STEMI strategy to bypass hospitals without percutaneous coronary intervention capability on treatment times. Circulation 2013; 127:604-12.
9. Levine GN, Bates ER, Blankenship JC, et al. 2015 ACC/AHA/ SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction: an update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention and the 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation 2016; 133:1135-47.
10. Minaeian A, Patel A, Essa B, Goddeau RP Jr, Moonis M, Henninger N. Emergency department length of stay and outcome after ischemic stroke. J Stroke Cerebrovasc Dis 2017; 26:2167-73.
11. Cowan RM, Trzeciak S. Clinical review: emergency department overcrowding and the potential impact on the critically ill. Crit Care 2005; 9:291-5.
12. Hirvonen TP, Halinen MO, Kala RA, Olkinuora JT. Delays in thrombolytic therapy for acute myocardial infarction in Finland: results of a national thrombolytic therapy delay study. Eur Heart J 1998; 19:885-92.
13. Mathews R, Peterson ED, Li S, et al. Use of emergency medical service transport among patients with ST-segment-elevation myocardial infarction: findings from the National Cardiovascular Data Registry Acute Coronary Treatment Intervention Outcomes Network Registry-Get With the Guidelines. Circulation 2011; 124:154-63.
14. Bang A, Grip L, Herlitz J, et al. Lower mortality after prehospital recognition and treatment followed by fast tracking to coronary care compared with admittance via emergency department in patients with ST-elevation myocardial infarction. Int J Cardiol 2008; 129:325-32.
16. Nam J, Caners K, Bowen JM, Welsford M, O’Reilly D. Systematic review and meta-analysis of the benefits of out-of-hospital 12-lead ECG and advance notification in ST-segment elevation myocardial infarction patients. Ann Emerg Med 2014; 64:176-86.
17. Hutchison AW, Malaiapan Y, Jarvie I, et al. Prehospital 12-lead ECG to triage ST-elevation myocardial infarction and emergency department activation of the infarct team significantly improves door-to-balloon times: ambulance Victoria and MonashHEART acute myocardial infarction (MonAMI) 12-lead ECG project. Circ Cardiovasc Interv 2009; 2:528-34.
18. Quinn T, Johnsen S, Gale CP, et al. Effects of prehospital 12- lead ECG on processes of care and mortality in acute coronary syndrome: a linked cohort study from the Myocardial Ischaemia National Audit Project. Heart 2014; 100:944-50.
19. Derlet RW, Richards JR. Emergency department overcrowding in Florida, New York, and Texas. South Med J 2002; 95:846-9.
20. Jeong J, Ro YS, Shin SD, Song KJ, Hong KJ, Ahn KO. Association of time from arrest to percutaneous coronary intervention with survival outcomes after out-of-hospital cardiac arrest. Resuscitation 2017; 115:148-54.
21. Kim MJ, Ro YS, Shin SD, et al. Association of emergent and elective percutaneous coronary intervention with neurological outcome and survival after out-of-hospital cardiac arrest in patients with and without a history of heart disease. Resuscitation 2015; 97:115-21.
22. Jones P, Schimanski K. The four hour target to reduce emergency department ‘waiting time’: a systematic review of clinical outcomes. Emerg Med Australas 2010; 22:391-8.
23. Liew D, Liew D, Kennedy MP. Emergency department length of stay independently predicts excess inpatient length of stay. Med J Aust 2003; 179:524-6.
24. Williams T, Savage L, Whitehead N, et al. Missed acute myocardial infarction (MAMI) in a rural and regional setting. Int J Cardiol Heart Vasc 2019; 22:177-80.
25. Stengaard C, Sorensen JT, Rasmussen MB, Botker MT, Pedersen CK, Terkelsen CJ. Prehospital diagnosis of patients with acute myocardial infarction. Diagnosis (Berl) 2016; 3:155-66.
26. Koganti S, Patel N, Seraphim A, Kotecha T, Whitbread M, Rakhit RD. Reducing time to angiography and hospital stay for patients with high-risk non-ST-elevation acute coronary syndrome: retrospective analysis of a paramedic-activated direct access pathway. BMJ Open 2016; 6:e010428.
27. Grubbs V, Bibbins-Domingo K, Fernandez A, Chattopadhyay A, Bindman AB. Acute myocardial infarction length of stay and hospital mortality are not associated with language preference. J Gen Intern Med 2008; 23:190-4.
28. Ferreira JC, Mochly-Rosen D. Nitroglycerin use in myocardial infarction patients. Circ J 2012; 76:15-21.
29. Rubini Gimenez M, Reiter M, Twerenbold R, et al. Sex-specific chest pain characteristics in the early diagnosis of acute myocardial infarction. JAMA Intern Med 2014; 174:241-9.
30. Chiu IM, Lin YR, Syue YJ, Kung CT, Wu KH, Li CJ. The influence of crowding on clinical practice in the emergency department. Am J Emerg Med 2018; 36:56-60.
31. Morais Oliveira M, Marti C, Ramlawi M, et al. Impact of a patient-flow physician coordinator on waiting times and length of stay in an emergency department: a before-after cohort study. PLoS One 2018; 13:e0209035.
32. Alishahi Tabriz A, Trogdon JG, Fried BJ. Association between adopting emergency department crowding interventions and emergency departments’ core performance measures. Am J Emerg Med 2020; 38:258-65.
Fig. 1.Patient flow. AMI, acute myocardial infarction; EMS, emergency medical service; OHCA, out-of-hospital cardiac arrest; DNR, do not resuscitate; IHCA, in-hospital cardiac arrest; ED, emergency department; ECG, electrocardiography. 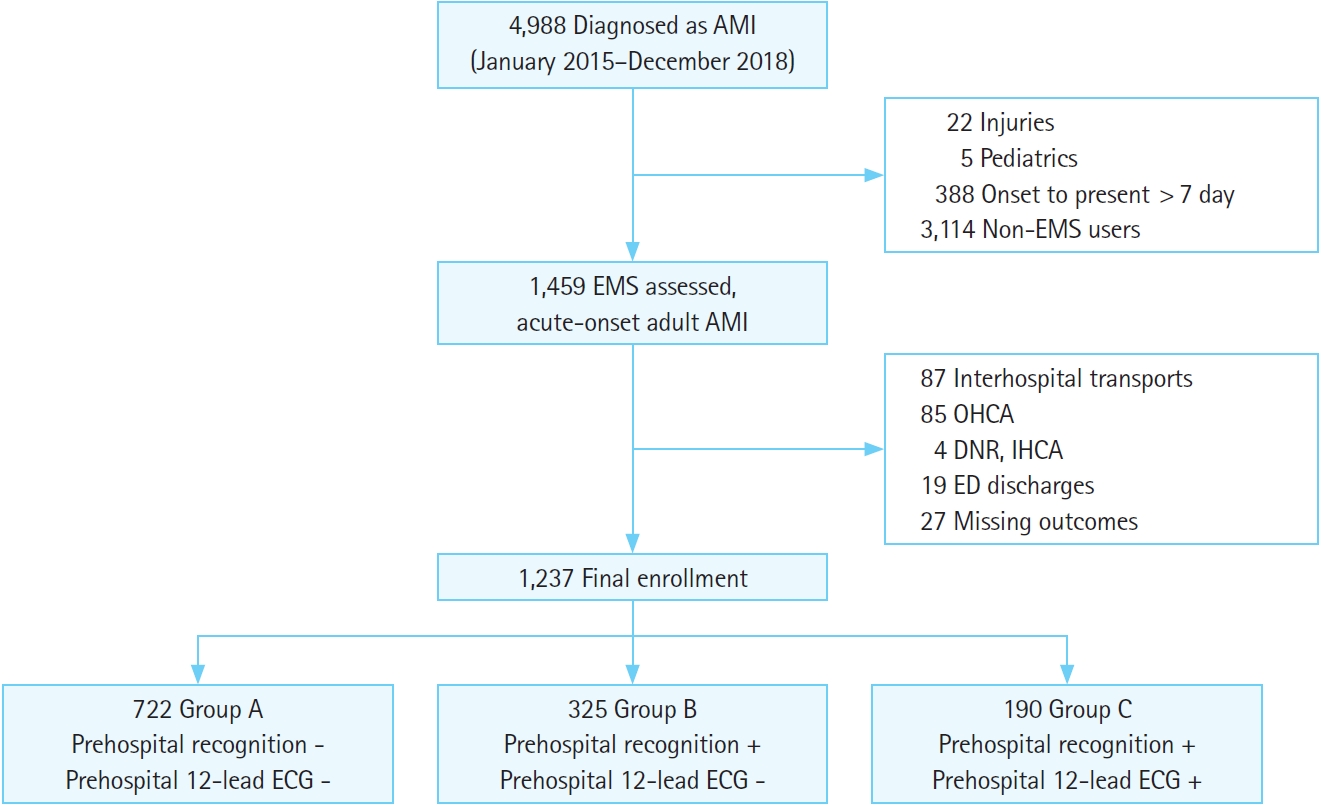
Table 1.Demographics and clinical findings according to study group Table 2.Univariable and multivariable logistic regression by prehospital recognition with or without 12-lead electrocardiography
The number of patients for groups A, B, and C were 722, 325, and 190, respectively. The multivariable model was adjusted for age group, sex, past heart disease history, chief complaint, prehospital shock, prehospital alertness, time of visit, weekend, and season. OR, odds ratio; CI, confidence interval; ED, emergency department; LOS, length of stay; NA, not applicable. Table 3.Univariable and multivariable logistic regression by prehospital recognition with or without 12-lead electrocardiography in patients admitted to the intensive care unit
The number of patients for groups A, B, and C were 288, 151, and 103, respectively. The multivariable model was adjusted for age group, sex, past heart disease history, chief complaint, prehospital shock, prehospital alertness, time of visit, weekend, and season. OR, odds ratio; CI, confidence interval; ED, emergency department; LOS, length of stay; NA, not applicable. Table 4.Univariable and multivariable logistic regression by prehospital recognition with or without 12-lead electrocardiography in non-ST-elevation myocardial infarction patients
The number of patients for groups A, B, and C were 635, 243, and 134, respectively. The multivariable model was adjusted for age group, sex, past heart disease history, chief complaint, prehospital shock, prehospital alertness, time of visit, weekend, and season. OR, odds ratio; CI, confidence interval; ED, emergency department; LOS, length of stay; NA, not applicable. |
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||